Mastocytosis is associated with an activating mutation in the KIT oncoprotein (KITD816V) that results in autophosphorylation of the KIT receptor in a ligand-independent manner. This mutation is inherently resistant to imatinib and, to date, there remains no effective curative therapy for systemic mastocytosis associated with KITD816V. Dasatinib (BMS-354825) is a novel orally bioavailable SRC/ABL inhibitor that has activity against multiple imatinib-resistant BCR-ABL isoforms in vitro that is presently showing considerable promise in early-phase clinical trials of chronic myeloid leukemia (CML). Pharmacokinetic analysis suggests that high nanomolar concentrations of dasatinib can be achieved safely in humans. In this study, we demonstrate significant inhibitory activity of dasatinib against both wild-type KIT and the KITD816V mutation in the nanomolar range in in vitro and cell-based kinase assays. Additionally, dasatinib leads to growth inhibition of a KITD816V-harboring human masto-cytosis cell line. Significantly, dasatinib selectively kills primary neoplastic bone marrow mast cells from patients with systemic mastocytosis while sparing other hematopoietic cells. Computer modeling suggests that the KITD816V mutation destabilizes the inactive conformation of the KIT activation loop to which imatinib binds, but it is not predicted to impair binding of KIT by dasatinib. Based upon our results, further evaluation of dasatinib for the treatment of systemic masto-cytosis in clinical trials is warranted. Moreover, dasatinib may be of clinical utility in other disease settings driven by activating KIT mutations. (Blood. 2006;108:286-291)
Introduction
Systemic mastocytosis and mast-cell leukemia are relatively rare conditions that are characterized by a pathologic accumulation of mast cells in various tissues.1 Previous work has demonstrated the clonal nature of the disorder as evidenced by an activating point mutation in the KIT receptor tyrosine kinase.2,3 This mutation, KITD816V, occurs near the activation loop of the kinase and can be identified in more than 80% of systemic mastocytosis cases and thus represents an attractive target for this disorder, for which few effective therapeutic options exist.1 Although a small molecule tyrosine kinase inhibitor of KIT, imatinib mesylate, has been available to patients recently, both preclinical and clinical studies have demonstrated convincingly that the KITD816V mutation is inherently resistant to imatinib.4-6 The crystal structure of the wild-type KIT kinase domain has been solved in an autoinhibited state, with the activation loop of the kinase in a closed conformation,7 similar to the cocrystal structure of imatinib bound to the ABL kinase domain.7,8 These structural studies suggest that substitution of valine for aspartic acid at position 816 in KIT may alter the conformation of the activation loop and thus prevent imatinib from efficiently binding to KITD816V. Inhibition of KITD816V has thus become the focus of recent studies aiming to find a curative therapy for mast-cell disease, and several potential drug candidates with an ability to inhibit KITD816V have been identified.9-15
Dasatinib (BMS-354825) is a novel, potent, oral, multitargeted kinase inhibitor that targets ABL, SRC, KIT, PDGFR, and other tyrosine kinases. Dasatinib is structurally unrelated to imatinib16 and is currently showing great promise for the treatment of all stages of imatinib-resistant and -intolerant chronic myeloid leukemia (CML) in early clinical development. The cocrystal structure of dasatinib bound to the kinase domain of ABL reveals that the compound binds to the active conformation of the kinase and, in contrast to imatinib, is not expected to be susceptible to alterations in the activation loop.17 This is supported by the observed inhibitory activity of dasatinib against 18 of 19 BCR-ABL mutations known to confer imatinib resistance, including those that result in conformational changes to the kinase.16,18 We therefore hypothesized that dasatinib would bind to KIT regardless of the conformation of the KIT activation loop and sought to evaluate dasatinib for potential activity in mastocytosis.
Here we provide preclinical evidence of effective binding of dasatinib to wild-type KIT at a concentration approximately 20-fold lower than that required for imatinib. Furthermore, we observed inhibition of KITD816V by dasatinib in in vitro kinase activity assays, which correlated with inhibition of growth of neoplastic cell lines carrying this mutation. Last, we provide evidence for efficient killing of primary human neoplastic mast cells carrying KITD816V ex vivo at concentrations that are safely achievable in humans. These studies clearly indicate that clinical trials to assess dasatinib for the treatment of aggressive variants of systemic mastocytosis are warranted.
Materials and methods
Inhibitors
Imatinib was provided by Novartis (Basel, Switzerland). Dasatinib was provided by Bristol-Myers Squibb Oncology (Princeton, NJ).
In vitro kinase assay
GST (glutathione S-transferase)-tagged KIT or KIT D816V (amino acids 544-end) (5 to 10 mU) was incubated with 8 mM MOPS (pH 7.0), 0.2 mM EDTA, 10 mM MnCl2, 0.1 mg/mL poly(Glu/Tyr) (4:1), 10 mM magnesium acetate, and [γ-33 P-ATP] (specific activity approximately 500 cpm/pmol) in a final reaction volume of 25 μL (Kinase Profile; Upstate, Dundee, United Kingdom). The reaction was initiated by the addition of the magnesium-ATP mix. After incubation for 40 minutes at room temperature, the reaction was stopped by the addition of 5 μL of a 3% phosphoric acid solution. Next, 10 μL of the reaction was spotted onto a Filtermat A and washed 3 times for 5 minutes in 75 mM phosphoric acid and once in methanol prior to drying and scintillation counting.
Cell-based kinase assay
Aliquots of 1 × 106 to 5 × 106 cells were serum starved for 3 hours and incubated in the presence of varying concentrations of inhibitors for 1 hour in Iscove medium. Cells were then lysed in 1% Triton containing the following protease and phosphatase inhibitors as described19 : Complete protease inhibitor cocktail (4 tablets per 10 mL) (Roche Molecular Biochemicals, Indianapolis, IN), Sigma protease inhibitor cocktail (500 μL/mL) (Sigma, St Louis, MO), 3,4 dichloroisocoumarin (50 μg/mL) (Roche Molecular Biochemicals), and benzamidine (1 mM); and the following phosphatase inhibitors: sodium orthovanadate (1 mM), sodium pyrophosphate (5.4 mM), and sodium fluoride (50 mM) (Sigma). Cells were lysed by adding an equal amount of the lysis buffer to cell suspension and passing several times through a 20-gauge needle, boiled for 5 minutes, and spun at 16 000g for 5 minutes. Twenty microliters of lysate was electrophoresed on a 4% to 12% NuPAGE Bis-Tris gel. Western blot analysis was performed using [pY823] phosphospecific anti-KIT (Bio-source, Camarillo, CA) or the anti-KIT antibodies (clone 57A5; Calbio-chem, San Diego, CA).
Cell lines
The murine P815 mastocytoma cell line expressing the D814V mutation (corresponding to human D816V) was purchased from American Type Culture Collection ([ATCC] Manassas, VA). The cells were cultured in RPMI 1640 medium supplemented with 10% fetal bovine serum (FBS) and 25 mM HEPES buffer at 37°C, 5% CO2.
Two previously described subclones of the human mastocytosis cell line HMC-1 were kindly provided by Dr Joseph Butterfield (Mayo Clinic).20 HMC-1.1V560G+, D816V- cells harbor only the activating mutation KITV560G, and HMC-1.2V560G+, D816V+ cells harbor the D816V mutation in addition. Both cell lines were propagated in Iscove medium supplemented with 10% fetal calf serum.
Cell growth inhibition assays
HMC cell lines were plated at 2 × 105/mL in the presence of varying concentrations of inhibitors. After 24, 48, and 72 hours, viable cells were counted by trypan blue dye exclusion. Annexin V staining was performed using a commercially available kit according to manufacturer's instructions (R&D Systems, Minneapolis, MN), and the cells were analyzed on a flow cytometer (FACSCalibur, Becton Dickinson, San Jose, CA).
P815 cells were plated at a density of 4 × 104 cells per well and grown overnight. Compounds were then added, and after 24, 48, and 72 hours, cell growth was determined by direct counting using a Coulter Channelyzer (Beckman Coulter, Miami, FL).
Mutational analysis and ex vivo human neoplastic mast-cell cytotoxicity assays
After obtaining informed consent on a clinical protocol approved by the Institutional Review Board of the University of Michigan, 5 to 10 mL of bone marrow aspirate was harvested from 4 patients with indolent systemic mastocytosis. For mutational analysis studies, mast cells were enriched by CD25+ magnetic bead selection as described.5 Briefly, bone marrow mononuclear cells were incubated with CD25 paramagnetic beads (Milte-nyi Biotec, Auburn, CA) for 30 minutes at 8°C in PBS containing 2 mM EDTA and 0.1% BSA, and the CD25+ cells were isolated using a miniMacs column according to manufacturer's instructions. The eluted cells were centrifuged at 500g for 5 minutes, and the pellet was lysed in 0.8 mL Trizol reagent (Invitrogen, Carlsbad, CA). Total RNA was reverse transcribed to cDNA by Superscript II kit (Invitrogen) following the manufacturer's guidelines. The presence of the KITD816V mutation in synthesized cDNA was demonstrated by polyerase chain reaction (PCR) amplification of this region, followed by restriction digestion with HinfI and HaeIII as previously described.21
For ex vivo culture studies, bone marrow mononuclear cells were isolated by Histopaque (density 1.077) gradient centrifugation for 30 minutes, washed once in Stem-Pro serumfree medium, and cultured at a density of 1 × 106/mL in 1 mL Stem-Pro serumfree medium for 7 days with or without inhibitors. Mast cells in bone marrow cultures were identified by flow cytometry as a CD117+-high, side scatter-high population as previously described.5 Briefly, bone marrow mononuclear cells were incubated in 100 μL aliquots for 30 minutes at 4°C with a phycoerythrin (PE) conjugate of anti-human CD117 (clone 104D2; Becton Dickinson). The cells were then washed, resuspended in PBS containing 0.1% BSA, and analyzed on a flow cytometer (FACSCalibur, Becton Dickinson). The percentage of mast cells in the mononuclear-cell population was then determined in cultures with or without inhibitors. Mast-cell percentage results were normalized to the counts obtained in the absence of inhibitors. Mast cells constituted 0.08% to 0.7% of the mononuclear cells in untreated cultures.
Computer modeling of imatinib and dasatinib in the KIT kinase domain
Imatinib was superimposed upon the crystal structure of the inactive conformation of KIT (pdb code 1T4622 ). Dasatinib is structurally similar to the SRC/ABL kinase inhibitor PD173955.23 Modeling was performed by superimposing the active conformation of KIT (pdb code 1PKG7 ) onto the structure of ABL kinase in complex with PD173955 (pdb code 1M52) and aligning a model of dasatinib on the position of PD173955. Small adjustments of dasatinib with respect to 1PKG were made to remove steric clashes.
Results
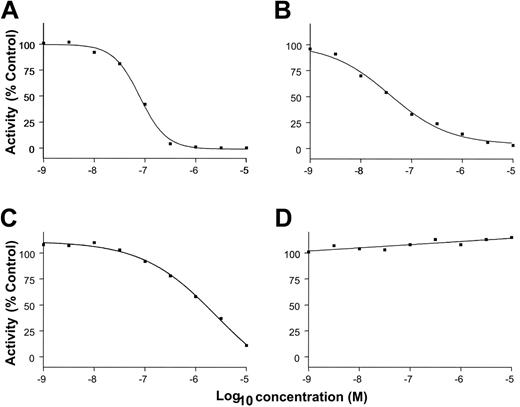
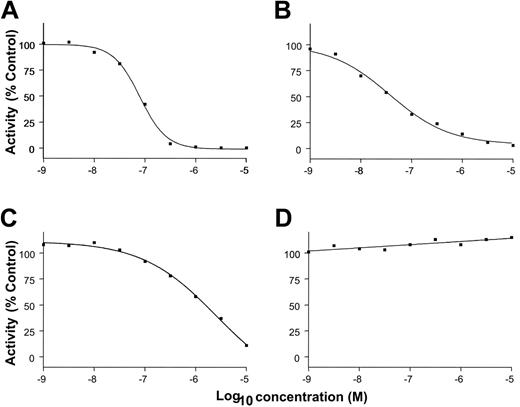
The abilities of imatinib and dasatinib to inhibit the kinase activity of KIT in vitro were compared. Figure 1 and Table 1 reveal that dasatinib inhibits the kinase activity of wild-type KIT approximately 20-fold more efficiently than imatinib. Significantly, dasatinib inhibits the kinase activity of KITD816V with comparable efficiency to wild-type KIT (IC50 of 37 and 79 nM, respectively) in in vitro kinase experiments, whereas the ability of imatinib to inhibit KITD816V kinase activity is highly impaired.
Inhibition of KIT by dasatinib. Inhibition of the kinase activity of human wild-type (A,C) and mutant (B,D) c-KIT by dasatinib (A-B) and imatinib (C-D). Kinase activity was conducted on N-terminal GST-tagged recombinant c-KIT (amino acids 544-end). IC50 was calculated by regression analysis.
Inhibition of KIT by dasatinib. Inhibition of the kinase activity of human wild-type (A,C) and mutant (B,D) c-KIT by dasatinib (A-B) and imatinib (C-D). Kinase activity was conducted on N-terminal GST-tagged recombinant c-KIT (amino acids 544-end). IC50 was calculated by regression analysis.
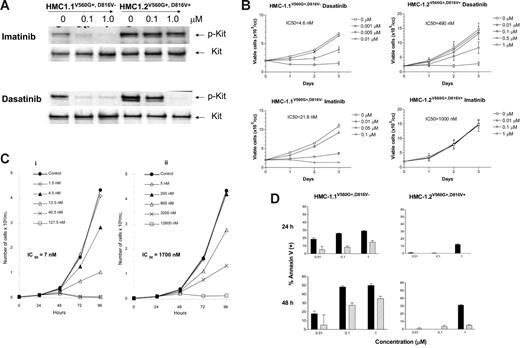
To assess for inhibition of KITD816V kinase activity by dasatinib in vivo, HMC-1.1V560G+, D816V- and HMC-1.2V560G+, D816V+ human mast-cell leukemia cells carrying V560G and D816V mutations were incubated in the presence of varying concentrations of the compound, and phosphotyrosine-associated KIT was assessed. Inhibition of KITV560G (HMC-1.1V560G+, D816V-) autophosphorylation was noted at concentrations significantly lower than those observed for imatinib, with inhibition of phospho-KIT at concentrations as low as 10 nM. While imatinib failed to inhibit KITV560G, D816V (HMC-1.2V560G+, D816V+) autophosphorylation at concentrations of up to 1 μM, dasatinib resulted in substantially decreased levels of phospho-KIT in the high nanomolar range (Figure 2A).
Growth inhibition assays of the HMC-1.1V560G+, D816V- and HMC-1.2V560G+, D816V+ cell lines were also performed and reveal that, consistent with previous studies, imatinib harbors activity against HMC-1.1V560G+, D816V- at high nanomolar concentrations but has no detectable effect on growth inhibition of KITD816V-harboring HMC-1.2V560G+, D816V+ cells at concentrations up to 1 μM. In contrast, dasatinib suppresses the growth of HMC-1.1V560G+, D816V- cells in the low nanomolar range and is approximately 5 times more potent than imatinib in this assay. Furthermore, dasatinib retains activity against HMC-1.2V560G+, D816V+ cells, although higher concentrations are required (Figure 2B). Dasatinib also shows a strong growth inhibitory activity against the P815 rodent mastocytoma line, which carries KITD814V, the murine equivalent of KIT D816V.
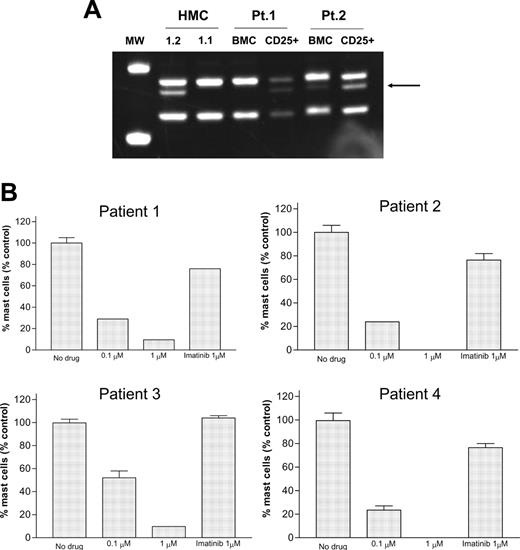
Because studies with the cell lines may not reflect the true sensitivity of neoplastic bone marrow primary mast cells, experiments were performed with primary bone marrow cells from patients with systemic mastocytosis. The presence of the KITD816V mutation was documented by reverse transcriptase (RT)-PCR of the corresponding region of KIT followed by restriction enzyme digestion with HinfI (Figure 3A) in CD25+ mast-cell-enriched bone marrow samples from all patients. To assess whether primary human neoplastic mast cells that harbor KITD816V are sensitive to dasatinib, a flow cytometry-based assay of mast-cell viability was employed. Previous studies showed an excellent correlation of the results of mast-cell viability in this assay with inhibition of KIT kinase activity, which was also associated with clinical response in one report.5,24 Using this assay system, clear preferential cytotoxicity to neoplastic mast cells was demonstrated in bone marrow mononuclear-cell cultures established from patients with mastocytosis in the presence of dasatinib at 0.1 μM concentration, with increased activity observed at 1 μM. In contrast, imatinib had no significant activity at 1 μM, as expected (Figure 3B).
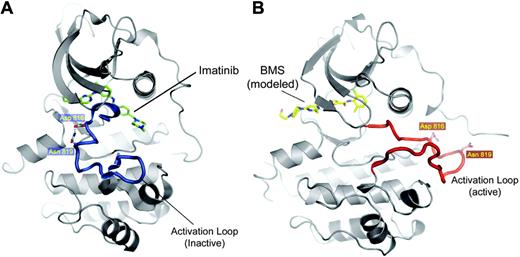
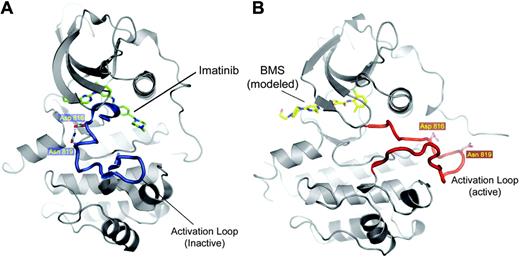
To understand how dasatinib may be capable of binding to KIT even in the presence of the D816V mutation, we compared the crystal structure of imatinib bound to KIT with a model of dasatinib bound to the KIT kinase domain (Figure 4). D816 resides within the activation loop of KIT and is important for maintaining the inactive conformation that imatinib prefers by forming a hydrogen bond with N819. Replacement of this aspartic acid residue with valine breaks this bond and thereby destabilizes the inactive conformation, thus preventing imatinib from binding. Dasatinib binds to the active conformation of ABL and is predicted to bind KIT in a similar manner. Because this conformation does not depend on interactions of D816, the D816V mutation would not be expected to have a drastic effect on the ability of dasatinib to bind and inhibit KIT activity.
Discussion
Mastocytosis is a disease with remarkable variation in its clinical course and prognosis. While symptomatic management is recommended to patients with indolent systemic mastocytosis, mast-cell cytoreductive therapy is indicated for the aggressive variants of systemic mastocytosis associated with poorer prognoses.25 The current options for cytoreductive therapy of mastocytosis include interferon alfa-2b26 and cladribine.27 While these drugs can at least temporarily halt the progression of disease and lead to a variable degree of mast-cell cytoreduction, they are not uniformly effective in all patients and their use is fraught with poor tolerability and potentially serious adverse effects.
The promise of targeted inhibition of oncogenic tyrosine kinases for the effective treatment of human malignancy has been validated in many disease settings. Imatinib inhibits wild-type KIT as well as KIT with transmembrane and juxtamembrane mutations,4-6 and this inhibition is associated with therapeutic activity in tumors, including gastrointestinal stromal tumors (GIST) and an unusual case of mastocytosis driven by these mutations.24,28 While plasma concentrations of imatinib in the low micromolar range can be safely achieved in humans,29 inhibition of KITD816V is not obtained at these drug concentrations.4,5 Given the high association of this activating point mutation with the clear majority of systemic mastocytosis cases, identification of novel compounds with the ability to inhibit the activity of this mutant kinase is expected to result in great therapeutic efficacy in the treatment of this currently incurable disorder. Indeed, PKC412, another small molecular weight tyrosine kinase inhibitor with in vitro efficacy against KIT D816V, has produced a transient clinical response in a patient with an aggressive mast-cell leukemia bearing this mutation.9 This report, together with an earlier report of induction of complete remission of a patient with mastocytosis carrying a transmembrane KIT F522C mutation24 and treated with imatinib, provided proof of principle that KIT in mast-cell disease represents a valid pharmacologic target.
Sensitivity of the cell lines carrying activating c-KIT mutations to dasatinib. (A) Western blot analysis of lysates prepared from HMC-1.1V560G+, D816V- and HMC-1.2V560G+, D816V+ cell lines following incubation in the presence of imatinib or dasatinib. Cells were serum starved for 3 hours and exposed for 60 minutes to the inhibitors indicated at the concentrations listed (μM). p-kit indicates phospho-KIT (B) Cell-growth inhibition of HMC-1.1V560G+, D816V- and HMC-1.2V560G+, D816V+ in the presence of varying concentrations of imatinib or dasatinib. Days in culture at the time of analysis are indicated. Each data point represents mean ± SEM from 3 separate experiments with duplicate counts. P < .05 at all concentrations of dasatinib or imatinib in HMC-1.1V560G+, D816V- cells and at 0.5 and 1 mM dasatinib in HMC-1.2 V560G+, D816V+ cells (2-tailed, paired t test on day-3 results). (C) Inhibition of cell growth of the P815 murine mastocytosis cell line harboring a c-KIT (D814V) mutation. Cells were grown in the presence of varying concentrations of dasatinib (i) or imatinib (ii). Days in culture at the time of analysis are indicated. (D) Annexin V binding of HMC-1.1V560G+, D816V- and HMC-1.2V560G+, D816V+ cells as assessed by flow cytometry. Cells were cultured with various concentrations of inhibitors as shown and analyzed at 24 and 48 hours. Baseline values of annexin V-positive cells in untreated cultures were subtracted from each treatment. Each point represents mean ± SEM from duplicate measurements. Dasatinib, ▪; imatinib, ▨.
Sensitivity of the cell lines carrying activating c-KIT mutations to dasatinib. (A) Western blot analysis of lysates prepared from HMC-1.1V560G+, D816V- and HMC-1.2V560G+, D816V+ cell lines following incubation in the presence of imatinib or dasatinib. Cells were serum starved for 3 hours and exposed for 60 minutes to the inhibitors indicated at the concentrations listed (μM). p-kit indicates phospho-KIT (B) Cell-growth inhibition of HMC-1.1V560G+, D816V- and HMC-1.2V560G+, D816V+ in the presence of varying concentrations of imatinib or dasatinib. Days in culture at the time of analysis are indicated. Each data point represents mean ± SEM from 3 separate experiments with duplicate counts. P < .05 at all concentrations of dasatinib or imatinib in HMC-1.1V560G+, D816V- cells and at 0.5 and 1 mM dasatinib in HMC-1.2 V560G+, D816V+ cells (2-tailed, paired t test on day-3 results). (C) Inhibition of cell growth of the P815 murine mastocytosis cell line harboring a c-KIT (D814V) mutation. Cells were grown in the presence of varying concentrations of dasatinib (i) or imatinib (ii). Days in culture at the time of analysis are indicated. (D) Annexin V binding of HMC-1.1V560G+, D816V- and HMC-1.2V560G+, D816V+ cells as assessed by flow cytometry. Cells were cultured with various concentrations of inhibitors as shown and analyzed at 24 and 48 hours. Baseline values of annexin V-positive cells in untreated cultures were subtracted from each treatment. Each point represents mean ± SEM from duplicate measurements. Dasatinib, ▪; imatinib, ▨.
Dasatinib is a thiazolecarboxamide that is presently in phase 2 clinical trials for the treatment of imatinib-resistant and -intolerant cases of CML and in phase 1 trials for solid tumors. Here we provide evidence of significant preclinical activity of this compound against KITD816V in the high nanomolar range. Our experiments indicate that 100 nM dasatinib is sufficient to not only inhibit the kinase activity of wild-type KIT and KITD816V but is also preferentially toxic to primary neoplastic mast cells as compared with other hematopoietic cells in the ex vivo culture system. Pharmacokinetic studies performed during a phase 1 dose-escalation study of dasatinib have demonstrated that high nanomolar concentrations of the compound can be safely achieved in humans.
Imatinib is the prototype small molecule tyrosine kinase inhibitor, and it appears that this compound binds to select kinases when in the inactive conformation and “freezes” the kinase in this state. It has been postulated that the safety and tolerability of imatinib is a reflection of its “conformation-restricted” binding. However, studies of acquired resistance cases to imatinib,30-39 and to other small molecule tyrosine kinase inhibitors such as gefitinib40,41 and erlotinib41 currently employed for the treatment of human malignancy, clearly implicate the acquisition of secondary kinase domain mutations as the predominant molecular mechanism of resistance. Because many of these secondary mutations are thought to impair the ability of the target kinase to adopt the inactive conformation to which imatinib binds, “conformation-tolerant” compounds such as dasatinib are expected to be less susceptible to subtle alterations in the kinase domain.42 Furthermore, mutations near the activation loop of target kinases, such as the activating KITD816V mutation that drives systemic mastocytosis as well as some cases of GIST, are expected to have little effect on the inhibitory activity of active conformation binders such as dasatinib. Indeed, both preclinical as well as early clinical evidence obtained from a phase 1 clinical trial suggest that nearly all imatinib-resistant BCR-ABL mutations are sensitive to dasatinib. Based upon the work presented here, clinical trials to assess the efficacy of dasatinib for the treatment of systemic mastocytosis are clearly warranted.
Analysis of primary bone marrow cells obtained from patients with mastocytosis. (A) HinfI restriction analysis of bone marrow cells isolated from patients with systemic mastocytosis. RNA was isolated from either unselected bone marrow or CD25-sorted marrow cells. The presence of the KITD816V mutation is indicated by the appearance of a novel restriction fragment as indicated by the arrow. (B) Primary neoplastic mast-cell viability following culture of bone marrow isolated from 4 patients with systemic mastocytosis in the presence of imatinib or dasatinib. Bars indicate mean ± SEM from duplicate cultures for each dose in 4 different patients. P < .001 comparing no treatment with 0.1 and 1 μM dasatinib by 2-tailed t test on pooled data.
Analysis of primary bone marrow cells obtained from patients with mastocytosis. (A) HinfI restriction analysis of bone marrow cells isolated from patients with systemic mastocytosis. RNA was isolated from either unselected bone marrow or CD25-sorted marrow cells. The presence of the KITD816V mutation is indicated by the appearance of a novel restriction fragment as indicated by the arrow. (B) Primary neoplastic mast-cell viability following culture of bone marrow isolated from 4 patients with systemic mastocytosis in the presence of imatinib or dasatinib. Bars indicate mean ± SEM from duplicate cultures for each dose in 4 different patients. P < .001 comparing no treatment with 0.1 and 1 μM dasatinib by 2-tailed t test on pooled data.
Ribbon representations of KIT. (A) The crystal structure of an inactive conformation of KIT bound to imatinib (green) is shown.7 The activation loop, shown in the inactive state, is depicted in blue. The positions of D816 and N819 are shown as well as the hydrogen bond formed between these residues, which stabilizes the inactive conformation. (B) The active conformation of KIT is shown, with dasatinib (yellow) modeled into the active site. The activation loop (red) is depicted in the active conformation.
Ribbon representations of KIT. (A) The crystal structure of an inactive conformation of KIT bound to imatinib (green) is shown.7 The activation loop, shown in the inactive state, is depicted in blue. The positions of D816 and N819 are shown as well as the hydrogen bond formed between these residues, which stabilizes the inactive conformation. (B) The active conformation of KIT is shown, with dasatinib (yellow) modeled into the active site. The activation loop (red) is depicted in the active conformation.
In our experiments, a higher dasatinib concentration was required to inhibit the kinase activity and cell growth of HMC-1.2V560G+, D816V+ cells than HMC-1.1V560G+, D816V- cells. In light of the equivalent potency of dasatinib against wild-type KIT and KITD816V in in vitro kinase assays, coupled with the observation that the rodent mastocytoma cell line is highly sensitive to dasatinib, the reason for this discrepancy is presently unclear. It is possible that the compound V560G and D816V KIT mutations present in HMC-1.2V560G+, D816V+ cells may alter the KIT kinase domain conformation and make binding by dasatinib less favorable. Notably, most cases of mastocytosis are associated with a single activating KIT mutation, and the sensitivity of primary neoplastic mast cells isolated from mastocytosis patients presented in this study further supports the promise of dasatinib for patients with systemic mastocytosis.
A recent study showed that dasatinib was bound to 47 of 148 kinases with high affinity (Kd less than 200 nM).43 Despite the apparent promiscuity of the drug, dasatinib appears to be generally well tolerated in patients with CML. This apparent paradox may be due to the short biologic half-life of the drug, which, while sufficient for efficacy, may limit toxicity. It is possible that the higher peak concentrations necessary to inhibit KIT activity will require more aggressive dosing, and the promise of this drug for systemic mastocytosis cases will depend to a large extent upon its safety and tolerability at higher doses, which remain to be established. The chemotype of dasatinib, which is distinct from that of imatinib and AMN107 in its ability to bind to the KIT kinase domain in the active conformation, should facilitate the development of KIT inhibitors that harbor even greater selectivity and potency.
Finally, some patients meeting the World Health Organization (WHO) criteria for systemic mastocytosis may carry the FIP1L1-PDGFRA fusion gene instead of KITD816V.44 These patients present with a myeloproliferative disorder characterized by prominent eosinophilia and mast-cell dysplasia. While these patients respond to imatinib, resistance to this drug may emerge by acquiring point mutations in the kinase domain of PDGFRA.45 PKC412, a drug capable of inhibiting the KITD816V, has also shown to be effective for the PDGFRA mutants resistant to imatinib.46 Dasatinib binds PDGFRA with high affinity43 although it is not known whether the drug will have any efficacy on FIP1L1-PDGFRA-associated myeloproliferative disease. However, based on structural similarity of PDG-FRA and KIT, the drug may also have activity in cases of systemic mastocytosis associated with the FIP1L1-PDGFRA fusion gene, including cases of imatinib resistance. Dasatinib thus offers significant promise for systemic mastocytosis, and clinical trials are currently ongoing.
Prepublished online as Blood First Edition Paper, January 24, 2006; DOI 10.1182/blood-2005-10-3969.
Supported in part by a grant from the Mastocytosis Society (C.A.), University of Michigan internal funds (C.A.), a Leukemia & Lymphoma Society Career Development Award for Special Fellows (N.P.S.), and the UCLA Mentored Clinical Pharmacology Research Scholars Award (N.P.S.).
Two of the authors (F.Y.L., R.L.) are employed by and own stock in a company (Bristol-Myers Squibb Oncology) whose product was studied in the present work.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
We thank Bhushan Nagar and John Kuriyan at the University of California, Berkeley, for contributing structural figures.