A wide range of factor VIII and IX levels is observed in heterozygous carriers of hemophilia as well as in noncarriers. In female carriers, extreme lyonization may lead to low clotting factor levels. We studied the effect of heterozygous hemophilia carriership on the occurrence of bleeding symptoms. A postal survey was performed among most of the women who were tested for carriership of hemophilia in the Netherlands before 2001. The questionnaire included items on personal characteristics, characteristics of hemophilia in the affected family members, and carrier testing and history of bleeding problems such as bleeding after tooth extraction, bleeding after tonsillectomy, and other operations. Information on clotting factor levels was obtained from the hospital charts. Logistic regression was used to assess the relation of carrier status and clotting factor levels with the occurrence of hemorrhagic events. In 2004, 766 questionnaires were sent, and 546 women responded (80%). Of these, 274 were carriers of hemophilia A or B. The median clotting factor level of carriers was 0.60 IU/mL (range, 0.05-2.19 IU/mL) compared with 1.02 IU/mL (range, 0.45-3.28 IU/mL) in noncarriers. Clotting factor levels from 0.60 to 0.05 IU/mL were increasingly associated with prolonged bleeding from small wounds and prolonged bleeding after tooth extraction, tonsillectomy, and operations. Carriers of hemophilia bleed more than other women, especially after medical interventions. Our findings suggest that not only clotting factor levels at the extreme of the distribution, resembling mild hemophilia, but also mildly reduced clotting factor levels between 0.41 and 0.60 IU/mL are associated with bleeding. (Blood. 2006;108:52-56)
Introduction
Hemophilia is an X-linked hereditary bleeding disorder caused by a deficient or defective coagulation factor VIII (hemophilia A) or factor IX (hemophilia B). Resulting from the recessive X-chromosomal inheritance pattern, mostly men are affected while their female relatives may be heterozygous for the mutation, often referred to as carriers of hemophilia. Previously, pedigree analysis and clotting factor VIII or IX levels were used to diagnose carriership for hemophilia.1 In the early 1980s, it became possible to ascertain the carrier status by means of DNA analysis, which has evolved from haplotyping to mutation analysis offering certainty about the carrier status.2 During the last 3 decades, genetic counseling, carrier testing, and prenatal diagnosis of hemophilia have become an integrated part of the comprehensive care for hemophilia.3
Female carriers are expected to have a plasma concentration of factor VIII or IX corresponding to half the concentration found in healthy individuals, which is generally sufficient for normal hemostasis. However, in carriers a wide range in clotting factor levels is seen, from very low, resembling affected males, to the upper limit of normal.4 This range has been attributed to the phenomenon of lyonization, random X-chromosome inactivation, which takes place in the early embryonic life.5 Other genetic factors, such as ABO blood group, may also affect factor VIII and IX plasma concentrations in carriers as well as noncarriers, in whom a wide distribution also is observed.6
Although Merskey and Macfarlane7 already reported excessive bleeding after tooth extraction in 47% of known carriers (n = 19) in 1952, this first publication was not followed by larger studies. Some case series showed joint bleeds, prolonged bleeding after tonsillectomy, tooth extractions, or postpartum bleeding.8-13
It is important to assess the risk of bleeding in carriers of hemophilia to enable physicians to improve care for hemophilia carriers, for instance, by the implementation of prophylactic intervention in carriers at risk for bleeding.
While extensive information on bleeding in men with hemophilia is available, only a few studies have focused on bleeding in carriers. We present a large national cross-sectional study examining bleeding in women in whom genetic testing for hemophilia was performed within the last decade. We focused on spontaneous bleeding events, bleeding after trauma, and bleeding following surgical interventions.
The aim of this study was to examine the risk of bleeding among carriers of hemophilia A or B compared with noncarriers.
Patients and methods
Subjects
We contacted all women who had been tested for carriership of hemophilia A or B before 2001 in the Netherlands. The women had to be 18 years or older to participate. Diagnosis of carriership of hemophilia was based on DNA analysis, pedigree analysis, or the assessment of clotting factor levels. Carriers of hemophilia were women in whom the genetic defect related to hemophilia was established through DNA analysis (haplotype or mutation analysis) or, before 1985, through the determination of clotting factor levels in combination with pedigree analysis. Noncarriers were women in whom testing showed that they were not likely to be carrying the mutation that caused hemophilia A or B in their family, by the same procedures as for carriers. By comparing carriers with noncarriers both from hemophilic families we excluded the possible bias introduced by knowledge of hemophilia.
Assessments
Questionnaires were sent by mail, followed by 2 reminder letters. The questionnaire included items on personal characteristics, type and severity of hemophilia in affected relatives, carrier testing, and several bleeding problems. We assessed whether patients ever reported spontaneous bleeding and bleeding after trauma: bruising, nose bleeds, gum bleedings, and joint bleeds. Questions on bleeding after medical interventions included bleeding after tooth extractions, adenotomy or tonsillectomy, and operations. Prolonged bleeding after medical interventions was defined as bleeding for more than 3 hours after tooth extractions, adenotomy or tonsillectomy, or operations. The topics on bleeding were based on a validated questionnaire developed by Srámek et al, validated by means of sensitivity analysis.14 Restrictions in daily life due to excessive blood loss during the menstrual period were measured on a 7-point scale in which a score of 1 represented no restrictions, and a score of 7, severe restrictions. To evaluate the questionnaire a pilot study was performed in 12 carriers. Informed consent was obtained to allow us to verify the diagnosis (type and severity of hemophilia in the family) and to obtain information on factor VIII and IX activity from the medical files of the patients in the hemophilia treatment centers. In most women, clotting factor activity had been determined at several time points, in which case the lowest value was used for evaluation in this study. Severity of hemophilia in the male family members was classified according to residual percentage of factor VIII or IX clotting activity: severe (less than 0.01 IU/mL), moderate (0.01 to 0.05 IU/mL), or mild (more than 0.05 to 0.40 IU/mL). The Committee of Medical Ethics of the Leiden University Medical Center approved this study.
Data analysis
Women with clotting disorders due to other causes than hemophilia or who used antithrombotic medication were excluded from the analysis. The prevalence of bleeding symptoms in women who were carriers of hemophilia A or B was compared with that of women not carrying a hemophilia mutation. Due to the limited number of women reporting hemophilia B in the family, we could not distinguish between the 2 types of hemophilia in the analysis. The risk of bleeding related to the carrier status and clotting factor levels was determined, and we tested for a graded response using a Wald test. If in the comparison between carriers and noncarriers a specific bleeding event showed a relative risk (RR) above 1 and a 95% confidence interval (CI) not including 1, its association with clotting factor levels is also presented. In the analysis of bleeding risk caused by specific interventions, only women who ever underwent this intervention were included in the analysis. Women who were treated with tranexamic acid, desmopressin, or clotting factor preparations before the medical intervention were excluded from the analysis because this affects the preexisting bleeding risk. Clotting factor levels were analyzed as a categorical variable; the studied categories were as follows: 0.40 IU/mL or below, 0.41 to 0.60 IU/mL, and more than 0.60 IU/mL. In the analysis of excessive blood loss during the menstrual period, only women who were premenopausal were included. To exclude the effect of referral for carrier testing because of bleeding problems, we calculated the risk of bleeding after adenotomy or tonsillectomy or operations among women who were not tested because of an increased bleeding tendency.
Results
Response and patient characteristics
A total of 766 questionnaires were sent, and 546 questionnaires were completed and returned (response of 80%). Excluded from analyses were women who reported clotting disorders other than hemophilia (19 women of whom 13 had von Willebrand disease) and 10 women in whom the carrier status was not conclusive or unknown. This resulted in 274 carriers and 245 noncarriers for the current analyses. Table 1 shows the general characteristics according to hemophilia carrier status. The median age of the carriers and noncarriers was similar: 39 years (range, 18-77 years) and 40 years (range, 20-90 years), respectively. Current use of oral contraceptives in carriers and noncarriers was similar, at 29% and 27%, respectively. Past use of oral contraceptives was reported by 159 carriers (51%) and by 119 noncarriers (56%). Carrier testing by means of DNA analysis, available in the Netherlands since 1985, was performed in 177 carriers (57%) and in 122 noncarriers (58%).
Factor VIII and IX characteristics
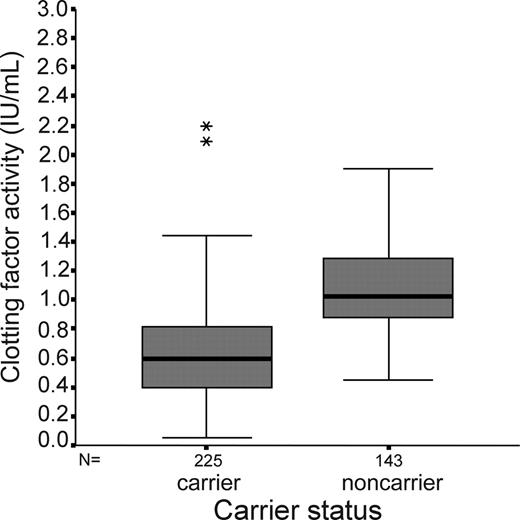
Clotting factor levels were missing for 18% (49 of 274) of carriers and 43% (103 of 245) of noncarriers. The median clotting factor level in carriers was 0.60 IU/mL (range, 0.05-2.19 IU/mL) compared with 1.02 IU/mL (range, 0.45-3.28 IU/mL) in noncarriers. Sixty-two carriers and none of the noncarriers had a clotting factor level of 0.40 IU/mL or below. Figure 1 shows the distribution of clotting factor levels in carriers and noncarriers.
Bleeding symptoms
Spontaneous bleeding and bleeding after trauma.Table 2 presents the risk of (ever having experienced) bleeding of carriers compared with noncarriers. The risk of prolonged bleeding (more than 5 minutes) from small wounds was 2 times higher (RR, 2.2; 95% CI, 1.4 to 3.5) in carriers than noncarriers.
Low clotting factor levels were associated with an increased occurrence of prolonged bleeding from small wounds and joint bleeding (Table 3). Joint bleeds were reported by 8% of carriers and by 5% of women not carrying hemophilia, which was a 2 times increased risk (RR, 1.9; CI, 0.9 to 3.7). Although no higher risk of nose bleeds was observed in carriers compared with noncarriers, prolonged nose bleeding occurred more often in carriers: 9% of carriers had nose bleeds that lasted longer than 10 minutes compared with 2% of noncarriers. Seventeen percent of carriers had received treatment for nose bleeds compared with 10% of noncarriers. Carriers of hemophilia did not have a higher risk of large bruising and gum bleeding.
Clotting factor level in relation to carrier status shown for participants for whom clotting factor level is known. This box-whisker plot shows the median and the interquartile range of clotting factor activity levels in carriers and noncarriers. The box is marked by the first and the third quartile; the whiskers indicate the range. The stacked asterisks indicate two extremes (2.09 and 2.19 IU/mL).
Clotting factor level in relation to carrier status shown for participants for whom clotting factor level is known. This box-whisker plot shows the median and the interquartile range of clotting factor activity levels in carriers and noncarriers. The box is marked by the first and the third quartile; the whiskers indicate the range. The stacked asterisks indicate two extremes (2.09 and 2.19 IU/mL).
Bleeding after medical interventions. Tooth extractions had been performed in 228 carriers and 219 noncarriers, and the risk of bleeding for more than 3 hours after tooth extraction was 2 times higher in carriers than noncarriers (RR, 2.3; CI, 1.5 to 3.4) (Table 4). In 24 of 228 carriers, additional treatment due to bleeding after tooth extractions had been required compared with 1 of 219 noncarriers. Treatment included intervention by a dentist or the use of tranexamic acid, desmopressin, or administration of clotting factor concentrate. Clotting factor levels below 0.60 IU/mL were associated with prolonged bleeding after tooth extraction. A total of 123 carriers and 122 noncarriers underwent tonsillectomy or adenotomy; 24% of carriers and 13% of noncarriers reported bleeding for more than 3 hours following tonsillectomy (RR, 1.8; CI, 1.0 to 3.1). In 8 carriers (3%), a blood transfusion was required after (adeno) tonsillectomy compared with none of the noncarriers. Eight percent of women carrying hemophilia needed treatment for bleeding following surgery. In most cases, a second intervention to treat bleeding had to be performed. Decreasing clotting factor levels were also associated with prolonged bleeding after (adeno) tonsillectomy. Women with a clotting factor level of 0.40 IU/mL or below had a 2.1 times (RR, 2.1; CI, 1.1 to 3.9) increased risk compared with women with a clotting factor level above 0.60 IU/mL. Prolonged bleeding for more than 3 hours after 1 or more operations was reported by 46 of 163 carriers and by 16 of 146 noncarriers (RR, 2.6; CI, 1.5 to 4.3). Women with a clotting factor level of 0.40 IU/mL or below had a 3 times (RR, 3.2; CI, 1.8 to 5.7) increased risk of prolonged bleeding after operations compared with women with a clotting factor level of 0.60 IU/mL and above.
Additional treatment during or after surgery due to bleeding problems was necessary in 6% (21 of 370) of the operations performed in carriers and in 2% (6 of 328) of the noncarriers. One or more blood transfusions were required in 11% of operations in participants carrying hemophilia compared with 7% in noncarriers. Other additional treatment consisted of infusion of clotting factor concentrate or a second operation.
After the exclusion of women in whom bleeding problems were not the indication for carrier testing, the risks of prolonged bleeding after operations (RR, 2.8; CI, 1.6 to 5.0) or tonsillectomy (RR, 1.8; CI, 0.9 to 3.4) were similar to the finding in the whole study population. Although obligatory carriers reported bleeding symptoms slightly more often than carriers who could not have been aware of their status prior to testing, these differences did not materially affect the estimates.
Excessive bleeding during menstrual period. Women with lower clotting factor levels more often reported excessive blood loss during the menstrual period (menorrhagia) (Table 5). Similarly, the risk of requiring iron suppletion was 80% increased (RR, 1.8; CI, 0.7 to 5.0) in women with a clotting factor level of 0.40 IU/mL or below compared with women with a clotting factor level of 0.60 IU/mL and above. Sixty-two (23%) women carrying hemophilia visited the general practitioner for excessive bleeding during the menstrual period compared with 20% (n = 47) of noncarriers. Fifty-eight women (31 carriers [11%] and 21 noncarriers [9%]) consulted a gynecologist, and in 18 women a hysterectomy was performed for this reason. Mild to severe restrictions in daily life due to excessive blood loss during the menstrual period were reported by 18% of women with a low clotting factor level compared with 9% of the women with a clotting factor level above 0.60 IU/mL (RR, 2.3; CI, 1.0 to 5.6).
Discussion
Although hemophilia is a well-known bleeding disorder in men, it is seldom recognized that female carriers of hemophilia might not only have an increased bleeding tendency but that the symptoms may be frequent and severe. We studied the risk of bleeding among carriers of hemophilia A or B compared with that of noncarriers. Although usually a level of 0.40 IU/mL is used as the upper limit defining hemophilia, we found an increased risk of bleeding in women with clotting factor levels between 0.41 and 0.60 IU/mL. Carriers of hemophilia experience more spontaneous and provoked hemorrhages than noncarriers, with a higher risk of prolonged bleeding after operations, tooth extractions, and tonsillectomy. The risk is highest in those with the lowest clotting factor levels.
In this study, we approached all women who had been counseled and tested for carriership of hemophilia A or B in the Netherlands. Eighty percent of women responded to the questionnaire. We included 519 women, which makes this currently the largest survey into the hemorrhagic risk in female relatives of men with hemophilia. Nonresponders were somewhat older than the responders. Yet, age did not modify the association between the clotting factor levels and the risk of bleeding. We therefore assume our results to be generalizable to carriers of hemophilia in general. Recall bias may have influenced the reporting of bleeding symptoms, because questions were asked after carrier testing. Yet, Mauser-Bunschoten et al showed by comparing bleeding tendency in obligatory carriers with normal factor VIII levels to noncarriers that the awareness of carrier status has little influence on the reported frequency of bleeding.10 A more serious problem is that women who grew up in families with hemophilia patients may judge bleeding symptoms differently from women in the general population. Selection bias may have been introduced if carrier testing was done because of bleeding problems. To counter this problem as well as the possible incomparability of carriers from hemophilia families to women from the general population, we only included women from families known to be affected by hemophilia. The carriers and noncarriers in our study had grown up in the same environment and had not been aware of their carrier status until testing. Therefore, even if carrier testing was done because of bleeding symptoms, which was the case in 7% of participants, this would not have affected the comparison. In some hemophilia centers, it is routine to measure clotting factor levels in all obligatory carriers. However, despite careful counseling not all carriers are aware of their clotting factor level. Clotting factor levels were missing for 18% of carriers and 43% of noncarriers. Although the group of women in whom clotting factor levels had been measured is most likely to be different from the group in whom these are missing, this will not affect the observed relation between clotting factor levels and bleeding.
Because this is a self-reported questionnaire, bleeding symptoms might have been overreported as well as underreported. In some cases, oozing might have been reported as bleeding. On the other hand, in families where blood loss is a well-known and accepted phenomenon, abnormal bleeding might not have been recognized as such.
Finally, information on the lowest clotting factor activity ever measured was collected from the medical files. We did not have insight into the reasons for these assessments. It is well known that clotting factor levels may vary considerably according to various circumstances (eg, pregnancy and stress). Yet, most investigations were done outside specific risk circumstances. We believe, therefore, that the additional variation in the levels will have had limited effect, although it may have caused an overestimation of risk among the higher clotting factor level categories.
In the literature, mild hemophilia is defined as a clotting factor level of below 0.40 IU/mL. This cutoff point is also described in the guidelines set by the subcommittee of the International Society on Thrombosis and Haemostasis15 (ISTH) and is used in clinical practice. Our study shows that the risk of bleeding is increased in women who would be defined as having mild hemophilia but also in women with clotting factor levels between 0.41 and 0.60 IU/mL. These findings could have implications for the currently used definition of clotting factor levels considered to be “reliable” to perform medical interventions.
We found a moderately increased risk of joint bleedings in carriers. We have no explanation for this; possibly joint bleeds were overreported due to confusion with superficial bleeding of tissue in the joint region. It seems unlikely from clinical practice that this is the true estimate of joint bleeds in carriers.
Our study mainly shows an increased risk of bleeding after trauma and medical interventions, which is similar to the clinical profile of mild hemophilia and in line with a previous study in carriers.10 Our findings underline the importance for clinicians and carriers to be aware of the complications that may occur after operations in carriers of hemophilia. Both the clinician and the carrier should be informed of the clotting factor level, which is strongly related to the hemorrhagic risk.
However, in many carriers the clotting factor levels were either not measured or not known to the woman. It is clear that not only in obligatory carriers, such as daughters of hemophilia patients, but also in potential carriers, clotting factor levels should be measured preceding a medical intervention, also at a young age. The clotting factor levels in carriers are independent of severity of hemophilia within the family and vary from person to person.16 This indicates the importance of clotting factor measurement during carrier testing in all women related to men with hemophilia, independent of the severity of hemophilia and family history unless carrier status is excluded by DNA analysis.
In conclusion, our study suggests a higher risk of bleeding in carriers of hemophilia related to clotting factor levels, especially after medical interventions. This emphasizes the importance of the measurement of clotting factor levels before interventions in all carriers and potential carriers of hemophilia.
Prepublished online as Blood First Edition Paper, March 21, 2006; DOI 10.1182/blood-2005-09-3879.
Supported by the Haemophilia Foundation (Stichting Haemophilia) and the Foundation of Friends of the Netherlands Hemophilia Society (Stichting Vrienden NVHP). responsible for the study concept and design; E.P.M.-B., H.K.P.v.A., J.E.M.v.D.-H., and I.P. acquired data; J.G.v.d.B., F.R.R., I.P., and E.P.M.-B. analyzed and interpreted data; E.P.M.-B., A.H.J.T.B.-V., H.K.P.v.A., J.G.v.d.B., J.E.M.v.D.-H., J.W., F.R.R., and I.P. drafted the manuscript; and J.G.v.d.B., F.R.R., and I.P. were responsible for critical revision of the manuscript for important intellectual content.
An Inside Blood analysis of this article appears at the front of this issue.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
The authors thank the Dutch hemophilia treatment centers from Amsterdam, Rotterdam, Leiden, and Utrecht that provided us with data on clotting factor levels. Dr M. Losekoot provided us with the data on the outcome of DNA analysis. We express our gratitude to all women who participated in our study.