Abstract
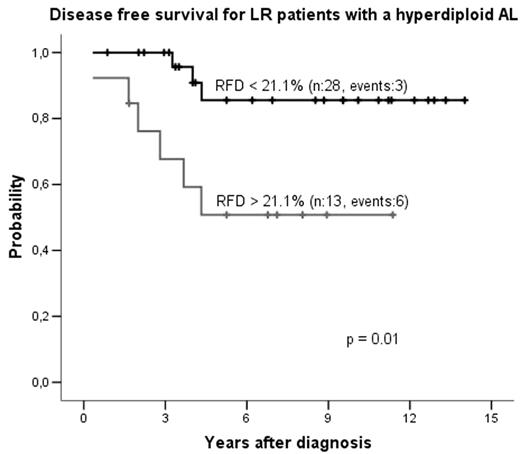
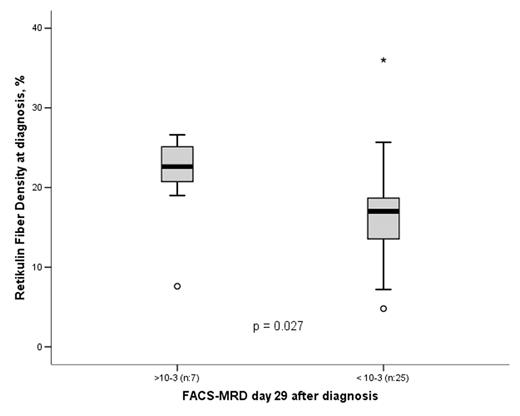
Fibrosis may complicate bone marrow (BM) disease and in its advanced stage negatively affect the outcome of the patients due to BM failure, particularly in myeloproliferative disorders. Studies of the potential importance of BM fibrosis are rare in childhood acute lymphoblastic leukemia (ALL). We have previously shown a prognostic impact of BM fibrosis measured as reticulin fibre density (RFD) at diagnosis in childhood ALL. To further investigate the consequence of BM fibrosis in childhood ALL in relation to immunophenotype, cytogenetic findings and minimal residual disease (MRD) we retrospectively evaluated the RFD in 139 diagnostic BM biopsies from patients with a total mean follow up time of five years and eight months from two childhood oncology centers in Sweden. Patients with pre-B-ALL showed a higher mean RFD (19.1%) compared to patients with T-ALL (11.4%, p < 0.001). This was true also when comparing high-risk (HR) pre-B-ALL patients (18.1%) with the T-ALL patients (p = 0.002). RFD correlated inversely with the white blood cell count in the HR group (r = −0.41, p = 0.009), probably reflecting our finding of low degree of fibrosis in T-ALL. The cytogenetic analysis revealed that for patients with a hyperdiploid ALL (modal chromosome number: 51–61, n: 41) in the low-risk (LR) group, mean RFD was higher for relapsed patients (22.6%) compared to patients in continuous complete remission (17.2%, p = 0.019). The probability of disease free survival for the same group using RFD cutoff of 21.1%, representing the upper third of the material, was 85%±8% for patients with hyperdiploid ALL and low RFD compared to 51%±14% for patients with hyperdiploid ALL and high RFD (p = 0.01, Figure 1). Data for 32 of the patients demonstrated an association between high RFD at diagnosis and high minimal residual disease (MRD) on day 29 after start of treatment. Patients with FACS-MRD > 10−3 day 29 displayed higher mean RFD at diagnosis (21.2%) compared to patients with FACS-MRD < 10−3 (16.7%, p = 0.027, Figure 2). When analyzing the PCR-MRD data day 29 the findings were similar. We conclude that RFD is higher in pre-B-ALL compared to T-ALL, that RFD has prognostic impact in LR patients with hyperdiploid ALL and that high RFD at diagnosis is associated to high MRD on treatment day 29. All these findings are to our knowledge novel, suggesting that evaluation of BM fibrosis at diagnosis is a potentially new therapy stratifying factor and support the need of further research on BM fibrosis in childhood ALL and expanded use of BM biopsy at diagnosis.
Disclosure: No relevant conflicts of interest to declare.
Author notes
Corresponding author