Abstract
Background: FL is an indolent but heterogeneous lymphoid neoplasm with a variable clinical course. Transformation into an aggressive lymphoma is a dominant clinical event that is frequently followed by shorter survival. There is no consistent biological prognostic marker for TR. Recent studies have highlighted the role of the microenvironment in helping to determine the prognosis of FL. However, its impact on TR is largely unknown. In this study we used diagnostic flow cytometry (FC) analysis to assess the role of non-malignant cells in determining OS and TR in FL.
Methods: We identified 567 patients with FL diagnosed at the BCCA over a 5-year period between 1997 and 2001. Of these, 270 cases had diagnostic FC and histological review, of which 137 were nodal and had complete clinical data in our electronic database. FC results were re-analyzed. The antibodies studied included anti-CD3, CD4, CD5, CD8, CD10, CD14, CD19, CD20, CD23, CD45, FMC-7 and IG kappa and lambda light chains. To ensure that biopsies were representative, the sum of the % gated events for CD3 and CD20 had to equal 100% +/− 20%. Light chain restriction was present in all cases and established clonality. The estimate of neoplastic B cells was determined by examining CD19 and CD20 frequency and the ratio of clonal light chain vs non-clonal light chain. Non-neoplastic B cells were estimated using CD19/20 and the amount of non-clonal light chain × 0.5 (λ clonal) or × 2 (κ clonal). Clinical characteristics, different subsets of T cells and the cell content of reactive, non-neoplastic B cells were evaluated using SPSS® software.
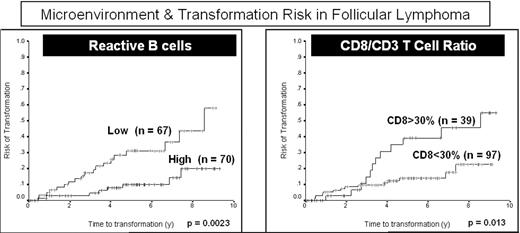
Results: The median age of the 137 patients was 57 years, 51.8% were male and 38.6% had a high IPI (4/5). There were 97 grade 1, 27 grade 2 and 13 grade 3a FL. The median ratio of CD4/CD8 was 4.4. Patients were given a variety of treatments, including observation if asymptomatic, precluding an analysis of progression-free survival. The median follow-up of the living patients was 5.8 years and the estimated 5-year OS and TR were 70% and 20%, respectively. The IPI was predictive of OS (p<0.0001). Two biological variables showed a significant impact on survival. Firstly, cases in which CD8+ cells represented more than 25% of the total (CD3+) T cells had shorter OS (p = 0.028) and increased TR (p = 0.013). The CD8 ratio (p = 0.026) affected OS independently of IPI (p = 0.046). Secondly, cases with a low content of reactive, non-neoplastic B cells, defined by the ratio between IG light chains >1/15 had shorter OS (p = 0.003) and increased TR (p=0.002). The impact of a reduction in normal reactive B cells (p = 0.014) on transformation risk was independent of the IPI (p = 0.05).
Conclusion: Two features of the FL microenvironment studied by diagnostic FC demonstrated an impact on prognosis. The proportion of CD8+ T cells relative to the total T cells and the number of residual, non-neoplastic B cells were both predictors of OS. Importantly, both predict, independently of the IPI, the risk of transformation. These biomarkers are easily measured and may be used to better stratify patients, choose initial treatment options and predict transformation risk in patients with FL.
Microenvironment & Transformation Risk in Follicular Lymphoma
Disclosures: Basic science research support and fellowship support from Roche, Canada.; Honoraria from Roche, Genitope.; Ad Board member for Genitope, Roche, Biogen Idec, Millenium and Lilly.
Author notes
Corresponding author