Abstract
Background: The prognosis of patients with T-cell large granular lymphocyte (LGL) leukemia is diverse, with some patients experiencing rapid progression of the disease while others surviving decades. Despite multiple case reports and a number of case series reported in literature, prognostic factors in this leukemia are unknown and no staging/prognostic system has been developed.
Aim: To identify factors predicting the prognosis of patients with newly diagnosed T-cell LGL leukemia.
Methods: We reviewed the presentation, laboratory data and the clinical course of patients with newly diagnosed T-cell LGL at seen at the Mayo Clinic, Rochester. T-cell LGL was diagnosed in patients with at least 2 of these criteria: morphological evidence of LGL leukemia on bone marrow biopsy or blood smear; LGL immunophenotype; evidence of clonal T-cell receptor gene rearrangements.
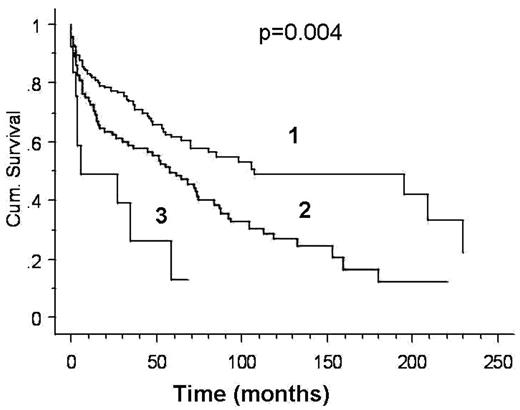
Results: 286 patients seen at Mayo Clinic Rochester between 6/1986 and 5/2005 met diagnostic criteria (52% male, median age at presentation 64 years (range 27–88)). Lymphadenopathy, splenomegaly, and hepatomegaly were present in 9%, 4% and 1.5% of the patients respectively. Median hemoglobin was 11.7 g/dL (range 3.5 – 17.1). Median absolute neutrophil count (ANC) was 1.51 × 109/L (range 0.0 – 20 × 109/L) and median absolute lymphocyte count (ALC) was 2.2 × 109/L (range 0.1 – 24). Median LGL count on peripheral smear was 0.81 × 109/L (range 0.06–10.8 × 109/L). Cytogenetic studies were done for 122 patients, of which, only 9 were abnormal. 87 patients (29%) had associated autoimmune conditions: rheumatoid arthritis (n=29), Felty’s syndrome (n=11), other connective tissue disorders (n=9)). Pure red cell aplasia, aplastic anemia, idiopathic thrombocytopenic purpura and autoimmune hemolytic anemia were seen in 17, 5, 8, 1 patients respectively. Median follow up was 50 months (range 1–229) and estimated median survival was 74.3 months. In multivariate analysis, the only independent risk factors were: anemia (hemoglobin<12 g/dl), hazard ratio (HR) 1.75, (95%CI 1.22–2.52, p= 0.0023), severe neutropenia (<0.1 × 109/L), HR 2.11 (95%CI 1.053–4.25) and lymphopenia (ALC< 1 × 109/L), HR 1.93 (95%CI 1.21–3.07). We developed a simple prognostic scoring system based on the above identified independent risk factors, stratifying patients in 3 groups: 0 - no risk factors present, 1 -one risk factor, 2 - two or more risk factors present. The median survival was 105, 55 and 5 months for score of 0, 1 and 2 respectively, p=0.004 (Figure).
Conclusion: The prognosis of patients with newly diagnosed T-cell LGL is variable. The presence of anemia, severe neutropenia and lymphopenia are independent poor prognostic factors in T-cell LGL. Combining these factors allows the identification of patients at a high risk of death from the disease. Further studies are needed to prospectively validate these findings and establish if the high risk group would benefit from aggressive therapy.
Disclosure: No relevant conflicts of interest to declare.
Author notes
Corresponding author