Abstract
Background: In contrast to the transfusion of red blood cells there is no evidence for stringent rules on ABO-matching in platelet transfusion.
Patients and methods: In a prospective study in pediatric patients we investigated the efficacy of randomly transfused ABO blood group identical and out-of-group (antigen incompatible or antibody [isoagglutinins] incompatible) leukocyte-depleted single donor apheresis platelets (SDP). Four hundred SDP (median, 5/child, range, 1–68) were transfused to 50 children (29 girls and 21 boys, age 0.2 y–18.5 y) with thrombocytopenia due to chemotherapy or aplastic anemia. In the majority, indications for platelet transfusion were not based on platelet counts <5 x 109/L, but were first of all prophylactical; e.g. before lumbar puncture, intramuscular injection, or minor surgery. Exclusion criteria were: splenomegaly, fever ≥38.5°C, major hemorrhage or transfusion reactions. Transfusion efficacy was measured by the 1-hour CCI. (CCI = increase in PLT count [109/L] x body surface area [m2]/number of PLT given [1011]). Expression of A antigen on platelets was assessed by flowcytometry. Accounting for the many patients receiving multiple transfusions, linear mixed effects (LME) analysis was used for univariate and multivariate analyses of the effect of ABO compatibility status on transfusion efficacy.
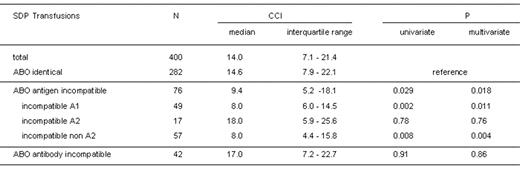
Results: Comparison of data between ABO identical and out-of-group transfusions is summarized in the table.
In addition, by multivariate LME the following parameters were significantly and independently associated with CCI: time since apheresis, apheresis device, volume of SDP, irradiation of SDP, and age of the recipients.
Discussion: CCI after ABO antigen incompatible transfusions was significantly lower compared to identical transfusions (p=0.018, multivariate analysis), particularly after antigen incompatible transfusion of A1 platelets (p=0.011, multivariate analysis). In patients with blood group O or B, transfused platelets expressing high levels of A antigen were rapidly cleared from the circulation as demonstrated by flowcytometry. Because donors with blood group A2 do not express A antigen on their platelets, after transfusion of A2 SDP there was no difference in CCI as compared to ABO identical transfusions (p=0.76, multivariate analysis). This led to a more striking (p=0.004, multivariate analysis) difference of CCI between ABO identical and antigen incompatible transfusions after excluding A2 SDP from the analysis.
Conclusions: If ABO identical SDP are not available, our data strongly support an ABO antigen compatible transfusion strategy for obtaining the best possible CCI - with the only equally effective exception being SDP from A2 donors given to group O or B recipients. However, this would require an extended ABO blood group typing in platelet donors, since by routine typing blood groups A1 and A2 are not differentiated. Although we have not observed significant hemolytic transfusion reactions, ABO antibody incompatible SDP are known to have an inherent risk for it, but relating to CCI they seem to be comparable to ABO identical SDP.
Disclosure: No relevant conflicts of interest to declare.
Author notes
Corresponding author