Abstract
Accurate prediction of venous thromboembolic (VTE) risk remains a clinical challenge, and no prospectively validated risk scoring systems have been described. Recently, a computer-based alert to highlight hospitalised patients at risk of VTE that employed a simple risk score based on eight principal VTE risk factors was shown to improve patient outcome (
The study cohort consisted of all patients who were enrolled in ‘VERITY’ up to 30th November, 2004. VERITY is a UK, prospective VTE treatment registry that enrolls patients presenting to hospital with suspected VTE (www.verityonline.co.uk). The vast majority of patients enrolled have no history of hospitalization and therefore patients will not have been risk assessed or have been given thromboprophylaxis, so essentially reflecting an untreated population.
The risk score was applied to the patient database and a score calculated for each patient for whom all 8 risk factors were known. Risk was scored as previously described: score=3 for cancer, prior VTE, hypercoagulability; score=2 for major surgery; score=1 for age>70 years, BMI>29, bed rest not related to surgery, use of hormone-replacement therapy or oral contraceptives. An increased risk was defined as a cumulative risk score of at least 4.
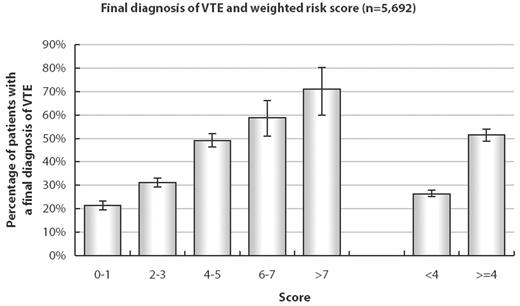
Of 27,179 patients presenting with suspected VTE, 6,124 had a positive diagnosis of deep vein thrombosis, pulmonary embolism, or both; in 15,980 cases the diagnosis was not confirmed. All 8 risk factors were known for 5,692 cases (1880 with confirmed VTE [31%] and 3812 VTE-negative cases [24%]). An increasing risk score was associated with an approximately linear rise in the proportion of patients with confirmed VTE; more than 50% of patients with a risk score ≥4 were diagnosed with VTE, rising to more than 71% in those with a score >7 (see figure).
Although this patient cohort is not identical to the population the risk score was developed for, these data suggest the value of this weighted risk score in identifying those at risk of VTE. Further refinement of this score, perhaps using more sophisticated modeling to increase the accuracy of the score to predict thromboembolic events, would be highly valuable for routine integration of VTE assessment into clinical practice.
Final diagnosis of VTE and weighted risk score (n=5,692)
Disclosures: The VERITY registry is supported by an unrestricted educational grant from Sanofi-Aventis.; The VERITY registry is supported by an unrestricted educational grant from sanofi-aventis.
Author notes
Corresponding author