Abstract
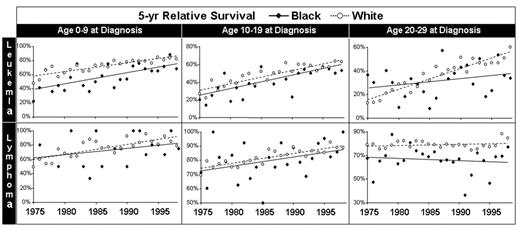
Overcoming disparities in the successful treatment of minority cancer patients has been a major challenge. In particular, blacks/African Americans face a higher likelihood of developing and dying from each of the four most common malignancies in the United States (breast, prostate, colon, and lung cancer) as well as from other cancers. Among children, leukemia and lymphoma have also shown a worse outcome in black patients versus whites. Given the success of the Children’s Oncology Group (COG) in reducing the racial deficit in leukemia and lymphoma, we examined national survival data from the U.S. Surveillance, Epidemiology and End Results (SEER) program for trends in survival difference between white and blacks with leukemia and lymphoma, as a function of age at diagnosis. The annual 5-year relative survival rate trends during 1975 to 2000 for all leukemia and all lymphoma (including Hodgkin lymphoma) showed convergence in white and black children (age <10), comparable trends in 10- to 19-year-olds, and divergence in those 20 to 29 years of age with blacks doing progressively worse than whites. The age dependent patterns were qualitatively similar for acute lymphoblastic leukemia, acute myelogenous leukemia, and non-Hodgkin lymphoma, with convergence in <10 year-olds and divergence in 20- to 29-year-olds apparent in each type of leukemia and lymphoma. For the year 2000, the trends in 20- to 29-year-olds project a 20 to 25% survival deficit for blacks versus whites for acute myelogenous leukemia and a 5 to 10% deficit for other leukemia and lymphomas. The fact that the deficits between white and black patients with leukemia and lymphoma have been overcome for pediatric patients in the United States indicates that this can also be achieved in young adults and older adolescents. A major solution would be access to clinical trials through COG or other clinical trials for the next older age group. The current National Cancer Institute Progress Review Group offers recommendations that are relevant to these disparate outcomes observed in this study; these will be reviewed.
Disclosures: Aaron Viny is a Howard Hughes Medical Institute Medical Research Training Fellow.
Author notes
Corresponding author