Abstract
Recombinant human erythropoietin (rhEpo) has proven to be remarkably safe and effective for treatment of anemias, primarily those secondary to renal disease and malignancy. Despite the worldwide use of rhEpo, concerns about its cost, the need for frequent parenteral administration, and the development of anti-Epo antibodies have prompted development of improved agents to stimulate erythropoiesis. Three strategies appear to be particularly promising. The half-life of Epo in the circulation can be prolonged by the addition of N-linked carbohydrate groups, by formation of adducts with polyethylene glycol, and by preparation of Epo multimers. Second, mimetic peptides can effectively trigger signal transduction at the Epo receptor, thereby boosting red-cell production. Finally, the hypoxia inducible transcription factor (HIF) can be pharmacologically induced by oral agents, resulting in enhanced expression not only of endogenous Epo but also of other genes important in the regulation of erythropoiesis.
Introduction
Recombinant human erythropoietin (rhEpo) is arguably the most successful therapeutic agent spawned thus far by the advent of molecular genetic technology. Since the initial reports 20 years ago demonstrating cure of the anemia of chronic renal failure,1,2 well over a million patients with uremia have been effectively treated, with remarkably few adverse side effects or complications. Amgen, the world's largest biotechnology company, has sold about $22 billion worth of its rhEpo product Epogen and, more recently, about $7 billion worth of darbepoetin alfa (Aranesp), a derivative of rhEpo with a longer half-life (described under “Modifications of full-length rhEpo that prolong plasma survival”). The use of rhEpo has further expanded following its approval by the Food and Drug Administration for the treatment of anemias associated with cancer and AIDS. In addition, rhEpo has been used effectively in the treatment of anemia in myelodysplasia and the anemia of prematurity as well in surgical patients, in both the preoperative and postoperative periods.
Despite the enormous success of rhEpo therapy, there is concern among patients and their physicians that it is costly (often > $10 000/year). The emergence on the market of a less expensive generic rhEpo has been delayed by extended and sequential patents. In addition, many patients object to parenteral administration as often as 3 times a week. Finally, considerable anxiety was engendered from a spate of reports, from 1998 to 2004, of the development of severe pure red-cell aplasia in European patients treated with rhEpo.3,4 However, this complication is now encountered only rarely and was probably caused by defective formulation rather than inherent antigenicity of rhEpo.
Because of these concerns, there is considerable impetus in the pharmaceutical industry to develop less costly agents that match rhEpo in safety and efficacy but are more easily administered, and nonantigenic. This article provides information on new erythropoietic-stimulating agents that aim to meet one or more of these criteria. In order to understand the rationale underlying the design of these agents, it is worthwhile to first briefly review the interaction of Epo with its receptor (EpoR) as well as the regulation of the Epo gene.
Epo–EpoR interaction
Epo is a member of an extensive cytokine family that includes growth hormone, prolactin, interleukins 2 through 7, granulocyte colony-stimulating factor (G-CSF), granulocyte macrophage (GM)–CSF, M-CSF, and others. Although there is very weak sequence homology among these proteins, they have similar numbers of exons and have either been demonstrated or are predicted to fold into a compact globular structure consisting of 4 amphipathic α-helical bundles (see review by Kaushansky and Karplus5 ). Extensive site-directed mutagenesis studies indicate that Epo has 2 domains, primarily located on Helix C and Helix D, that are necessary for binding to the Epo receptor (EpoR).6-10 Subsequent x-ray diffraction analysis of the complex between Epo and the extracellular ligand-binding portion of EpoR (Figure 1A) is consistent with these mutagenesis studies but provides much more detailed information on the binding sites.11 The presence of 2 functionally important domains supports the notion that a single Epo molecule brings 2 EpoR molecules together, thereby initiating a signal transduction cascade. However, x-ray structural analysis of the unliganded extracellular EpoR surprisingly revealed that it too is dimeric but has a very different conformation.12 As shown in Figure 1B, in the absence of Epo the arms of the dimeric extracellular EpoR that attach to the transmembrane domains are splayed apart by a distance of 73 Å. This distance prevents JAK2, which binds to the cytosolic domain of each EpoR polypeptide, from phosphorylating its dimeric partner, and thus the signal transduction cascade is not initiated. Upon binding of Epo, the conformation change in the extracellular domain of dimeric EpoR shortens the transmembrane distance to 39 Å, allowing autophosphorylation and activation of JAK2, thereby triggering the signal transduction cascade necessary for Epo's biologic activity.13
Binding of Epo to its homodimeric receptor and initiation of signal transduction. (A) Crystal structure of the complex of Epo with 2 extracellular domains of EpoR (from Syed et al).11 Red cylinders denote α-helices and green ribbons denote β-sheets. For detailed information on interacting sites in the complex see Syed et al.11 (B) Schematic representation of the conformational change imposed on the dimeric Epo receptor (EpoR) upon binding to Epo. The close proximity off the cytosolic domains of the dimeric EpoR enables autophosphorylation of JAK2 and the initiation of signal transduction. Modified from Remy et al.13
Binding of Epo to its homodimeric receptor and initiation of signal transduction. (A) Crystal structure of the complex of Epo with 2 extracellular domains of EpoR (from Syed et al).11 Red cylinders denote α-helices and green ribbons denote β-sheets. For detailed information on interacting sites in the complex see Syed et al.11 (B) Schematic representation of the conformational change imposed on the dimeric Epo receptor (EpoR) upon binding to Epo. The close proximity off the cytosolic domains of the dimeric EpoR enables autophosphorylation of JAK2 and the initiation of signal transduction. Modified from Remy et al.13
Regulation of the Epo gene
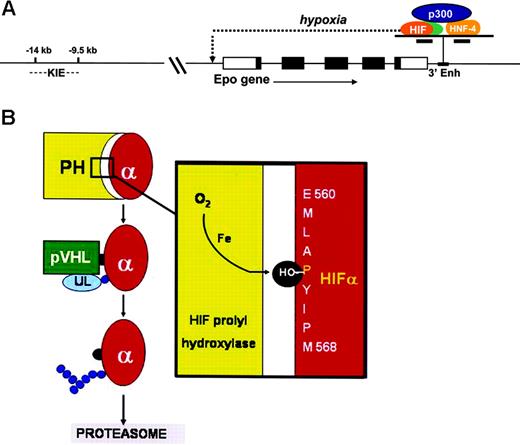
Plasma Epo is produced primarily in the kidney, and to a lesser extent in the liver. The expression of Epo mRNA and protein is regulated primarily at the transcriptional level. The most physiologically important and best understood stimulus for Epo production is hypoxia. Clinicians are familiar with the progessive logarithmic rise in plasma Epo levels in patients with anemias of increasing severity. The marked enhancement of EPO transcription at low oxygen tension is mediated through the hypoxia-inducible transcription factor HIF.14-16 As shown in Figure 2A, this αβ heterodimer binds to a cognate hypoxia response element in a crucial enhancer located just 3′ to EPO's polyadenylation site (3′ Enh). HIF is expressed in nearly all cells and organs and serves as the master orchestrator of oxygen-dependent expression of a number of physiologically important genes. There are 3 highly homologous HIFα subunits with differential tissue specificity and affinity for cognate hypoxia response elements. It is not clear whether the EPO gene is regulated primarily by HIF-1α17 or HIF-2α.18
Hypoxic induction of the Epo gene. (A) The Epo gene has 5 exons, represented by rectangles. The coding regions are shown in black. The 3′ enhancer binds to HNF-4 (hepatic nuclear factor 4) and, in hypoxic cells, to HIF (hypoxia inducible factor). These 2 transcription factors bind cooperatively with the adaptor protein p300. This complex interacts with the Epo promoter, thereby enabling initiation of transcription. Upstream kidney inducible elements (KIEs) are required for enhanced renal expression of Epo. (B) The oxygen-sensing mechanism responsible for the oxygen-dependent degradation of HIF-α. In well-oxygenated cells, HIF-1α protein undergoes oxygen- and iron-dependent hydroxylation at proline 564 and proline 402 (not shown). These posttranslational modifications enable the von Hipple Lindau protein (pVHL) to bind specifically to HIF-α, thereby providing a docking site for the E3 ubiquitin ligase (UL). UL is required for ubiquitylation of HIF-α, resulting in uptake by the proteasome and proteolytic degradation. At low oxygen tension, HIF-α is not hydroxylated and therefore escapes degradation. HIF-α can be activated in oxygenated cells by inhibitors of prolyl hydroxylase (PH) or by iron chelation.
Hypoxic induction of the Epo gene. (A) The Epo gene has 5 exons, represented by rectangles. The coding regions are shown in black. The 3′ enhancer binds to HNF-4 (hepatic nuclear factor 4) and, in hypoxic cells, to HIF (hypoxia inducible factor). These 2 transcription factors bind cooperatively with the adaptor protein p300. This complex interacts with the Epo promoter, thereby enabling initiation of transcription. Upstream kidney inducible elements (KIEs) are required for enhanced renal expression of Epo. (B) The oxygen-sensing mechanism responsible for the oxygen-dependent degradation of HIF-α. In well-oxygenated cells, HIF-1α protein undergoes oxygen- and iron-dependent hydroxylation at proline 564 and proline 402 (not shown). These posttranslational modifications enable the von Hipple Lindau protein (pVHL) to bind specifically to HIF-α, thereby providing a docking site for the E3 ubiquitin ligase (UL). UL is required for ubiquitylation of HIF-α, resulting in uptake by the proteasome and proteolytic degradation. At low oxygen tension, HIF-α is not hydroxylated and therefore escapes degradation. HIF-α can be activated in oxygenated cells by inhibitors of prolyl hydroxylase (PH) or by iron chelation.
At normal oxygen tension the α-subunit of HIF is posttranslationally modified by proline hydroxylation and ubiquitylation, causing it to be rapidly degraded (Figure 2B). Only in hypoxic cells can HIF-α survive, allowing nuclear translocation, αβ dimer assembly, and induction (or repression) of gene expression. The robust hypoxic induction of Epo in kidney and liver is due in part to cooperation in the 3′ enhancer between HIF and HNF-4, a nuclear receptor that is preferentially expressed in these organs (Figure 2A). These 2 transcription factors interact cooperatively with the transcriptional adaptor p300. Moreover, as shown in Figure 2A, the high renal level of Epo expression also depends on an as-yet-uncharacterized cis element in the Epo gene, 9 kb to 14 kb upstream of the promoter.
Modifications of full-length rhEpo that prolong plasma survival
The initial rhEpo and that most commonly administered to date is the full-length unmodified Epo polypeptide, which has an amino acid sequence identical to that of endogenous Epo. Both contain about 40% carbohydrate, although the composition and arrangement of the sugar moieties differ slightly. Both have similar turnover times in the plasma with a t1/2 of about 7 to 8 hours. In contrast, nonglycosylated Epo is very rapidly cleared from the circulation. However, its in vitro erythroid activity and its nonerythroid biologic activity are at least as great as that of native Epo.
Realizing that asparagine(N)-linked glycosylation is an important contributor to the prolonged survival of Epo in the circulation, scientists at Amgen reasoned that engineering additional N-linked sites into the Epo polypeptide might result in a product with an even longer half-life. The product with the most efficacy, darbepoetin alfa (Aranesp), has multiple mutations that create 2 N-linked glycosylation sites, above and beyond the 3 normally present in endogenous Epo. These modifications result in a 3-fold increase in plasma half-life,19 enabling less frequent administration. As mentioned in “Introduction,” this drug is currently in widespread use. In patients with chronic kidney disease, darbepoetin alfa is generally given once every 2 weeks, but even monthly administration is effective.20 In hemodialysis patients the drug is usually given intravenously but in predialysis patients subcutaneous administration, at equivalent dosing, is more convenient and equally effective.21 Darbepoetin alfa is also widely used in cancer patients undergoing chemotherapy, and is comparable to rhEpo in significantly reducing transfusion requirements.22,23 A 3-week dosing interval allows synchronization with most chemotherapy regimens.24 Although there is much less overall experience and reported information in patients with myelodysplasia, darbepoetin alfa is at least as effective as rhEpo in improving anemia and lowering transfusion requirements in a substantial fraction of patients, particularly those with relatively low endogenous plasma Epo levels.25,26 A single dose of darbepoetin alfa has also shown to be effective in the treatment of anemic preterm neonates.27
Three other strategies have been used to prolong the half-life of Epo in the circulation. Recombinant dimeric Epo linked via a flexible peptide bridge28 and rhEpo chemically crosslinked via free sulfhydryl groups to form dimers and trimers29 were both found to have enhanced specific bioactivity and markedly prolonged half-life. Clinical trials have not yet been carried out on these dimeric Epo's.
Scientists at Gryphon Therapeutics have developed synthetic erythropoiesis protein (SEP), which is a fully synthetic 50.8-kDa macromolecule of uniform structure composed of 166-amino-acid polypeptide with a sequence similar to but not identical to that of native Epo. Negatively charged noncarbohydrate precision-length branched polymers have been attached to this protein at 2 sites by chemical ligation.30 SEP has in vitro erythropoietic activity that is considerably greater than that of rhEpo, probably owing to its having an approximately 2.5 prolongation of plasma half-life.
The conjugation of rhEpo to polyethylene glycol results in a product that also has prolonged survival in the circulation.31 Two companies, Prolong Pharmaceuticals and Roche, have developed structurally distinct PEGylated Epo products for therapeutic use. Information is available only on the Roche product.32 The Roche product CERA (Continuous Erythropoietin Receptor Activator) is a 60-kDa molecule, twice the mass of Epo. A methoxy-polyethylene glycol polymer is incorporated into Epo at the N-terminal amino as well as the ϵ-amino of lysine 52 or lysine 45. This modification markedly prolongs the product's half-life in the circulation to about 135 hours in humans after either intravenous or subcutaneous administration. Surface plasmon resonance (Biacore) studies indicate that CERA binds to EpoR more slowly than Epo and that its dissociation (“off”) rate is faster. Thus CERA can trigger the Epo signal transduction cascade without being internalized and has more sustained biologic activity. A single administration of CERA to healthy human volunteers results in a dose-dependent rise in reticulocytes that peaks at about day 7. The agent has few if any significant adverse effects in healthy individuals or in over a thousand patients. No antierythropoietin antibodies have developed to date following CERA treatment. Phase 2 studies have shown impressive erythropoietic responses in patients with chronic renal failure as well as in those with multiple myeloma and non-Hodgkin lymphoma. A phase 3 study is currently under way in patients with non-Hodgkin lymphoma.
In principle, Epo's that have been engineered to have a long half-life should require administration of less protein product and therefore the cost for maintenance therapy should be less. Unfortunately, this is not the case for predialysis patients treated with darbepoetin alfa.33
Small molecule Epo mimetics
In 1996 scientists from Scripps, Affimax, and Johnson Pharmaceutical Research Institute screened a peptide phage library to search for novel sequences that bound to EpoR and possessed biologic activity. Their strategy of using a Cys-X8-Cys insert that could be released by thrombin cleavage resulted in generation of decapeptides capable of dimerizing by means of disulphide bonds. Because of symmetry considerations, the dimeric peptide afforded a greater chance of binding to the dimeric EpoR, thereby enabling triggering of the signal transduction cascade. They found a sequence, CRIGPITWVC, that bound weakly to EpoR (Kd ∼10 mM) and was used as a template for adding random flanking residues as well as internal mutagenesis. After multiple rounds of further screening, they isolated and identified a 20-amino-acid peptide (GGTYSCHFGPLTWVCKPQGG) that bound to EpoR with a Kd of 200 nM and had biologic activity both in vitro and in vivo.34 X-ray analysis of the peptide bound to the extracellular domain of EpoR revealed, for the first time, the dimeric structure of EpoR and demonstrated the docking sites of the dimeric peptide.35 The sequence of this peptide bears no resemblance whatever to that of Epo. However, this strategy offered the opportunity for further structural modifications that might raise its affinity to EpoR approximately 1000-fold, comparable to that of native or rhEpo.
Even if an Epo mimetic peptide had affinity for EpoR close to that of native Epo, its low molecular weight would probably result in rapid urinary excretion, and therefore it would be unlikely to serve as practical or useful therapy. This concern has been addressed by scientists at Affymax, who have developed another peptide with no sequence homology to Epo but with EpoR specificity. This peptide has been PEGylated in order to enhance its stability and prolong its half-life in the circulation. The product, Hematide, has biologic activity both in vitro and in vivo.36 This agent has been shown to be safe in a cohort of 28 healthy human volunteers. One time intravenous administration stimulated erythropoiesis in a dose-dependent manner, with a boost in hemoglobin levels that lasted for at least one month.37 Preliminary results indicate that Hematide is also safe and effective in the treatment of patients with chronic kidney disease.38 Single doses resulted in sustained increments of hemoglobin levels with a return to baseline at approximately 43 days. Interestingly, in comparison to healthy volunteers, a given increment in hemoglobin was achieved in patients with renal failure at half the dose. Hematide is now being evaluated in phase 2 studies both in renal patients and in patients with cancer.
Activation of HIF
As explained in the “Introduction,” in the absence of anemia or other causes of hypoxia, Epo expression in the kidney and liver is suppressed by the oxygen-dependent degradation of the α-subunit of HIF, mediated by prolyl hydroxylation (Figure 2B). Three HIFα prolyl hydroxylases (PHDs) have been cloned and characterized. PHD2 appears to play the dominant biologic role. Inhibition of HIFα prolyl hydroxylation results in increased levels of HIF even in oxygenated cells, and therefore should enhance expression of Epo as well as other HIF responsive genes. Prolyl hydroxylation depends on the presence of oxygen, iron and the cofactor 2-oxoglutarate (Figure 2B). N-oxalylglycine, an analog of 2-oxoglutarate, is a potent inhibitor of prolyl hydroxylation and therefore induces HIF activation.39 During the past decade, scientists at Fibrogen have developed a large series of other inhibitors of prolyl hydroxylases with the aim of preventing formation of hydroxyproline that is essential for stable triple helical collagen. This group of compounds was screened for the ability to up-regulate Epo expression in the Hep3B hepatoma cell line. Several lead compounds markedly induced Epo without any effect on vascular endothelial growth factor, another gene that is normally HIF responsive. One compound (FG-4487) strongly induced the accumulation of HIF-1α and HIF-2α in renal tubular and peritubular cells along with HIF target gene expression in a rat model of acute ischemic renal failure.40 Of considerable interest is the finding that 2 of their lead compounds, FG-2216 and FG-4592, up-regulate other genes besides Epo that are important in erythropoiesis including EpoR, transferrin, transferrin receptor, ferroportin, and the divalent metal transporter 1.41
Oral administration of either FG-2216 or FG-4592 was more effective than parenteral darbepoetin in correcting anemia and reducing hepcidin expression in a rat model of inflammation.42 In healthy human volunteers, dose escalation of another lead compound, FG-2216, resulted in a graded increase in hemoglobin levels with only a modest increase in plasma Epo. A phase 2 dose-escalation study of FG-2216 in patients with chronic kidney disease revealed stimulation of erythropoiesis comparable to standard rhEpo/darbepoetin therapy but, importantly, with plasma Epo levels an order of magnitude lower.43 Thus, it is likely that the coordinated up-regulation of the above-mentioned genes involved in iron mobilization contributes in a major way to the enhanced erythropoiesis. This phenomenon is akin to Chuvash polycythemia in which an Arg200Trp mutation in the VHL protein (Figure 2B) results in constitutive HIF activation and in a marked increase in red-cell mass but often only modestly increased plasma erythropoietin.44
A major concern with the use of this type of drug is whether adverse effects might arise owing to activation or suppression of some of the many other genes known to be regulated by HIF. For example, might the drug trigger unwanted vascular neogenesis? Even more concerning is the possibility that the drug may induce or aggravate neoplasia. The fact that HIF is constitutively expressed in many cancers, particularly metastatic ones,45 raises the specter of enhanced tumor growth in the presence of a drug that activates HIF. These concerns seem to be at least partially addressed by the finding that FG-4592 and FG-2216 are remarkably specific for up-regulation of Epo and a family of other genes that regulate erythropoiesis. Indeed, in 5 different mouse models of lung or colon cancer, FG-2216 corrected the anemia but tumor growth was not enhanced and may have been retarded.46 The specificity of these agents may be based on differential inhibition of the 3 PHDs and/or differential activation of the 3 HIFα subunits. Clinical trials are under way to assess the safety and efficacy of these agents in different types of anemias. In addition to inhibitors of prolyl hydroxylase, HIF may also be activated by iron chelation, both in vitro and in vivo.47 It is worth noting that patients with transfusional iron overload on chronic iron chelation therapy, like those with Chuvash polycythemia, have not evinced any apparent increase in tumor development.
The development of a potentially inexpensive small-molecule oral agent with erythropoietic specificity offers obvious therapeutic advantages.
Concerns and caveats
During the development of rhEpo it was initially believed that the expression of EpoR was limited to erythroid progenitors and therefore Epo therapy would have a high degree of specificity with few if any nonerythropoietic effects. However, it has become increasingly apparent that EpoR is present on a wide range of cells and that high (pharmacologic) doses may result in diverse sequelae at sites outside of the erythron.48 Possible beneficial effects include protection of the central and peripheral nervous system, myocardium, and other tissues against injury. Modification of Epo by removal of sialic acid, which greatly shortens its half-life in the circulation, has been shown to be neuroprotective in models of cerebral ischemia, spinal cord compression, and sciatic nerve injury with no significant stimulation of erythropoiesis.49 In like manner, Epo modified by carbamylation lacks erythropoietic activity but prevents cardiomyocyte loss in a model of myocardial infarction.50 In nonerythroid cells, EpoR is present in much lower abundance. It is likely that in these cells Epo and the modified Epo's mentioned above bind to a heterodimer consisting of EpoR and the common cytokine β receptor.51
The potential and proven beneficial nonerythroid effects of Epo notwithstanding, there is concern that chronic administration of pharmacologic doses of rhEpo could have several types of deleterious consequences including neovascularization, thrombosis, and enhancement of cancer growth.
Among its many nonerythropoietic effects, Epo stimulates proliferation and migration of vascular endothelial cells in vitro and promotes angiogenesis.52,53 Epo may contribute to the pathogenesis of proliferative diabetic retinopathy. Levels of both Epo and vascular endothelial growth factor (VEGF) were markedly higher in the vitreous fluid of these patients than in those with nondiabetic ocular disease.54 Epo levels were more strongly associated with proliferative vessel disease compared with VEGF. Inhibition of both Epo and VEGF greatly retarded the growth of bovine retinal microvascular cells.
During the early days of treating hemodialysis patients with rhEpo, one of the uncommon complications was thrombosis, particularly in arteriovenous shunts or fistulas. This problem was thought to be due to excessive dosing, with hematocrit levels rising to the mid- or high 40s. However, rhEpo may pose a thrombotic risk independent of its effect on the red-cell mass. Administration of rhEpo to dogs resulted in a decline in platelet count but enhanced platelet reactivity,55 and promoted development of thrombus in those with an arteriovenous shunt.56 In healthy human volunteers, intravenous administration of rhEpo (100 U/kg or 500 U/kg) resulted in a 10% to 20% increase in platelet count as well as activation of both platelets and the endothelium.56 However, the rise in platelets may be due in part to induction of iron deficiency owing to the increase in red-cell mass.58 Cancer patients are inherently predisposed to thrombosis. This complication may be enhanced in those treated with rhEpo. In a retrospective review of 9353 cancer patients who participated in 57 trials, the administration of rhEpo or darbepoetin alfa significantly reduced the need for red-cell transfusions but increased thrombo-embolic events with a relative risk ratio of 1.67.23
It is not surprising that the many organs and tissues that express EpoR include a wide variety of human malignancies, both solid tumors and leukemias.48 In some animal tumor models, inhibition of Epo binding to EpoR has resulted in tumor regression.59,60 A multicenter trial of patients with breast cancer treated with chemotherapy was terminated early because of increased mortality in the first 4 months of those also treated with rhEpo.61 In a double-blind, placebo-controlled study of 351 patients with head and neck cancer, those receiving rhEpo had higher hemoglobin levels than those given placebo, but had significantly greater cancer progression and lower survival.62 In contrast to these studies, Hedenus et al63 found that darbepoetin alfa therapy had no effect on tumor progression (overall survival or disease-free survival) in 314 patients with lung cancer and 344 patients with lymphoma.
Fear of adverse effects from high doses of rhEpo is somewhat allayed by the fact that patients with severe chronic anemias do not appear to have complications that can plausibly be attributed to levels of circulating Epo that are often 100 times normal. Concern about nonerythroid effects of Epo therapy would be minimized by the agents described above that activate HIF and achieve sustained and efficient enhancement of erythropoiesis despite only a modest increase in plasma Epo.
Conclusions
A reasonably full understanding of the regulation of the Epo gene as well as the interaction of Epo with EpoR has permitted fruitful exploration of rational strategies for the development of new erythropoietic agents that match rhEpo in safety and efficacy but are easier to administer, better tolerated, and, hopefully, much less costly. Within the next few years one or more of these agents are likely to be in widespread use around the world.
Authorship
Conflict-of-interest disclosure: The author declares no competing financial interests.
Correspondence: H. Franklin Bunn, Hematology Division, Brigham and Women's Hospital, Harvard Medical School, Boston, MA 02115; e-mail: hfbunn@rics.bwh.harvard.edu.