Abstract
Although imatinib induces marked responses in patients with chronic myeloid leukemia (CML), resistance is increasingly problematic, and treatment options for imatinib-resistant or -intolerant CML are limited. Dasatinib, a novel, highly potent, oral, multitargeted kinase inhibitor of BCR-ABL and SRC family kinases, induced cytogenetic responses in a phase 1 study in imatinib-resistant or -intolerant CML and was well tolerated. Initial results are presented from a phase 2 study of 186 patients with imatinib-resistant or -intolerant chronic-phase CML (CML-CP) designed to further establish the efficacy and safety of dasatinib (70 mg twice daily). At 8-months' follow-up, dasatinib induced notable responses, with 90% and 52% of patients achieving complete hematologic and major cytogenetic responses (MCyR), respectively. Responses were long lasting: only 2% of patients achieving MCyR progressed or died. Importantly, comparable responses were achieved by patients carrying BCR-ABL mutations conferring imatinib resistance. Dasatinib also induced molecular responses, reducing BCR-ABL/ABL transcript ratios from 66% at baseline to 2.6% at 9 months. Nonhematologic adverse events were generally mild to moderate, and most cytopenias were effectively managed with dose modifications. Cross-intolerance with imatinib was not evident. To conclude, dasatinib induces notable responses in imatinib-resistant or -intolerant CML-CP, is well tolerated, and represents a promising therapeutic option for these patients. This trial was registered at www.clinicaltrials.gov as CA180013.
Introduction
Chronic myeloid leukemia (CML) is a hematopoietic disorder that typically first appears as a benign, extended chronic phase (CP), and progresses, usually via an accelerated phase, to fatal blast crisis over 3 to 5 years.1 CML is defined by the presence of the BCR-ABL fusion gene, which results from the translocation of the long arms of chromosomes 9 and 22 to form the Philadelphia (Ph) chromosome.1,2
Treatment with imatinib (Glivec; Novartis, Basel, Switzerland), a selective inhibitor of BCR-ABL tyrosine kinase, induces hematologic and cytogenetic responses; however, the occurrence of resistance to imatinib is now well described.3–5 Such resistance is frequently associated with BCR-ABL point mutations, particularly in CML-CP6 ; however, BCR-ABL–independent mechanisms of resistance have also been identified, including dysregulation of SRC family kinases (SFKs).7,8 Furthermore, imatinib intolerance is also recognized as a treatment concern. The most recent update of the International Randomized study of Interferon-α plus cytarabine versus STI571 (imatinib) (IRIS) indicated that approximately 30% of the 553 imatinib-treated patients with CML-CP recruited had discontinued imatinib as a result of an unsatisfactory therapeutic effect, adverse event(s), switch to alternative agents, or other reasons after 4.5 years of follow-up.5 The lack of attaining cytogenetic and molecular responses correlated with long-term outcomes,5 and yet current alternative treatment options for patients with imatinib-resistant or -intolerant CML-CP are extremely limited. The use of allogeneic stem cell transplantation (SCT), although potentially curative, is restricted because of the availability of suitable donors and not insignificant SCT-related morbidity and early mortality.9–11
Dasatinib (SPRYCEL, formerly BMS-354825; Bristol-Myers Squibb, New York, NY) is a novel, oral, multitargeted kinase inhibitor that is active against BCR-ABL and SFKs. Dasatinib binds to multiple conformations (active and inactive) of the ABL kinase,12 is active against 21 of 22 tested BCR-ABL mutations conferring imatinib resistance, and potently inhibits the SFKs implicated in imatinib resistance.13–15 In vitro, dasatinib has a 325-fold greater potency compared with imatinib in cells transduced with unmutated BCR-ABL.13,14 In a phase 1, open-label, dose-escalation study, dasatinib induced major cytogenetic responses (MCyRs) and was generally well tolerated in patients with all phases of imatinib-resistant or -intolerant CML and with Ph-positive acute lymphoblastic leukemia (ALL).16
The primary objective of this phase 2 study was to estimate the MCyR rate with dasatinib treatment in patients with imatinib-resistant CML-CP. Results from a formal interim analysis conducted with 6-months' follow-up are summarized for the initial 186 patients in tabular format only; data from a subsequent analysis conducted on the same patient cohort, extending the follow-up to a minimum of 8 months, form the basis for this report. In late June 2006, the United States Food and Drug Administration, based partly on this dataset, granted approval for dasatinib in the treatment of imatinib-resistant and -intolerant chronic myelogenous leukemia. We believe that making these data available to hematologists at this time, although incomplete, will be helpful in advising patients of available treatment options.
Patients, materials, and methods
Study design and patient eligibility
This was an open-label, single-arm, phase 2 study conducted in 20 countries worldwide; patients were enrolled between February and May 2005. Written, informed consent was obtained from every patient prior to their participation in this trial. The study was conducted in accordance with the Declaration of Helsinki and was consistent with International Conference on Harmonization Good Clinical Practice (ICH GCP) and applicable regulatory requirements. The protocol was reviewed and approved by a recognized ethics review committee at each trial center.
Patients, aged at least 18 years, were eligible for entry if they had imatinib-resistant or -intolerant CML in CP. Chronic-phase CML was defined as less than 15% blasts in peripheral blood and bone marrow, less than 20% basophils in peripheral blood, less than 30% blasts plus promyelocytes in peripheral blood and bone marrow, platelets at least 100×109/L unless thrombocytopenia was due to recent therapy, and no extramedullary involvement other than in the liver or spleen. Patients with prior accelerated-phase or blast crisis CML were not eligible. The imatinib-resistant population included patients with progressive CML-CP on imatinib greater than 600 mg/day or those who had resistance to imatinib no more than 600 mg/day and BCR-ABL mutations associated with high-level imatinib resistance (cellular IC50 ≥ 1325 nmol/L; M244V, G250E, Q252H, Y253H, E255K/V, T315I, F359V, H396R).14 Imatinib resistance was defined as a lack of complete hematologic response (CHR) after 3 months of imatinib treatment, a lack of any cytogenetic response after 6 months of treatment, a lack of a MCyR (Ph-positive cells > 35%) after 12 months of treatment, an increasing white blood cell (WBC) count on at least 2 consecutive occasions (with a doubling of the count from the nadir to ≥ 20×109/L or an absolute increase of ≥ 50×109/L), or a relapse after a CHR or MCyR. Imatinib intolerance was defined as at least grade 3 nonhematologic toxicity, or grade 4 hematologic toxicity persisting for more than 7 days, related to imatinib at any dose.
Exclusion criteria included, but were not limited to (1) prior dasatinib therapy, (2) imatinib therapy within 7 days of initiation, (3) an Eastern Cooperative Oncology Group (ECOG) performance status greater than 1, (4) uncontrolled or significant cardiovascular disease, or (5) a history of a significant bleeding disorder unrelated to CML.
Treatment with dasatinib
Patients received an oral dose of 70 mg dasatinib twice daily. Therapy could be interrupted or reduced to 50 mg twice daily or 40 mg twice daily in response to hematologic toxicity of at least grade 3 or some nonhematologic toxicity events of at least grade 2. Treatment was then reinitiated at the previous dose, at a reduced dose level, or discontinued altogether, depending on the severity of the adverse event and on the number of times the same event had occurred. In addition, dose reduction or discontinuation decisions were made by the investigator and sponsor for patients with any sign of bleeding or hemorrhage of any grade. Escalation to 90 mg dasatinib twice daily was permitted for patients who had (1) disease progression, even after an initial response; (2) no CHR after 8 weeks; or (3) no MCyR after 12 weeks. Study drug was administered until withdrawal from the study, intolerable toxicity, or progression of CML despite dose escalation.
CML therapies other than dasatinib were prohibited on-study. Exceptions included anagrelide and hydroxyurea for the treatment of elevated platelet (> 700×109/L) and WBC counts (> 50×109/L), respectively; usage was limited to 2 weeks. Administration of colony-stimulating factors and recombinant erythropoietin was also permitted at the discretion of the investigator.
Patient evaluation
Cytogenetic and hematologic responses to dasatinib were monitored by bone marrow aspirates or biopsies (conducted every 12 weeks) and complete blood counts (once weekly for the first 12 weeks, and every 3 months thereafter). Assessment of study drug toxicities was continuous and included a physical examination to monitor adverse events, conducted weekly for the first month and every 4 weeks thereafter. Peripheral blood cell mRNA was collected and analyzed for BCR-ABL gene point mutations by denaturing high-performance liquid chromatography (D-HPLC) and sequencing and for the level of expression by quantitative reverse transcriptase–polymerase chain reaction (Q-RT-PCR). To determine molecular responses to dasatinib, BCR-ABL transcripts in peripheral blood were evaluated using Q-RT-PCR at baseline and every month on study and compared with levels of total ABL transcripts.
Cytogenetic responses were based on the prevalence of Ph-positive metaphases among at least 20 metaphase cells in each bone marrow sample. The criteria for cytogenetic responses according to the percentage of Ph-positive cells in metaphase in bone marrow were as follows: complete cytogenetic response (CCyR), 0%; partial cytogenetic response (PCyR), 1% to 35%; minor cytogenetic response, 36% to 65%; minimal cytogenetic response, 66% to 95%; no cytogenetic response, 96% to 100%. The rate of MCyR was defined as the number of CCyRs plus the number of PCyRs of all treated patients.
To be classified as achieving a CHR, a patient had to meet all of the following criteria: (1) WBC count no more than the institutional upper limit of normal, (2) absolute neutrophil count (ANC) at least 1×109/L, (3) platelet count less than 450×109/L and no more than the institutional upper limit of normal, (4) no blasts or promyelocytes in peripheral blood, (5) less than 5% myelocytes plus metamyelocytes in peripheral blood, (6) less than 2% basophils in peripheral blood, (7) no extramedullary involvement (including no hepatomegaly or splenomegaly). Hematologic responses were required to be maintained for at least 4 weeks.
Statistical analysis
Analysis of efficacy parameters was performed for all patients receiving at least one dose of dasatinib. Hematologic and cytogenetic response rate 95% confidence intervals were estimated. Duration of MCyR was estimated via the Kaplan-Meier product-limit method and was measured from the first day the criteria were met until the date treatment was discontinued as a result of progressive disease or death. Patients who discontinued for other reasons were censored on the date of their last cytogenetic assessment. Two-sided, 95% confidence intervals for median duration of MCyR were computed using the method of Brookmeyer and Crowley.17 All safety and laboratory observations were analyzed descriptively, with adverse events graded according to the National Cancer Institute Common Toxicity Criteria (NCI CTC) Version 3.0.
Results
Patient demographics and disease characteristics
A total of 387 patients [196 women, 191 men; median age, 58 years (range, 21-85 years)] were enrolled into this study between February and July 2005 and treated in 75 centers worldwide. Results presented are for the initial cohort of 186 patients: 127 with imatinib-resistant and 59 with imatinib-intolerant CP-CML.
Patient demographics and baseline disease characteristics were representative of the broader patient population with imatinib-resistant or -intolerant CP-CML; the efficacy and safety results from this study should therefore be directly applicable to the broader target population. Patients had a median duration of CP-CML of 64 months, although this was markedly longer for patients with imatinib-resistant disease than those with intolerance to imatinib (median, 77 versus 26 months). Patients were heavily pretreated, with 70% having received prior interferon-α, 42% prior chemotherapy, and 9% stem cell transplantation (Table 1).
The majority of patients with imatinib-resistant disease (73%) had received imatinib at daily doses exceeding 600 mg/day. Primary reasons for imatinib intolerance included grade 3 to 4 rash [22 patients (37%)], hepatotoxicity [17 (29%)], arthralgias [13 (22%)], gastrointestinal events [6 (10%)], and edema [5 (8%)].
Median duration of dasatinib therapy for all treated patients was 8.3 months (range, 0.03-11.0 months), at which time 143 patients (77%) remained on study. The median dasatinib dose was 101 mg/day (range, 18-149 mg/day).
Of the 43 patients who had discontinued treatment, 16 (9%) discontinued because of study drug toxicity, 12 (6%) as a result of disease progression, 6 (3%) because of an adverse event unrelated to dasatinib, 4 (2%) because of patient request, 2 (1%) as a result of death, and 3 (2%) as a result of other reasons (Table 1).
Efficacy
Complete hematologic responses were observed in 168 of 186 patients (90%) treated with dasatinib (95% CI, 85.1%-94.2%] (Table 2); rates of CHR were 87% (95% CI, 80.3%-92.6%) and 97% (95% CI, 88.3%-99.6%)] for imatinib-resistant and imatinib-intolerant disease cohorts, respectively. These response rates proved to be long-lasting (range, 1.1+ to 10.6+ months), with 7 (6%) of the 111 patients with imatinib-resistant disease and 1 (2%) of 59 patients with imatinib-intolerant CP-CML who achieved a CHR with dasatinib subsequently progressing.
Dasatinib induced notable cytogenetic responses in patients with CP-CML who were resistant to, or intolerant of, imatinib therapy. MCyRs were evident in 97 (52%) of 186 patients (95% CI, 44.7%-59.5%) (Table 2): 50 (39%; 95% CI, 30.8%-48.4%) of 127 patients with imatinib-resistant disease and 47 (80%; 95% CI, 67.2%-89.0%) of 59 patients who were unable to tolerate imatinib. Subsequent analysis revealed that 38% of patients with no prior cytogenetic response to imatinib and 44% of patients who had received doses of imatinib exceeding 600 mg/day achieved MCyRs with dasatinib.
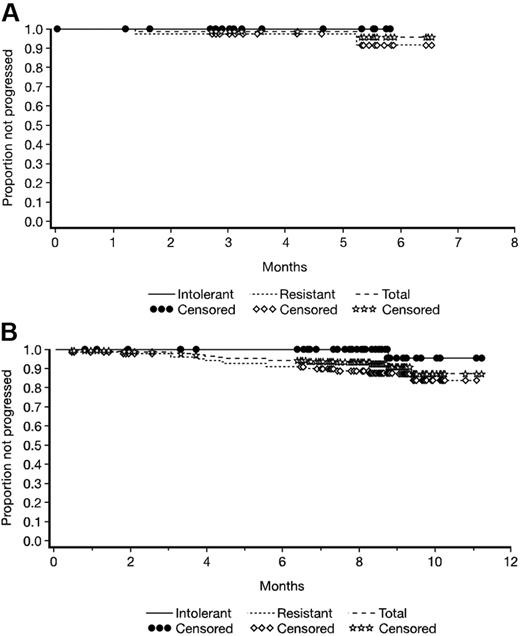
Major cytogenetic responses were long lasting; responses with dasatinib were maintained in 96% of patients with imatinib-resistant disease and 100% of patients with imatinib-intolerant CP-CML (Figure 1A).
(A) Duration of major cytogenetic response associated with dasatinib treatment and (B) progression-free survival with dasatinib for the total treated population and imatinib-resistant and -intolerant CML subgroups, with a minimum of 8-months' follow-up.
(A) Duration of major cytogenetic response associated with dasatinib treatment and (B) progression-free survival with dasatinib for the total treated population and imatinib-resistant and -intolerant CML subgroups, with a minimum of 8-months' follow-up.
Marked molecular responses were also evident with dasatinib. The median ratio of BCR-ABL to ABL transcripts, as determined by Q-RT-PCR, fell from 66% at baseline (n = 149) to 2.6% (n = 26) at 9-months' follow-up (Figure 2).
Molecular response to dasatinib treatment depicted as ratio of BCR-ABL to ABL transcript, as measured by Q-RT-PCR.
Molecular response to dasatinib treatment depicted as ratio of BCR-ABL to ABL transcript, as measured by Q-RT-PCR.
The progression-free survival rate was 92.4% (Figure 1B). After a minimum of 8-months' follow-up, 15 patients (8%) with imatinib-resistant disease and 1 patient (0.5%) with imatinib-intolerant CML-CP had experienced disease progression or had died. Nine of these 16 patients had shown evidence of a response prior to progression (Table 1; Figure 1–2).
Analysis of efficacy by baseline BCR-ABL mutational status
Baseline analysis of the ABL kinase domain failed to identify the presence of any imatinib-resistant mutation in 107 (59%) of the 180 patients for whom such analyses were performed by the central laboratory (Table 3): 56 (46%) of 122 patients with imatinib-resistant disease and 51 (88%) of 58 patients who were unable to tolerate imatinib. In the remaining 73 patients (41%), 26 distinct imatinib-resistant mutations were observed; in 46 of these patients, these mutations were associated with moderate to very high resistance to imatinib (≥ 5-fold increase in cellular IC50 compared with unmutated BCR-ABL).
Cytogenetic and hematologic responses were observed broadly across all BCR-ABL genotypes; only one mutation, T315I, identified in 2% of patients precluded patients attaining MCyR or CHR (Table 3).
Safety
Dasatinib was generally well tolerated, with only 16 patients (9%) having discontinued treatment as a result of adverse events at 8-months' follow-up. Incidences of events were comparable for the imatinib-resistant and -intolerant CP-CML cohorts.
Cytopenias were common but were generally reversible and could be managed effectively with dose adjustments (reductions or temporary interruptions). Packed cell and platelet transfusions were administered to 22% and 31% of patients, respectively.
Nonhematologic events, considered by the investigator to be related to dasatinib therapy, were generally mild to moderate in intensity (grades 1 or 2); headache, gastrointestinal disorders (diarrhea, nausea), fatigue/asthenia, and dyspnea were the most common (Table 4). Dose reductions or interruptions were used effectively to treat cases of neuropathy, dyspnea, elevated activity of liver enzymes (primarily alanine aminotransferase), headache, bone pain, rash, renal failure, cardiac abnormality, and diarrhea. Six patients (3%) experienced grade 3 to 4 pleural effusions; in general, however, most cases of pleural effusion were uncomplicated, resolving with temporary dose interruption, diuretics, or, in some cases, pulse steroids.
The majority of the serum chemistry changes observed with dasatinib were also mild to moderate in intensity (grade 1 or 2) (Table 4); grade 3 to 4 elevated activity of ASAT was seen in 4 patients (2%) and 3 patients (2%) experienced grade 3 to 4 elevated activity of ALAT. Asymptomatic, transient hypocalcemia was reported in patients presenting with normal calcium levels at baseline; these events tended to resolve spontaneously during continued treatment (Table 4).
Discussion
The results of this phase 2 study demonstrate the efficacy and tolerability of dasatinib in patients with imatinib-resistant or -intolerant CML-CP. Responses were seen in a substantial proportion of patients. The high rate and durability of MCyR reported in the present study is of particular note, because several studies with other agents have shown MCyR to be predictive of long-term survival.18,19 In addition, because the extent of BCR-ABL/ABL transcript reduction achieved early in the course of therapy is an indicator of subsequent response,20 it is significant that marked molecular responses were also achieved with dasatinib therapy (Figure 2). Furthermore, the major molecular response rate for imatinib in this population is predicted to be zero.
Patients who develop imatinib-resistant or -intolerant CML-CP have few therapeutic options, and those that are available have substantial limitations. The efficacy of dasatinib in the heavily pretreated patients in this study is of note, as this may represent a population particularly refractory to treatment. Moreover, consistent with preclinical observations,13,14 dasatinib treatment led to responses even in the presence of documented imatinib-resistant mutations in the BCR-ABL kinase domain. Mutations associated with clinical imatinib resistance have been identified at in excess of 25 amino acid positions. Both the P- and A-loops undergo large conformational shifts on binding of imatinib to BCR-ABL; mutations that hinder these shifts can prevent imatinib binding, resulting in imatinib-resistant CML.21 A smaller proportion of mutations directly interfere with drug binding.21 In patients with mutations associated with high resistance to imatinib (cellular IC50 ≥ 1325 nmol/L; M244V, G250E, Q252H, Y253H, E255K/V, F317L, F359V, H396R),14,22–24 response rates to dasatinib were comparable to rates for the total treated population. Dasatinib lacked activity in patients with the T315I mutation, all with imatinib-resistant disease. The failure of all 3 patients with the T315I mutation to achieve MCyR or CHR is consistent with previous clinical and preclinical observations describing the resistance of this mutation to ATP-competitive BCR-ABL inhibitors, including imatinib and nilotinib.14,21,25
The observation that 46% of patients with imatinib-resistant CML-CP in this study did not carry imatinib-resistant BCR-ABL mutations indicates that other mechanisms of resistance may also exist (although the looser definition of resistance in this study may explain why kinase domain mutations were detected less frequently). Alternative mechanisms reported include amplification of the BCR-ABL gene, overexpression of the P-glycoprotein efflux pump (of which imatinib is a substrate), dysregulation of SFK activity, and activation of other pathways (eg, mTOR, p53, aneuploidy).7,8,26–29 The mechanism by which dasatinib induces MCyR and CHR in these patients remains to be determined, but this could be due to the greater potency of BCR-ABL inhibition of dasatinib versus imatinib and/or the ability of dasatinib to also potently inhibit SFKs.
Dasatinib was generally well tolerated in this study. Approximately one third of the patients had imatinib-intolerant CML-CP, but the vast majority of these patients were able to tolerate dasatinib. No relationship was evident between the duration of treatment and either the nature or intensity of AEs reported, suggesting a lack of cumulative toxicity for dasatinib. Only 7% of patients with imatinib-intolerant CML-CP discontinued treatment at 8-months' follow-up because of dasatinib-related toxicity, suggesting a lack of cross-intolerance between dasatinib and imatinib.
These data demonstrate that dasatinib is well tolerated and highly effective in overcoming resistance and intolerance to imatinib, inducing long-lasting cytogenetic and hematologic responses in patients with imatinib-resistant and -intolerant CML-CP, and molecular responses in a highly resistant group of patients. Dasatinib activity is also being investigated in patients with previously untreated CML, including a study that randomly assigned such patients to either dasatinib or imatinib. On the basis of clinical experience to date, dasatinib has the potential to have a large impact on the current treatment paradigm for patients with CML-CP with resistance or intolerance to prior therapy, including imatinib.
Authorship
Contribution: A.H. and N.P.S. designed and performed research, analyzed data, and wrote the paper; H.M.K. designed and performed research and analyzed data; M.B., J.H.L., D.N., and T.P.H. performed research and analyzed data; J.F.A., B.J.D., T.F., S.L.G., F.C., R.T.S., and R.M.S. performed research; M.C.M. performed research, contributed vital new reagents or analytical tools, and analyzed data; R.E. designed and performed research, contributed vital new reagents or analytical tools, analyzed data, and wrote the paper; A.M.C. analyzed data.
Conflict-of-interest disclosure: All authors have received financial support from Bristol-Myers Squibb. A.H. has received research support and honoraria from Bristol-Myers Squibb; H.M.K. has received a research grant from Bristol-Myers Squibb and Novartis; B.J.D. is a principal investigator on several Bristol-Myers Squibb and Novartis trials and has received institutional funding for trial expenses; B.J.D. has also acted as an advisor for Bristol-Myers Squibb and has a patent submitted on Bcr-Abl kinase mutations; R.E. and A.M.C. are employees of Bristol-Myers Squibb; N.P.S. has received honoraria and served as a consultant for Bristol-Myers Squibb.
Correspondence: Andreas Hochhaus, III. Medizinische Klinik, Medizinische Fakultät Mannheim, Universität Heidelberg, Theodor-Kutzer-Ufer 1-3, 68167 Mannheim, Germany; e-mail: hochhaus@uni-hd.de.
An Inside Blood analysis of this article appears at the front of this issue.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
In addition, the following primary investigators participated in this trial. Australia: C. Arthur, S. Branford (molecular analyses), A. Grigg, J. Seymour, K. Taylor; Austria: P. Valent; Belgium: A. Bosly; Canada: D. Forrest, P. Laneuville, C. Gambacorti-Passerini; Denmark: J. Lanng-Nielsen; Finland: K. Porkka; France: H. Dombret, F. Guilhot; J.-L. Harrousseau, F. Maloisel, M. Michalet, J. Reiffers, P. Rousselot; Germany: U. Berger, C. Bokemeyer, P. Erben (molecular analyses), T. Fischer, M. Schatz; Ireland: E. Conneally, M. O'Dwyer, Israel: A. Nagler; Italy: S. Amadori, F. Ferrara, G. Lambertenghi, V. Liso, B. Rotoli, G. Saglio; Korea: D.-W. Kim; Netherlands: J. Cornelissen, A.V.M.B Schattenberg; Peru: J. Navarro; Singapore: Y.T. Goh; Spain: J. Odriozola, J.L. Steegmann; Sweden: M. Ekblom, B. Markevarn, B. Simonsson, L. Stenke; Switzerland: A. Gratwohl, United Kingdom: T. Holyoake; United States: K. Bhalla, S. Bilgrami, B. Cheson, R. Collins, S. Coutre, J. Dipersio, S. Durham, L. Fehrenbacher, J.K. Giguere, F.A. Greco, H.J. Khoury, R. Larson, M. Lilly, J. Lister, S. Luger, A. Maniam, J. McGuirk, E. Merriam, M.S. Murali, C. Nicaise, J. Radich (molecular analyses), A. Rapoport, C.E. Rivera, C. Schiffer, R. Strair, M. Talpaz, M. Voi.
This work was supported by research funding from Bristol Myers Squibb. Editorial support for this manuscript was funded by Bristol-Myers Squibb.