Abstract
Background: Extranodal status is one of the five key factors in the International Prognostic Index (IPI) for diffuse large B-cell lymphoma (DLBCL). We have re-examined the prognostic utility of extranodal involvement in DLBCL patients by determining whether the number and location of extranodal sites correlate with survival, particularly in the post-rituximab era.
Methods: Using the Lymphoid Cancer Database of the British Columbia Cancer Agency, all patients with a diagnosis of DLBCL were included between January 1979 and May 2006 except those who were less than age 18 at diagnosis, HIV positive, presented with disease in the testicular or central nervous system, had discordant indolent lymphoma at or before diagnosis, or did not receive any chemotherapy. Any degree of extranodal involvement was recorded as positive for extranodal disease and all sites of involvement were documented.
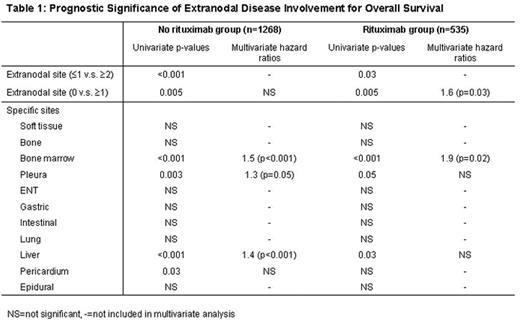
Results: 1803 patients were identified with the following characteristics: median age 62 (range 19–93), male 58%, stage III/IV 49%, elevated LDH 51% and performance status ≥2 34%. Of the 1268 patients treated without rituximab, 358 (28%) had only nodal disease, 532 (42%) had 1 extranodal site and 378 (30%) had ≥2 extranodal sites. Among 535 patients who received rituximab, 163 (30%), 217 (41%) and 155 (29%) had 0, 1 and ≥2 extranodal sites, respectively. Of the 37 coded extranodal sites, the most commonly involved sites included soft tissue (16.2%), bone (11.3%), bone marrow (9.1%), pleura (9.1%), head and neck soft tissue (8.2%), stomach (8.7%), intestine (8.2%), lung (7.8%) and liver (5.8%). In multivariate analysis that included other IPI variables, extranodal involvement as defined in the IPI (≥2 sites) was not a significant prognostic factor in our cohort (with or without rituximab, see Table 1). However, the presence of any extranodal disease was found to correlate with a poorer overall survival in patients treated with rituximab (p=0.03). When specific extranodal sites were examined in the rituximab group, bone marrow (p<0.001), liver (p=0.03) and pleura (p=0.05) involvement correlated with inferior overall survival in univariate analysis, but only bone marrow involvement (HR=1.9, p=0.02) remained significant in multivariate analysis.
Conclusions: In the post-rituximab era, extranodal involvement remains a significant prognostic factor, although not as traditionally defined in the IPI, but rather refined as the presence of any extranodal disease involvement. Furthermore, bone marrow involvement represents the only extranodal site associated with a poorer overall survival independent of the IPI.
Prognostic Significance of Extranodal Disease Involvement for Overall Survival
Author notes
Disclosure: No relevant conflicts of interest to declare.

