Abstract
Introduction: The identification of an 11q deletion (del) by FISH analysis is reportedly an independent predictor of poor survival in CLL (
Methods: We searched our database for untreated CLL patients who presented to MDACC from 10/03 to 4/07 with an 11q del and reviewed their medical records. Patient bone marrow samples were assessed at presentation by FISH analysis using probes for trisomy 12, ATM, LAMP1, D13S319, and P53 genes.
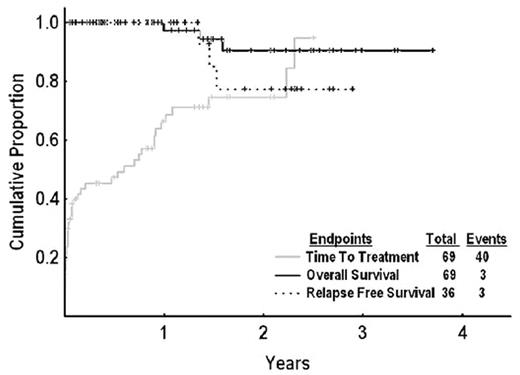
Results: Overall, 69 of 708 (9.7%) patients analyzed using FISH, had an 11q del without a 17p del. In addition to 11q del, 62% had 13q del, and 3% had trisomy 12. Their median age was 59 yrs; and 80% were males. Zubrod performance status was > 0 in 53%; and 13% had Rai stage 3–4. Lymphadenopathy was present in 96% (> 5 cm, 11%), splenomegaly in 19%, anemia in 9%, and thrombocytopenia in 4%. ZAP-70 was expressed in 74% (34/46), CD38 in 61% (33/54), and 89% (39/44) had an unmutated IgVH gene. The median absolute lymphocyte count (ALC) was 24 × 109L (range, 2–513 × 109L), and the median proportion of cells that exhibited an 11q del was 53% (range, 9–98%). Cytogenetics were as follows: del(11)(q13q23) in 17/63 (27%) patients, normal in 37 (59%), del6(q13q25) in 1, complex in 2, and other in 6 patients. The median time from presentation at MDACC to treatment was 1 month (range, 0–28) and from diagnosis to treatment was 15 months (range, 1–97). The median ALC doubling time was 237 days. Forty patients required therapy for progressive disease (lymphadenopathy 17, ALC doubling time <1 yr 14, B-symptoms 6, splenomegaly 2, and anemia 1); and 38 were evaluable for response: 29 treated with FCR (fludarabine, cyclophosphamide, and rituximab), 4 with CFAR (FCR+alemtuzumab), 3 with R-GMCSF (rituximab+GMCSF), and 2 with other therapies (FC 1, CVP+R 1). The overall response rates for FCR+CFAR, R-GMCSF, and other therapies were 100%, 33%, and 100%, respectively; and the CR rates were 88%, 0%, and 100%, respectively. Among 23 patients who were monitored by FISH analysis after treatment, 21 had disappearance of 11q del. One patient who developed Richter’s syndrome (RS) and another patient with relapsed CLL had recurrence of the 11q del clone (both ZAP-70 positive, IgVH gene unmutated). The median follow-up of surviving patients was 13 months. Only 3 patients have died, including the RS patient, who died from sepsis after therapy, and 2 patients who died from pancreatic cancer and glioblastoma. At 1 and 3 yrs, the survival rates were 97% and 91%, respectively. Three patients developed relapsed disease at 16, 17, and 18 months. Time to treatment, survival, and relapse-free survival (RFS) are shown in Fig.
Conclusions: CLL with an 11q del was associated with high rates of response, survival, and RFS when treated with FCR-containing therapy. This cohort of patients will be followed over the long term to establish the natural history of 11q del in the chemoimmunotherapy era.
Disclosure: No relevant conflicts of interest to declare.