Abstract
Background: Glutathione peroxidase-1 (GPX1) is the most significant catalytic antioxidant in the red cell. Congenital deficiency of GPX1 has been reported in association with hemolytic anemia due to oxidant stress. Hemolytic rate has been implicated in the development of sickle vasculopathy.
Methods: Red cell pellets were collected from 32 patients with sickle cell disease and 17 healthy African American control subjects, and were stored frozen until assayed. A novel microplate immunoaffinity capture assay was used that measures both immunoreactive GPX1 protein and enzyme activity.
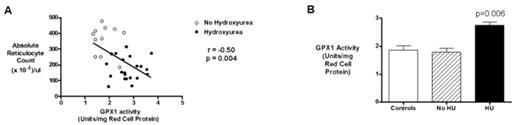
Results: Patients with SCD had higher levels of red cell GPX1 activity than controls (2.42 ± 0.12 vs. 1.86 ± 0.15 units/mg red cell protein (mean ± SEM), p=0.006). GPX1 activity correlated with low reticulocyte count (r=−0.50, p=0.004)(Fig. 1A), low indirect bilirubin (r=–0.45, p=0.01) and high fetal hemoglobin expression (r=0.39, p=0.03). GPX1 activity in SCD patients on hydroxyurea was much higher than those not on hydroxyurea (2.75 ± 0.12, n=21 vs. 1.79 ± 0.13, n=11, p<0.001)(Fig. 1B), suggesting that hydroxyurea might induce GPX1 expression. In the patients off hydroxyurea, low GPX1 activity closely correlated with high serum lactate dehydrogenase level, a marker of high hemolytic rate (r=–0.85, p=0.002), suggesting that low GPX1 levels might contribute to rapid hemolytic rate. In a multivariate model, GPX1 was independently associated with reticulocyte count even when adjusted for fetal hemoglobin level.
Conclusions: In addition to fetal hemoglobin, hydroxyurea may also induce expression of GPX1, a potent antioxidant that might have a role in decreasing hemolysis associated with the robust oxidant stress of SCD. This finding is consistent with previously published evidence of GPX1 induction by hydroxyurea in cancer cell lines, with increased antioxidant function. Additional studies are needed to confirm this phenomenon in a larger cohort of patients with SCD and to further evaluate the combined effect of fetal hemoglobin co-induction, but this finding suggests a potential mechanism by which hydroxyurea may produce clinical benefit in SCD even in the absence of significant fetal hemoglobin induction.
Author notes
Disclosure:Employment: Jong Seo Lee PI is employed by Ab Frontier Co., Ltd., the manufacturer of the microplate immunoaffinity capture assay that was used to generate the data in this study. Research Funding: Gregory Kato and Mark Gladwin are supported by intramural funding from the National Institutes of Health. Sue Goo Rhee is supported by Korean Government Grant FPR-0502. Membership Information: Sue Goo Rhee serves as a member of a paid advisory board to Ab Frontier Co., Ltd., which produces antibodies.