Abstract
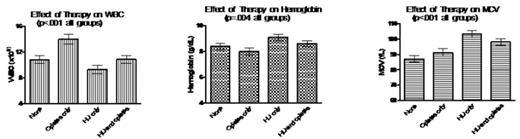
Sickle cell disease (SCD) patients experience high rates of morbidity and early mortality. Hydroxyurea (HU) therapy is associated with decreased morbidity and mortality as well as improved patient health outcomes (Charache et al, 1995 and Steinberg et al, 2003). However, the effect of chronic opiate pain management on HU treatment outcomes is unknown. In the current study, we evaluated the effects of HU and chronic long acting opiate therapy-OxyContin, methadone, fentanyl and MS Contin-on the following laboratory parameters: white blood cell count (WBC), hemoglobin (Hb), and mean corpuscular volume (MCV). Changes in these variables are known to be linked with HU effects on morbidity and mortality in SCD. 142 homozygous sickle cell anemia patients (75 females and 67 males) from the outpatient clinic at Duke University Medical Center were included in this study. Clinical data were collected by patient interview as well as review of medical records after informed consent. Patients were classified in 4 groups based on report of chronic daily use of long acting opiates and/or HU (current therapy with HU) as follows: No HU or opiates (None); opiates only; HU only; and HU and opiates. ANOVAs were used to identify combined effects of opiate therapy, HU therapy and the 3 laboratory parameters. Overall, we found that patients on HU (n=76, 54%), had lower WBC and higher Hb and MCV than the no HU patients (n=66, 46%), with p<.01 for all associations, as could be expected. In contrast to the positive effects of HU, patients on opiates had higher WBC than non opiate patients (p<.01). Surprisingly, when adjusting for gender and age, opiate therapy appeared to moderate the effect of HU treatment on WBC (p=.05) and MCV (p=.04). Patients who were on HU and opiates concurrently exhibited 17% higher WBC and 6% lower MCV than patients who were on HU alone, suggesting that opiate therapy may be attenuating the positive effects of HU. The findings from the current study confirm that HU treatment is associated with better patient health indices, i.e. lower WBC, higher Hb and MCV. In contrast, chronic opiate pain management, often a concomitant therapy with HU, was associated with poorer patient laboratory indices, both with or without concurrent HU treatment. Overall, these data indicate that the chronic use of opiates may decrease the efficacy of HU treatment in this patient population. Further studies are needed to study the mechanism of drug interaction between opiate and HU in SCD patients. The previously suggested inhibitory effect of HU on the cytochrome P450 CYP3A, an important cytochrome in the metabolism of some opiates (Reardon et al, 2005), should be considered for future studies of drug-drug interaction in SCD.
Author notes
Disclosure: No relevant conflicts of interest to declare.