Abstract
Low dose aspirin is widely used as a well-documented antiplatelet drug in patients with cardiovascular disease. However, several laboratories report a highly variable platelet response to aspirin treatment when assessed by different methods, referred to as ’aspirin resistance’. Aspirin resistance may in part be explained by different degrees of compliance, and also by different doses of aspirin used. In a prospective study we measured serum thromboxane B2 (se-TxB2) in order to investigate whether 75 mg daily of aspirin was sufficient to inhibit the enzyme COX-1. Furthermore, the endogenous production of thromboxane A2, urinary-11-dehydro-thromboxane B2 (U-TxM), was determined. Finally, we measured platelet function by optical platelet aggregometry (OPA) in platelet-rich plasma induced by arachidonic acid (AA) 1.0mM and by adenosine diphosphate (ADP) 5.0 μM. Twenty-two healthy individuals ≥18 years and 44 patients with stable coronary artery disease were included. All subjects had been treated with 75 mg of plain aspirin daily for at least 7 days to achieve steady state before blood sampling. At inclusion the participants received a pill box with the study medication and careful instruction regarding the medication. Compliance was optimized by interview and pill counting at each visit. Reading through all case report forms we found that every participant was 100% compliant stated by every-day interviewing and pill-counting. We found that low-dose aspirin inhibited se-TxB2 more than 99% and U-TxM by 74% on average.
| Group . | se-TxB2, baseline . | se-TxB2, aspirin . | U-TxM, baseline . | U-TxM, aspirin . |
|---|---|---|---|---|
| Healthy (n=22) | 326 [277;377] | 1.2[0.9;1.5] | 295 [248;343] | 77 [65;90] |
| Patients (n=44) | - | 1.0 [0.9;1.2] | - | 68 [61;76] |
| Group . | se-TxB2, baseline . | se-TxB2, aspirin . | U-TxM, baseline . | U-TxM, aspirin . |
|---|---|---|---|---|
| Healthy (n=22) | 326 [277;377] | 1.2[0.9;1.5] | 295 [248;343] | 77 [65;90] |
| Patients (n=44) | - | 1.0 [0.9;1.2] | - | 68 [61;76] |
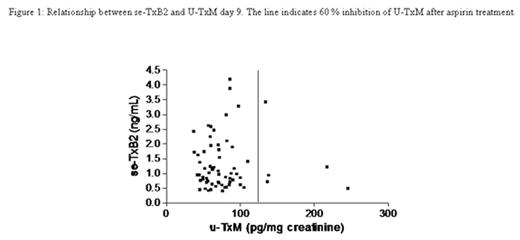
All of the participants had a complete inhibition of their COX-1 pathway evaluated by measurements of se-TxB2 (<4.5 ng/mL). However, 5 of the 66 (7.5%) individuals had less than 60% inhibition of the U-TxM.
Relationship between se-TxB2 and U-TxM day 9. The line indicates 60% of inhibition U-TxM after aspirin treatment.
Relationship between se-TxB2 and U-TxM day 9. The line indicates 60% of inhibition U-TxM after aspirin treatment.
The high U-TxM indicates that other pathways synthesizing TxA2 were not completely inhibited. After treatment with aspirin the OPA induced by AA and by ADP decreased significantly. By using limits of > 20% aggregation with AA 1.0 mM and > 70% aggregation for ADP 5 μM as suggested in the literature, we identified three participants (4.5%) who were aspirin resistant. Our finding, that 4.5% of the participants were identified as aspirin resistance by OPA, despite 100% compliance, is interesting and makes the concept ’aspirin resistance’ even more complicated. Even though the COX-1 pathway was completely inhibited, insufficient suppression of OPA and U-TXM, were observed. In conclusion, our findings support that low-dose aspirin of 75 mg daily, was sufficient to suppress se-TxB2 > 99% in patients with stable coronary artery disease. High level of se-TxB2 in patients on low dose aspirin as reported in other studies may be due to poor compliance.
Author notes
Disclosure: No relevant conflicts of interest to declare.