Abstract
Transfusion-associated graft versus host disease (TA-GVHD) is a rare, but almost always a fatal complication. It has a mortality rate above 90%. For the development of TA-GVHD is need
immunocompetent cells in the blood product,
incompatibility in HLA alloantigen,
immune failure of the recipient against the donor cells.
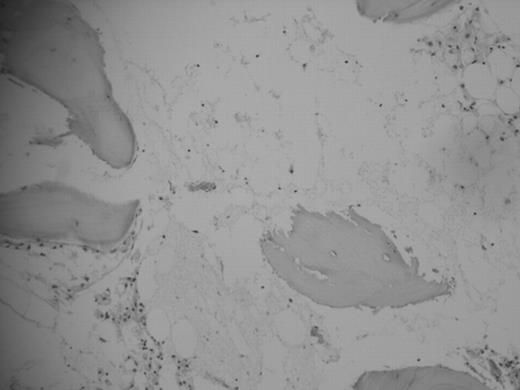
The exact incidence is unknown, but more than 200 cases have been reported in the world literature and the molecular test for diagnostic where performed only in a very few of them. Thirty-five years old woman with multiple fractures in right leg from a car accident was treated in her rural town, she received a fresh whole blood transfusion from her sister and then went for surgery, antibiotics and analgesia where given; six days after she developed erytroderma in the upper chest, two days later generalized bone pain and weakness were aggregated, the next day erithroderma generalize and started with diarrhea and jaundice; her evolution was torpid with fever, more weakness and jaundice, pallor, purpura and oropharyngeal pain. She was sent for hematological evaluation to our tertiary care institution, and a TA-GVHD was considerate; a work up on that was performed and the CBC showed pancytopenia, LFT with elevation of bilirubins, transaminases and alkaline phosphatase; the bone marrow aspiration and biopsy with aplasia, the skin biopsy with lymphoid infiltration, junction of epidermis with dermis was intact and no leukocytoclastic vasculitis. She received methylprednisolone, cyclosporine, filgrastim, wide range antibiotics and amphotericin B, leukoreduced and irradiated blood products. Her evolution was torpid with deterioration of her conditions and 48 hour later she died of septic shock. There is no effective treatment for TA-GVHD and no difference between early o delayed diagnostic, the evolution is almost always fatal, that is why the prevention is needed with the leukoreduction and irradiation of blood products, specially in recipients with clear risk for development of TA-GVHD: congenital immunodeficiencies, fetuses y newborns, hematological cancers, solid tumors in chemotherapy, hemopoiectic and solid organ transplanted, and first and second degree relatives. Better policies, technology, education for the primary care physician and access to blood products with high quality is needed to prevent this type of complications, specially in rural areas where transfusions with whole fresh blood from relatives are performed commonly.
Author notes
Disclosure: No relevant conflicts of interest to declare.