Abstract
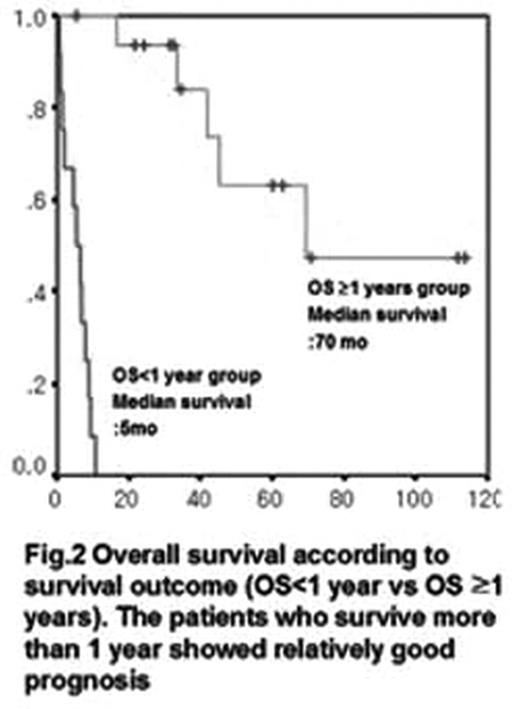
BACKGROUND Extranodal NK/T-cell lymphoma is notable for its unique behavior; Many patients die before 1 year from the diagnosis. However, the patients who survive the first year from the diagnosis live for longer period. Known prognostic factors were insufficient to explain this unique pattern. The objective of this study was to investigate clinicopathological features according to survival outcome(OS<1 yr vs OS ≥1 yrs).
METHODS We reviewed 28 patients who diagnosed as extranodal NK/T cell lymphoma from March, 1995 to July, 2006. Patients were treated with chemotherapy alone or chemoradiotherapy. Real-time PCR was done from the tissue of the biopsy specimen to quantify the Epstein-Barr virus load.
RESULTS Of the 28 patients, 14 patients(50%) achieved a complete remission(CR). Median survival was 46 months(range, 1–114 months). The B symptoms, IPI score, stage, ECOG status, first treatment response was significant prognostic factor (P<0.05). However ECOG status the only significant prognostic factor by using mutivariate analysis (P=0.001). Seventeen patients (61%) expired; 12 of those patients died during the first year of diagnosis. Thus we divided them into 2 groups; who lived more than 1 year and who lived less than 1 year. The ECOG status, first treatment response rate was different between the two groups significantly(p<0.05). All patients showed positive EBV by PCR. However, there was no significant difference in EBV load between these two groups. (p=0.113)
CONCLUSION The ECOG status, and response to the first treatment related to the survival of first year from the diagnosis. For the patients with poor performance status, and failure to achieve CR after the first treatment, more aggressive treatment should be considered to improve survival. In our study, EBV load measured on the paraffin tissue failed to correlate with survival.
Univariate Analysis of Overall survival
| Prognostic Factors . | Median OS(months) . | P value . |
|---|---|---|
| Age | ||
| >60yrs | 33 | |
| <60yrs | 10 | 0.783 |
| Type | ||
| Nasal | 33 | |
| Nasal type | 5 | 0.225 |
| B symptom | ||
| Yes | 5 | |
| No | 42 | 0.021 |
| IPI | ||
| Low/Low-intermediate | 42 | |
| High-intermediate/High | 2 | 0.002 |
| Stage | ||
| I/II | 42 | |
| III/IV | 2 | 0.001 |
| ECOG | ||
| 0,1 | 45 | |
| 2,3,4 | 2 | 0.001 |
| LDH | ||
| Normal | 33 | |
| High | 17 | 0.720 |
| EBV | ||
| load(copies/ug DNA)(n=22) | 46 | 0.228 |
| Treatment | ||
| C/T alone | 5 | |
| C/T and R/T | 42 | 0.196 |
| treatment response | ||
| CR | 45 | |
| No-CR | 14 | 0.0127 |
| Prognostic Factors . | Median OS(months) . | P value . |
|---|---|---|
| Age | ||
| >60yrs | 33 | |
| <60yrs | 10 | 0.783 |
| Type | ||
| Nasal | 33 | |
| Nasal type | 5 | 0.225 |
| B symptom | ||
| Yes | 5 | |
| No | 42 | 0.021 |
| IPI | ||
| Low/Low-intermediate | 42 | |
| High-intermediate/High | 2 | 0.002 |
| Stage | ||
| I/II | 42 | |
| III/IV | 2 | 0.001 |
| ECOG | ||
| 0,1 | 45 | |
| 2,3,4 | 2 | 0.001 |
| LDH | ||
| Normal | 33 | |
| High | 17 | 0.720 |
| EBV | ||
| load(copies/ug DNA)(n=22) | 46 | 0.228 |
| Treatment | ||
| C/T alone | 5 | |
| C/T and R/T | 42 | 0.196 |
| treatment response | ||
| CR | 45 | |
| No-CR | 14 | 0.0127 |
Multivariate Analysis of Overall survival
| Prognostic Factors . | Hazad Ratio . | 95% CI . | P . |
|---|---|---|---|
| B symptom | |||
| No | 1.00 | ||
| Yes | 0.97 | 0.11–8.58 | 0.980 |
| IPI score | |||
| Low/Low-inermediate | 1.00 | ||
| High-intermediate/High | 1.35 | 0.25–7.26 | 0.730 |
| Stage | |||
| I,II | 1.00 | ||
| III,IV | 0.60 | 0.06–6.12 | 0.668 |
| ECOG | |||
| 0,1 | 1.00 | ||
| 2,3,4 | 6.94 | 2.23–21.55 | 0.001 |
| Treatment response | |||
| CR | 1.00 | ||
| No-CR | 1.98 | 0.56–6.96 | 0.287 |
| Prognostic Factors . | Hazad Ratio . | 95% CI . | P . |
|---|---|---|---|
| B symptom | |||
| No | 1.00 | ||
| Yes | 0.97 | 0.11–8.58 | 0.980 |
| IPI score | |||
| Low/Low-inermediate | 1.00 | ||
| High-intermediate/High | 1.35 | 0.25–7.26 | 0.730 |
| Stage | |||
| I,II | 1.00 | ||
| III,IV | 0.60 | 0.06–6.12 | 0.668 |
| ECOG | |||
| 0,1 | 1.00 | ||
| 2,3,4 | 6.94 | 2.23–21.55 | 0.001 |
| Treatment response | |||
| CR | 1.00 | ||
| No-CR | 1.98 | 0.56–6.96 | 0.287 |
Overall survival according to survival outcome (OS<1 year vs OS ≥ 1 years). The patients who survive more than 1 year showed relativily good prognosis.
Overall survival according to survival outcome (OS<1 year vs OS ≥ 1 years). The patients who survive more than 1 year showed relativily good prognosis.
Author notes
Disclosure: No relevant conflicts of interest to declare.