Abstract
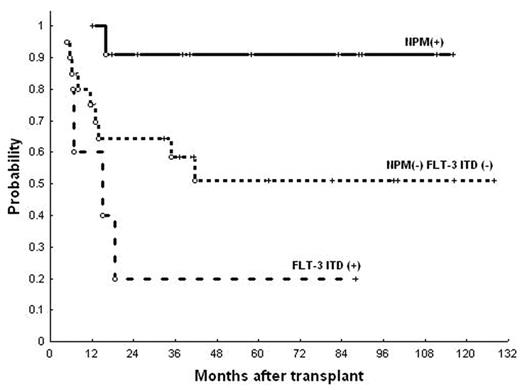
Post-remission therapy in patients with acute myeloid leukemia (AML) is assigned according to the predictable biological risk of the disease, mainly based on cytogenetics. Nonetheless, optimal post-remission strategy for the intermediate-risk subtype, given the prognostic heterogeneity of this category, is currently undefined. Analysis of potentially relevant molecular features within this subgroup might contribute to clarify the role of autologous stem cell transplantation (autoHSCT) in these patients. Thirty seven patients (age: 53, 15–66; 51% female) diagnosed with intermediate-risk de novo AML during the period 1994–2006 who received an autoHSCT in first complete response were included in the study. Pre-transplant therapy was similar in all patients, consisting of standard induction chemotherapy (ICE, n=8, IDICE, n=29) and one cycle of high-dose ara-C-based consolidation chemotherapy. Internal tandem duplication of flt-3 (flt-3 ITD) and exon 12 NPM1 mutations were studied by either PCR or RT-PCR following standard methods. Gene expression profiling was examined in 28 patients with oligonucleotide HGU133 Plus 2.0 arrays (Affymetrix). Gene expression measures were normalized using RMA methodology (Affy package), and dChip v1.3 and Limma software (Bioconductor) were used for unsupervised and supervised analyses. In order to identify genes with prognostic value, a supervised analysis based on patients’ outcome (relapsed patients vs. long-term responders, i.e. >2-year duration) was performed. The combined results of NPM mutation and flt-3 ITD defined three subgroups of patients with different outcome: group 1 (n=12), constituted by patients with mutated NPM1 without flt-3 ITD; group 2 (n=20), which included patients with neither NPM1 mutation or flt-3 ITD; and group 3 (n=5), defined by flt-3 ITD regardless NPM1 mutational status. Thus, 5-year survival of these 3 subgroups of patients was 91%±9%, 52%±12%, and 20%±18%, respectively (p=0.02; see figure). Preliminary results of multiple gene profile comparisons between subgroups of patients with different outcome disclosed a cluster of genes with differential expression. Thus, in the most significant balanced comparison, 1238 genes were found to vary significantly in the unsupervised analysis, and 109 differentially expressed genes were identified in the supervised analysis. Interestingly, overexpression of genes such as TNF, RETN, CFLAR, SLC16A7, ENG, CD48, PLCR1, and SULTB1 correlated with a high relapse risk, whereas increased expression of YY1, FBXL12 and EXOSC6 were associated with a favorable outcome. In conclusion, presence of NPM1 mutation and flt-3 ITD are strong predictors of the outcome after autoHSCT in patients with intermediate-risk AML. Furthermore, genome-wide analysis may contribute to further define gene clusters with prognostic significance in patients with cytogenetically intermediate-risk AML receiving autoHSCT as consolidation therapy.
Author notes
Disclosure:Research Funding: Grant no. 04/1085 from the Spanish Fondo de Investigaciones Sanitarias.