Abstract
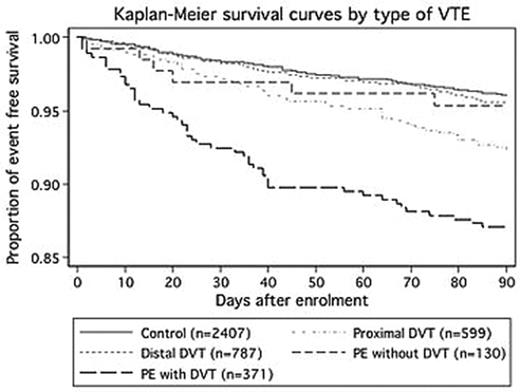
Venous thromboembolism (VTE), including deep vein thrombosis (DVT) and pulmonary embolism (PE), is associated with a significant mortality and life-long morbidity. A large number of studies have focused on VTE, contributing to better improving its management. Especially studies have provided accurate estimates of 3-month mortality rates for PE and have identified prognostic factors that may guide the physician’s initial treatment decision for these patients. However, improvements in the prevention of venous thromboembolism (VTE) and diagnosis have changed the epidemiology of VTE over the last twenty years. Advances in imaging technology have resulted in more frequent diagnosis and treatment of early presentation of VTE, including isolated distal DVT or isolated PE. However, the clinical signification and the prognosis of these forms of VTE are unknown. Therefore we prospectively investigated the 3-month overall for isolated distal DVT, proximal DVT, PE with DVT and PE without DVT, among a large in and out population study. Between November 2004 and January 2006, all patients over 18 years old who were referred to 359 french board-certified vascular physicians for a clinical suspicion of VTE were included. VTE presentations were categorized using validated clinical decision rules and objective tests including ultrasonography, lung scan and helical CT scan. Subjects without an objectively confirmed diagnosis of VTE were used as controls. All patients with confirmed VTE and a random sample of controls were followed-up at 3 months. We estimated 3 months survival for each type of VTE 8256 patients entered the study, among which 7532 were analysed. The median age for all patients was 65 years (49–77 years), 2923 (39%) were men, 2925 were inpatients (39%), and 1884 (25%) had a previous history of VTE. 933 had isolated distal DVT (12%), 710 proximal DVT (9.4%), 426 PE with DVT (5.7%), 148 PE without DVT (2.0%) and 5315 had no VTE (70.6%). Overall, 4290 patients were followed up at 3 months. At 3 months, VTE recurrence was not significantly different between the 5 groups of patients. By contrast, 95/2407 control patients (4%), 35/787 (4.4%) distal DVT, 48/598 (8%) proximal DVT, 48/371 (12.9%) PE with DVT, and 6/130 (4.6%) died. In multivariate analysis, the 3-months mortality adjusted hazard ratio [95% CI] was 1.1 [0.7–1.7] for distal DVT (P 0.59), 1.6 [1.1–2.3] for proximal DVT (P 0.013), 2.1 [1.4–3.0] for DVT-associated PE (p<0.01), and 0.5 [0.2–1.1] for isolated PE (P 0.084). Kaplan-Meier survival estimates were 96% [95% CI 95–97] for controls as compared with 95% [94–97], 92% [90–94], 87% [83–90] and 95% [90–98] for isolated distal DVT, proximal DVT, PE with DVT, and PE without DVT cases, respectively (Figure 1). Therefore, compared to controls, only patients with proximal DVT or PE with DVT were at increased risk of death, while patients with isolated PE without DVT were not.
Author notes
Disclosure: No relevant conflicts of interest to declare.