Abstract
Background: A previous CALGB trial (
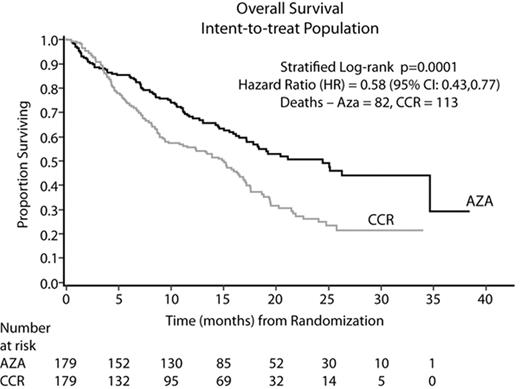
Results: In all, 358 pts (70% male), were randomized at 79 sites to AZA (N=179) or CCR (N=179): BSC only (N=105, 59%), LDAC (N=49, 27%), or Std CT (N=25, 14%). Median age was 69 yrs (38–88) and per treatment (TX): AZA (69 yrs); BSC only (70 yrs); LDAC (71 yrs); and Std CT (65 yrs). The AZA and CCR groups were comparable for baseline (BL) parameters. At BL, 95% of pts were higher risk: RAEB (58%), RAEB-T/WHO AML (34%), CMML (3%), and other (5%). By IPSS, 87% were higher risk: Int-2 (40%), High (47%), and 13% indeterminate/other. AZA was administered for a median of 9 cycles; LDAC for 4 cycles. Median followup for the OS analysis was 21.1 months (mo). AZA demonstrated statistically superior OS vs CCR (stratified log-rank p=0.0001). AZA showed a median Kaplan-Meier (KM) OS time of 24.4 mo vs 15 mo with CCR (Figure). The hazard ratio (HR, Cox Model) was 0.58 (95% CI: 0.43, 0.77) for a 74% OS improvement. At 2 yrs, there was a 2-fold OS advantage: AZA (51%) vs CCR (26%), 95% CI: 13, 36%, p<0.0001. Differences in OS KM medians (HR; log-rank p) between AZA and BSC, LDAC, and Std CT, respectively, were 12.9 mo (0.55; p=0.0003), 9.1 mo (0.60; p=0.016), and 8.7 mo (0.69; p=0.19). Median OS per IPSS cytogenetic subgroup showed similar results (Table). The 1, 2, and 3-mo survival rates did not differ between AZA and BSC only (p>0.20). AZA was well tolerated with safety data consistent with previous reports.
Conclusion: These data confirm and extend previous CALGB findings. This AZA trial is the first MDS clinical study to demonstrate a significant OS advantage, thus altering the natural disease course. AZA should now be considered first-line therapy for higher-risk MDS pts.
OS Analyses per IPSS Cytogenetic Group
| Group . | % (n/N) Pts . | AZA Median (Months) . | CCR Median (Months) . | HR (95%CI) . | Log-rank p . |
|---|---|---|---|---|---|
| Good | 46 (166/358) | Not reached | 17.1 | 0.61 (0.39, 0.96) | 0.030 |
| Intermediate | 21 (76/358) | 26.3 | 17.0 | 0.43 (0.21, 0.88) | 0.017 |
| Poor | 28 (100/358) | 17.2 | 6.0 | 0.52 (0.32, 0.87) | 0.011 |
| Group . | % (n/N) Pts . | AZA Median (Months) . | CCR Median (Months) . | HR (95%CI) . | Log-rank p . |
|---|---|---|---|---|---|
| Good | 46 (166/358) | Not reached | 17.1 | 0.61 (0.39, 0.96) | 0.030 |
| Intermediate | 21 (76/358) | 26.3 | 17.0 | 0.43 (0.21, 0.88) | 0.017 |
| Poor | 28 (100/358) | 17.2 | 6.0 | 0.52 (0.32, 0.87) | 0.011 |
Figure
Author notes
Disclosure:Employment: Dr Jay Backstrom, CL Beach, Linda Zimmerman, and David McKenzie are employees of Pharmion Corporation. Consultancy: Drs Bennett, Byrd, List, Giagounidis, Gore, and Mufti. Ownership Interests:; Dr Byrd, Dr Giagounidis, Dr Backstrom, CL Beach, Linda Zimmerman, and David McKenzie. Research Funding: Drs. Fenaux, Seymour, Silverman, List, and Hellstrom-Lindberg. Honoraria Information: Drs. Fenaux, Seymour, Gore, Mufti, List, Santini, Silverman, and Hellstrom-Lindberg. Membership Information: Drs Seymour, Hellstrom-Lindberg, and Gore. Off Label Use: The abstract discusses results of a long term randomized, multicenter, controlled survival trial of azacitidine in the label-approved population of MDS patients. However, the current labeling for azacitidine does not include an effect on survival.