To the editor:
Five to 10% of patients with chronic myelogenous leukemia (CML) do not have the Philadelphia (Ph) translocation. A smaller number also lack any detectable BCR/ABL rearrangement by interphase fluorescent in situ hybridization (FISH) or real-time polymerase chain reaction (RT-PCR). Although clinically and hematologically similar, BCR/ABL negative (BCR/ABL−) CML has been associated with a worse prognosis.1,2 Transplantation remains an option, although successful outcomes have only been reported in a handful of patients.3
Ph+ CML is uniquely susceptible to graft-versus-leukemia (GVL) effects and molecular studies have shown that BCR/ABL functions as a tumor antigen.4,–6 In contrast, the efficacy of GVL in BCR/ABL− patients remains poorly defined. For these patients, the prospect of transplantation presents many uncertainties; in the absence of BCR/ABL expression will their disease be as susceptible to GVL?
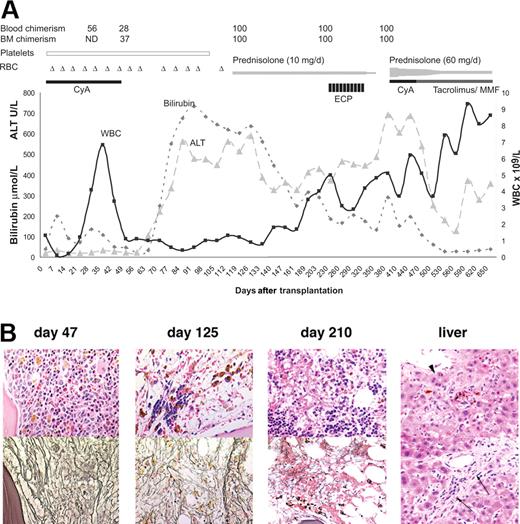
A 45-year-old woman presented with massive splenomegaly, a white cell count of 8.6 × 109/L, platelet count of 53 × 109/L, and hemoglobin of 110 g/L. The karyotype was 46XX, interphase FISH and RT-PCR for BCR/ABL were negative. BCR/ABL− CML was diagnosed and she was prepared for transplantation from her HLA-identical brother with high-dose busulfan (64 mg/kg) and cyclophosphamide (120 mg/kg). Routine whole blood chimerism testing at day 30 revealed partial donor chimerism of only 56% (Figure 1A) and cyclosporine (CyA) was rapidly tailed to boost donor engraftment. At day 47, upon cessation of immunosuppression, the bone marrow showed marked infiltration with leukemia (Figure 1B) and donor chimerism had further declined to 28% in the peripheral blood and 37% in the bone marrow aspirate.
Clinical and histologic analysis of recovery after transplantation. (A) Recovery after transplantation. Blood chimerism and bone marrow (BM) chimerism are percentages; (▵) indicates days on which the patient received red blood cells (RBC). The open, black, and grey bars indicate administration of platelets, CyA, ECP, prednisolone, tacrolimus, and MMF. (B) Hematoxylin and eosin (top) and silver stain for reticulin (bottom) on bone marrow biopsies 47, 125, and 210 days after transplantation; liver biopsy on day 210 showing biliary metaplasia ( ) and portal tract fibrosis (←). Images were acquired using a Nikon microscope (Nikon, Melville, NY) equipped with a 40×/.75 NA objective, a Spot color camera, and imaging software version 4.0.1 (Diagnostic Instruments, Sterling Heights, MI).
) and portal tract fibrosis (←). Images were acquired using a Nikon microscope (Nikon, Melville, NY) equipped with a 40×/.75 NA objective, a Spot color camera, and imaging software version 4.0.1 (Diagnostic Instruments, Sterling Heights, MI).
Clinical and histologic analysis of recovery after transplantation. (A) Recovery after transplantation. Blood chimerism and bone marrow (BM) chimerism are percentages; (▵) indicates days on which the patient received red blood cells (RBC). The open, black, and grey bars indicate administration of platelets, CyA, ECP, prednisolone, tacrolimus, and MMF. (B) Hematoxylin and eosin (top) and silver stain for reticulin (bottom) on bone marrow biopsies 47, 125, and 210 days after transplantation; liver biopsy on day 210 showing biliary metaplasia ( ) and portal tract fibrosis (←). Images were acquired using a Nikon microscope (Nikon, Melville, NY) equipped with a 40×/.75 NA objective, a Spot color camera, and imaging software version 4.0.1 (Diagnostic Instruments, Sterling Heights, MI).
) and portal tract fibrosis (←). Images were acquired using a Nikon microscope (Nikon, Melville, NY) equipped with a 40×/.75 NA objective, a Spot color camera, and imaging software version 4.0.1 (Diagnostic Instruments, Sterling Heights, MI).
Fearing the worst, we counseled the patient that she might not survive and offered continuing supportive care. Over the next 30 days, she became increasingly unwell with anorexia, abdominal pain, nausea, jaundice, and hepatosplenomegaly. An ultrasound scan showed diffuse enlargement of the liver and spleen in keeping with progressive CML. She remained profoundly transfusion dependent. Rapidly rising bilirubin and alanine aminotransferase (ALT) levels reached peaks of 733 mM (42.8 mg/dL) and 479 U/L, respectively, at about 90 days. No rash or diarrhea was ever noted.
Unexpectedly, her condition slowly stabilized and she was fit enough for chimerism assessment and bone marrow biopsy at day 125. To our surprise, this revealed 100% donor engraftment in blood and marrow with dramatic and complete clearance of leukemia and some returning erythroid activity (Figure 1B). By 210 days, bone marrow cellularity and reticulin staining were approaching normal (Figure 1B). Liver biopsy confirmed chronic hepatic graft-versus-host disease (GVHD; Figure 1B), and conservative treatment with prednisolone was commenced. An early attempt to withdraw corticosteroids following extracorporeal phototherapy (ECP) was unsuccessful. With stable donor chimerism of 100% at 1 year after transplant, triple immunosuppression was initiated with prednisolone, cyclosporine/tacrolimus, and mycophe-nolate mofetil (MMF). Liver function tests subsequently improved and the patient remains alive and well more than 3 years after transplantation.
This case demonstrates a potent GVL effect in BCR/ABL− CML, suggesting that the cellular phenotype rather than the expression of BCR/ABL itself is paramount. A refractory leukemia was cleared from the bone marrow in parallel with aplasia and clinical GVHD, classic features of GVL reactions after donor lymphocyte infusion for relapsed Ph+ CML. While this observation is primarily relevant to the minority of patients who present with BCR/ABL− CML, BCR/ABL− clones are also found in imatinib-resistant Ph+ CML patients7,8 who may become future candidates for transplantation.
Authorship
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Matthew Collin, Haematological Sciences, Newcastle University, Framlington Place, Newcastle upon Tyne NE2 4HH, United Kingdom; e-mail:matthew.collin@ncl.ac.uk.