Mateo and colleagues demonstrate the ability of angiotensin-II to induce selective recruitment of mononuclear leukocytes to the arterial vasculature in both animals and simple but relevant human systems, a process that might underlie the earliest events of atherosclerosis.
Atherosclerosis is a disease of large arteries in which macrophage recruitment to the vascular wall plays an integral role. The prevailing view is that for these cells to be recruited to sites of lesion development, they must adhere to the endothelial lining of large arteries, an environment of high shear forces and low adhesion molecule expression. Mediators like TNF or Toll-like receptor (TLR) ligands, which induce neutrophil adhesion to venular endothelium, induce very subtle or no adhesion on the arterial side of the circulation.1-3 This raises the question of whether alternative mediators exist with a unique ability to induce recruitment in arteries.
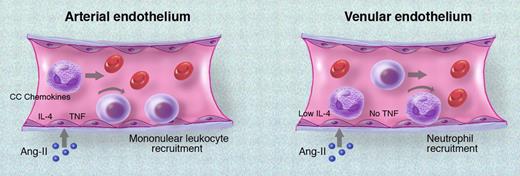
Important previous work from Alvarez et al has demonstrated that angiotensin-II (Ang-II), a molecule implicated in numerous cardiovascular diseases, induces significant leukocyte adhesion in both venules and arterioles.4 However, the arterial response to Ang-II was strikingly different from the venous response, in that mononuclear cells adhered to arterial endothelium whereas neutrophils adhered to venular endothelium. Now, Mateo and colleagues provide further detail on the mechanism underlying the differential effect of Ang-II on arterial endothelial cells. Their data show that Ang-II–mediated mononuclear leukocyte recruitment in arterioles occurs in part via release of TNF, which drives CC chemokine expression, as well as via IL-4. In sharp contrast, neither of these cytokines contributes to Ang-II–induced neutrophil recruitment in adjacent postcapillary venules (summarized in the figure). These results are explained by observations that arterioles, but not venules, (1) constitutively express IL-4 and (2) express TNF in response to Ang-II, and that TNF in combination with IL-4 is necessary for the arterial response. The latter point is not trivial, as TNF or IL-4 alone are poor inducers of arterial adhesion.1,5 Human aortic endothelial cells as well as monocytes are also shown to respond to Ang-II by expressing TNF mRNA and releasing chemokines such as MCP-1 in a TNF-dependent fashion.
Comparison of angiotensin-II (Ang-II)–mediated leukocyte recruitment in arterioles and venules. In arterioles, high constitutive expression of IL-4 and Ang-II–induced TNF induces expression of CC chemokines such as MCP-1 and RANTES over a time course of several hours. These chemokines mediate selective arrest of mononuclear leukocytes in arterioles. In contrast, in postcapillary venules, Ang-II induces rolling and arrest within 60 minutes, predominantly recruiting neutrophils to the endothelial surface. This process does not require either IL-4 or TNF.
Comparison of angiotensin-II (Ang-II)–mediated leukocyte recruitment in arterioles and venules. In arterioles, high constitutive expression of IL-4 and Ang-II–induced TNF induces expression of CC chemokines such as MCP-1 and RANTES over a time course of several hours. These chemokines mediate selective arrest of mononuclear leukocytes in arterioles. In contrast, in postcapillary venules, Ang-II induces rolling and arrest within 60 minutes, predominantly recruiting neutrophils to the endothelial surface. This process does not require either IL-4 or TNF.
Importantly, these findings demonstrate that Ang-II has the ability to induce unique responses from arterial endothelial cells, which favor selective recruitment of mononuclear leukocytes. These responses were observed in arterioles; however, there is potential for differential responses between macrovascular and microvascular endothelium, as well as between endothelium from different organs. Since atherosclerosis is a disease of large arteries, it begs the question of whether Ang-II can also mediate these effects on endothelial cells in large arteries. Studies using in vivo or ex vivo imaging of atheroma-affected arteries could be used to address this issue.3,6 Often forgotten is that large arteries have their own microvasculature (the vasa vasorum), and it remains unclear how much of the mononuclear cell recruitment occurs via this microvasculature.7 As a final note, infection and the related activation of TLRs have recently received attention as inciting agents in atherosclerosis.8 It will be interesting to determine what relationship, if any, exists between Ang-II and TLRs.
Conflict-of-interest disclosure: The authors declare no competing financial interests. ■