Myelodysplastic syndrome (MDS) is a well-recognized complication of chemotherapy for multiple myeloma (MM). Serial bone marrow metaphase examinations were performed for MM restaging in 3077 patients undergoing high-dose therapy (HDT). MDS-associated cytogenetic abnormalities (MDS-CAs) were observed in 105 of 2418 patients in whom cytogenetic data were available after HDT. MDS-CAs occurred transiently in 72 patients and on 3 successive occasions (persistent MDS-CAs) in 33 patients, for 10-year estimates of 4% and 2%, respectively; only 21 patients developed overt clinical MDS and 5, acute myeloblastic leukemia (AML). MDS-CA development was linked to lower CD34 yield at collection, longer time interval from MM diagnosis to HDT, older age, and lower platelet recovery after HDT; persistent MDS-CAs were predicted by CD34 yield of less than 3 × 106/kg and need for more than 2 apheresis procedures. Applying a tertile frequency distribution over time to all 105 patients with MDS-CAs, its detection early after HDT was associated with longer time interval from diagnosis and low pre-HDT platelet count (likely resulting from pre-HDT damage), whereas late-onset MDS-CAs were noted among patients treated with Total Therapy 2 and Total Therapy 3 that applied post-HDT consolidation chemotherapy (suggesting possible post-HDT damage). While the risk of MDS-CAs was low and clinical MDS occurred infrequently, monitoring after post-HDT consolidation chemotherapy appears warranted.
Introduction
Autologous hematopoietic cell–supported high-dose therapy (HDT) with melphalan has become the standard of care in the management of younger patients with symptomatic or progressive multiple myeloma (MM).1,2 According to both randomized and historically controlled trials, tandem autotransplantation, especially, has increased complete response (CR) rates beyond 40% and at least doubled survival in relationship to standard-dose therapies.3,4 In fact, 10-year survival rates of more than 30% have been observed.5 The treatment-related mortality in most HDT trials is well less than 5% in patients up to and even older than 65 years.6 Long-term sequelae are uncommon, so that even third and fourth transplants have been successfully applied.7,8
Myelodysplastic syndrome (MDS) is a well-recognized complication of cancer therapy, especially with hematopoietic stem cell–toxic therapies such as ionizing radiation and alkylating agent–based chemotherapy (melphalan, nitrosoureas), occurring a median of 4 to 5 years after treatment.9,–11 Whereas cytogenetic abnormalities typifying MDS (MDS-CAs) after alkylator-based therapy include partial or complete deletions of chromosomes 5, 7, and 20 as well as trisomy 8,12,13 topoisomerase inhibitors, etoposide and doxorubicin, target chromosome 11 and induce MDS with a shorter latency phase of 1 to 2 years.14,–16 Sizable series have been reported on the development of therapy-related MDS (t-MDS) in the context of HDT for Hodgkin and non-Hodgkin lymphoma as well as for MM.17,,,–21 Since standard-dose regimens precede autologous bone marrow and, more recently, peripheral blood stem cell (PBSC) collection, it remains unclear whether t-MDS was initiated by chemotherapies administered prior to PBSC collection or by HDT or both. Most studies attributed MDS development to pretransplantation regimens; however, primary HDT after non–stem cell–toxic vincristine-adriamycin-dexamethasone (VAD) therapy for MM was associated with a low incidence of t-MDS of only 0% at 4.7 years.20 According to multivariate analyses, MDS-CA frequency reached 15% at 10 years after HDT in older patients (> 65 years), those with more than 24 months of standard chemotherapy prior to PBSC collection and poor PBSC collection.21,22 In recent studies that applied fluorescence in situ hybridization (FISH) analysis for the detection of MDS lesions in interphase cells, such abnormalities sometimes were already present in PBSCs prior to high-dose regimens and were similar or identical to those subsequently detected after HDT.23,24
At the University of Arkansas for Medical Sciences, cytogenetic analyses of Giemsa-banded metaphases were routinely performed as part of initial and subsequent bone marrow evaluations in patients with MM, primarily to detect MM-typical cytogenetic abnormalities (MM-CAs) conferring a poor prognosis.25,26 We now report our experience with such serial cytogenetic analyses for the detection of MDS-CAs during the follow-up of more than 3000 consecutive patients enrolled in melphalan-based HDT trials.
Methods
The institutional review board of the University of Arkansas for Medical Sciences approved the studies. Informed consent was obtained in accordance with the Declaration of Helsinki.
The database
The Arkansas MM database was reviewed for all 3077 patients who received at least one HDT regimen prior to January 2007. Bone marrow aspirates were routinely submitted for cytogenetic analysis prior to and serially after HDT, usually at 3-month to 6-month intervals during the first 3 years of follow up and then semiannually. Of all 3077 patients, at least one informative karyotype was available both prior to and after HDT in 2816. A diagnosis of MDS-CA was based on the presence of MDS-associated cytogenetic abnormalities in at least 2 metaphases in case of structural aberrations or trisomies, whereas 3 metaphases were required in case of hypodiploid abnormalities.27 Additional information gathered from the MM database included age, duration and type of pretransplantation therapy, hemoglobin concentration, platelet count, CD34 yield/kg body weight, days of PBSC collection, data on days to platelet and granulocyte recovery after first and second transplantation, as well as MM-related parameters such as immunoglobulin isotype, beta-2-microglobulin (B2M), C-reactive protein (CRP), and MM-CAs. Also annotated was whether patients received their primary therapy at Arkansas as part of Total Therapies 1 (TT1),28 2 (TT2),29 or 3 (TT3)30,–32 ) or other protocols (non–TT-P) or off-protocol (non-P), along with the transplantation preparatory regimen, such as melphalan 200 mg/m2 (MEL 200), melphalan 140 mg/m2 (MEL 140), MEL 140 plus total body irradiation (TBI), or combination chemotherapy with carmustine, etoposide, cytarabine, and melphalan (BEAM).33
Statistical methods
The method of Kaplan-Meier was used to estimate overall survival and cumulative incidence of MDS-CAs,34 using the log-rank test statistic for comparisons.35 Starting time for cumulative incidence of MDS-CAs was the date of the first HDT for each patient, with death included as a competing risk.36 P values for nonparametric tests of association in the 2 groups of patients (those with and without MDS-CAs) with continuous baseline variables, first and second transplantation, were obtained according to the method of Kruskal-Wallis (chi-square).37 The Cochran-Armitage trend test was used to compare patient characteristics according to their tertile frequency distribution over time.38 Univariate and multivariate Cox proportional hazard models were used to model time to t-MDS as a function of the baseline prognostic variables.39 Overall survival models were also created using the Cox proportional hazards methodology with stepwise model selection based on likelihood ratio and score tests.
Results
Onset of and variables associated with MDS-CAs
One-hundred five patients developed MDS-CAs, the details of which are summarized in Table 1. Only 21 of these patients were eventually diagnosed with MDS and 5 with acute myeloblastic leukemia (AML). While the majority of patients (78%) developed a single MDS abnormality, 17% had 2; 3%, 3; and 2%, even 4 concurrent MDS-CAs. Overall, del20q was the dominant abnormality; − 7/7q−, t(1;7)(p;q), and − 5/5q− abnormalities were each present in at least 10%. Figure 1 portrays the cumulative proportions of patients developing MDS-CAs. Since MDS-CAs could occur intermittently with intervening normal karyotypes, data are also presented separately for patients with transient versus persistent MDS-CAs (defined as 3 successive MDS-CA hits). At 10 years, the cumulative frequencies of transient MDS-CAs were 4% and of persistent MDS-CAs, 2%.
Cumulative incidence of MDS-CAs. Denoted are the times from first transplantation to any MDS-CA (blue), to the detection of transient MDS-CAs (red), and to the observation of the first among 3 successive MDS-CA examinations (persistent MDS-CAs [green]).
Cumulative incidence of MDS-CAs. Denoted are the times from first transplantation to any MDS-CA (blue), to the detection of transient MDS-CAs (red), and to the observation of the first among 3 successive MDS-CA examinations (persistent MDS-CAs [green]).
Variables predicting timing of MDS-CA onset
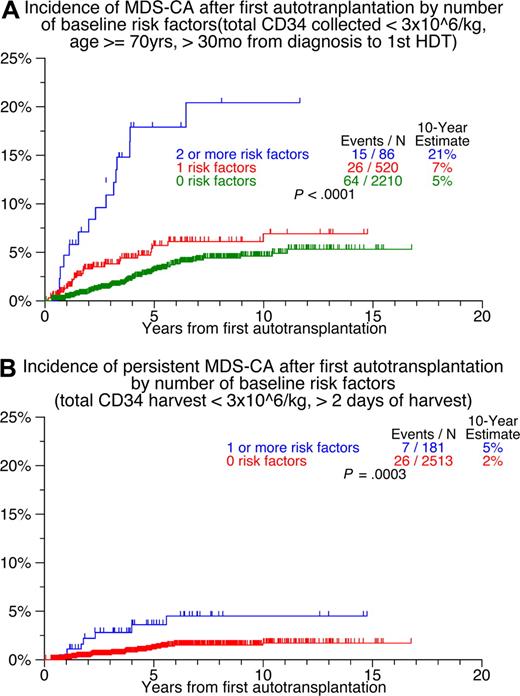
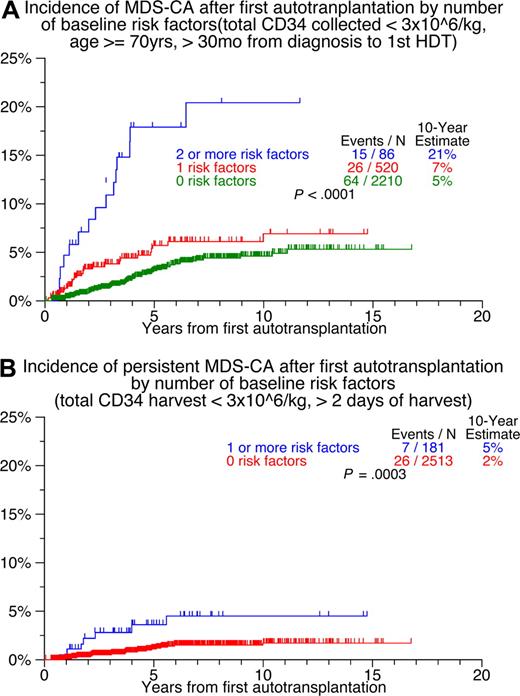
Features associated with MDS-CA development were examined by Cox regression analyses. Among all 105 patients with MDS-CA development (transient or persistent), low CD34 yield (≤ 3 × 106/kg), low platelet recovery level 3 months after first transplantation (< 150 × 109/L), advanced age (≥ 70 years), and longer time interval from MM diagnosis to HDT (> 30 months) were independently associated with MDS-CA development (Table 2 “All 105 patients”). Days of stem-cell collection and low CD34 yield were independently associated with the development of persistent MDS-CAs in 33 patients (Table 2 “33 patients with persistent MDS-CAs”). Thus, the 10-year risk of first MDS-CA was 3% in the absence, 5% in the presence of 1, and 12% in the presence of 2 and more baseline risk factors (excluding platelet recovery) (Figure 2A); for the 33 patients with persistent MDS-CAs, the 10-year estimates were 5% and 2% in the presence of 1 and 0 risk factors, respectively (Figure 2B). Clinical MDS or AML, observed in 26 patients, was observed with similar frequencies in transient and persistent MDS-CA categories (P = .52).
Cumulative incidence of MDS-CAs according to number of risk factors. (A) Transient and persistent MDS-CAs. (B) Persistent MDS-CAs.
Cumulative incidence of MDS-CAs according to number of risk factors. (A) Transient and persistent MDS-CAs. (B) Persistent MDS-CAs.
Time course of MDS-CA development by calendar year and protocol status
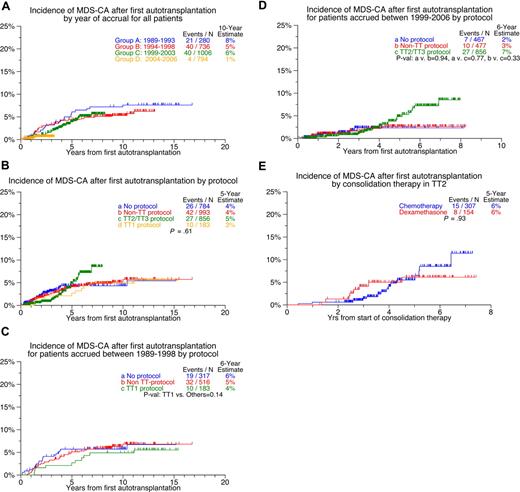
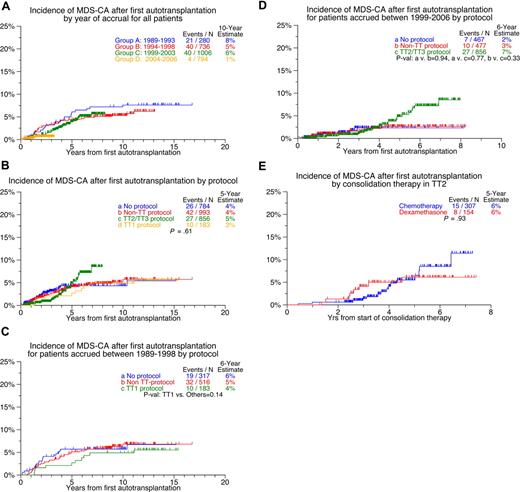
Figure 3 examines the cumulative times of MDS-CA onset in relationship to the calendar year of HDT therapy and protocol- or nonprotocol-based HDT regimens. Patients treated since 1999 seemed to have a delayed onset of MDS-CAs (Figure 3A). Nonprotocol (non-P) and non–TT protocol (non–TT-P) groups experienced as a group an earlier onset of MDS-CAs, whereas such onset appeared delayed in TT2 and TT3 patients (Figure 3B). Beyond 5 years from HDT, there was a projected higher rate of MDS-CAs among TT2 and TT3 patients. Among patients treated prior to 1999, those receiving TT1 tended to develop MDS-CAs less frequently than non–TT-P and non-P groups (Figure 3C). In more recent HDT recipients, the 2-year and 3-year risk of MDS-CAs was low in the 2% to 3% range, especially with TT2 and TT3 protocols; however, the MDS-CA risk seemed to increase among such patients beyond the fourth year after HDT (Figure 3D). There was a provision in TT2 for patients not recovering a platelet count of at least 100 × 109/L to receive, as post-HDT consolidation therapy, dexamethasone instead of combination chemotherapy comprising topoisomerase inhibitors (etoposide, doxorubicin); such patients seemed to have an earlier onset of MDS-CAs, whereas those receiving chemotherapy tended to exhibit an ongoing increased risk of MDS-CAs beyond 5 years after HDT (Figure 3E). No difference in MDS-CA development was observed among patients on the control versus thalidomide arm of TT2 (data not shown). Furthermore, the MDS-CA subtype distribution was similar in the 3 treatment categories (TT-P, non–TT-P, non-P).
Cumulative incidence of MDS-CAs. (A) By calendar year of therapy. (B) According to protocol. (C) According to protocol among patients treated from 1989 to 1998. (D) According to protocol among patients treated from 1999 to 2006. (E) Among patients enrolled in TT2 protocol according to whether consolidation consisted of chemotherapy or dexamethasone.
Cumulative incidence of MDS-CAs. (A) By calendar year of therapy. (B) According to protocol. (C) According to protocol among patients treated from 1989 to 1998. (D) According to protocol among patients treated from 1999 to 2006. (E) Among patients enrolled in TT2 protocol according to whether consolidation consisted of chemotherapy or dexamethasone.
Patient characteristics associated with tertile time intervals to MDS-CAs
Since there were time-dependent differences in MDS-CA development (Figure 3), we examined variables that were associated with early versus late onset of MDS-CAs. As noted in Table 3, significant differences were observed in the tertile distributions of patients with early, intermediate, or late onset of MDS-CA development. TT2 and TT3 recipients had a progressively increasing risk of MDS-CAs with the transition from first to third tertile, which contrasted with the higher early-onset MDS-CA risk with subsequent decline among patients whose time interval from initial MM diagnosis to HDT exceeded 12 months, whose pre-HDT platelet count was in the lowest quartile, and who had elevated CRP levels; a trend was apparent for early-onset MDS-CAs among patients with low CD34 quantities infused with the second transplant (< 3 × 106/kg) and among those who developed the − 7/7q− MDS-CA variety.
MDS-CAs and subsequent survival
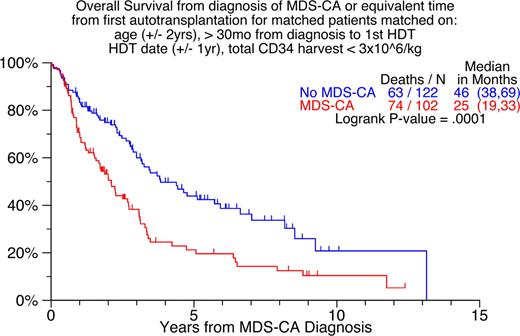
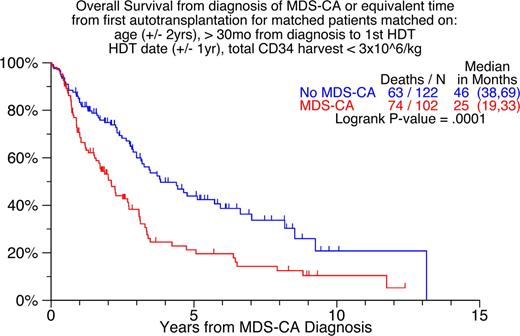
We also examined whether MDS-CAs impacted post-HDT survival in the context of standard pre-HDT prognostic factors (Table 4). Indeed, MDS-CAs (considered as a time-dependent variable) were associated with shortened survival after adjusting for other significant prognostic factors. Forty of the 75 deaths observed among the 105 patients with MDS-CAs were attributable to MM progression, while merely 7 could be traced directly to the consequences of clinical MDS/AML or its treatment; the cause of death in the remaining 28 patients could not be ascertained.
Since the time of onset of MDS-CAs varied greatly (ranging from 154 to 3780 days), a pair-mate analysis matched 95 of the 105 MDS-CA patients with 115 non–MDS-CA patients (Table 2 “All 105 patients”; age within 2 years, transplantation date matched within 1 year, CD34 < 3 × 106/kg, and interval between diagnosis and HDT > 30 months). The survival probability for the MDS-CA group was significantly lower (median, 25 mo vs 69 mo (P < .001) (Figure 4).
Survival of patients with and without MDS-CAs matched on age, HDT date, months from diagnosis to first HDT, and CD34 quantity.
Survival of patients with and without MDS-CAs matched on age, HDT date, months from diagnosis to first HDT, and CD34 quantity.
Discussion
To our knowledge, this report is the largest ever on the prospective detection of potentially treatment-induced MDS by metaphase cytogenetic abnormalities, termed here MDS-CAs, in the context of HDT for MM. Interestingly, MDS-CAs were often only transiently observed. Even in the subgroup of 33 patients in whom MDS-CAs were observed on 3 successive occasions, the detection subsequently of normal metaphases was common. Considering the tight follow-up of all patients (90% of whom returned to our institution at least semiannually), the low incidence of clinical MDS or AML of 1% must be considered accurate.
Predictors of MDS-CAs were older age and hematopoietic stem-cell compromise, as revealed by lower CD34 yield and less complete platelet recovery after the second transplantation. Longer time intervals from MM diagnosis to first HDT probably reflected more extensive prior treatment exposure. Among the 33 patients with persistent MDS-CAs, the 2 independent adverse predictors for such occurrence were low CD34 yield and need for extended apheresis procedures, reflecting damage to hematopoietic stem cells that antedated HDT.
When examined according to calendar year of HDT and type of HDT regimen, no significant difference was observed between patients receiving TT1 primary therapy compared with those with prior treatment exposure elsewhere. Of interest were the differences in the timing of MDS-CA onset related to post-HDT consolidation chemotherapy applied in TT2 and TT3 (late-onset MDS-CAs) and time interval from diagnosis and low platelet count prior to HDT (early-onset MDS-CAs). The latter more likely reflect pre-HDT–inflicted hematopoietic stem-cell damage, whereas in the case of TT2 postconsolidation chemotherapy appears to be the primary culprit; the follow-up in case of TT3 is too short, although it will be interesting to see whether the fewer induction and consolidation cycles applied in TT3 compared with TT2 and the incorporation of bortezomib into TT3 will lower the risk of MDS-CAs. Thus, in the context of our HDT programs for MM, MDS-CAs detected after autotransplantation can be traced to stem-cell compromise as a result of host senescence, pre-HDT, HDT-based, and post-HDT interventions. While clinically largely silent in terms of MDS or AML manifestation, the presence of MDS-CAs contributed independently to shorter survival. We have previously reported on a particularly grave prognosis in patients presenting with an MDS signature within a typical MM karyotype, referred to as MM-MDS-CAs, the occurrence of which we attributed to not only normal hematopoietic cells' but also MM cells' susceptibility to MDS-type damage.26 Such metaphases could be present together with normal diploid, MM-type CAs, and MDS-CAs. The shorter OS in the case of MDS-CAs in this study, however, could not be accounted for by concomitant presence of MM-MDS-CAs (data not shown), which does not rule out the possibility that such abnormalities might have been detectable by interphase FISH analysis.
Most reports on t-MDS are based on the clinical/morphologic diagnosis of MDS or AML developing in the context of HDT following standard-dose chemotherapy, either as consolidation or salvage intervention, so that the critical question of pre-HDT or HDT induction of t-MDS/AML could not be answered. In the present study, applying cytotoxic, growth stimulatory, and immunomodulatory agents for remission maintenance or disease recontrol, dysmyelopoiesis and pancytopenia are common, so that the already difficult task of diagnosing t-MDS early prior to frank leukemic transformation is further aggravated. Critically objective and semiquantitative criteria for MDS/AML detection are based on metaphase detection of MDS-CAs as in our study and the detection of such CAs in interphase nuclei by appropriate molecular probes (interphase FISH),24,25 abnormal in vitro colony growth characteristics, and shortening of telomeres.40
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
This work was supported in part by National Institutes of Health grant CA55819 (B.B., G.T., F.R., J.C.).
National Institutes of Health
Authorship
Contribution: B.B. and G.T. conceptualized and wrote the paper; B.B., G.T., F.R., E.A., M.P.-R., R.T., M.Z., K.H., A.M., and Y.A. conducted clinical research; J.W. performed histopathologic evaluations; J.S. supervised cytogenetic analyses and validated data; M.C.-F. supervised autologous stem cell procurement; J.H., A.H., and J.C. analyzed data.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Bart Barlogie, Myeloma Institute for Research and Therapy, University of Arkansas for Medical Sciences, 4301 W Markham, Little Rock, AR 72205; e-mail: barlogiebart@uams.edu.

![Figure 1. Cumulative incidence of MDS-CAs. Denoted are the times from first transplantation to any MDS-CA (blue), to the detection of transient MDS-CAs (red), and to the observation of the first among 3 successive MDS-CA examinations (persistent MDS-CAs [green]).](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/111/1/10.1182_blood-2007-06-097444/3/m_zh80020811600001.jpeg?Expires=1769096703&Signature=lEp0YOLHD8ekUiP7HEYSRa3dhOrgUnYf52atHiOv94UHSWIKxNWWk3D5iRv4rgLeD2N9gN82hfPQTglYcjjsFpM0jNHcfcNiHT5x3GnTfE1wqG9EtofwvJpub2iokh1B0dl0sX2BiBM0elOTfDF5v0-nOeFIZT34rJlUoL~N~0cebOzS7fYAfTw27L9OnN5OVZ3QqxaYFHHWvzCLKI4YkFHfWuILJRYVVF8F49DVQdu8fjrY0Baaus6OqYNHVfQ8ZsVwF4asOdIMyliDIbTQMp9fasjgjQX7Niyua4-gfnwx8gpHvmQ6hgxmpYZ233QWI5xDnXU06wfY9TwlrqyJPQ__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)

![Figure 1. Cumulative incidence of MDS-CAs. Denoted are the times from first transplantation to any MDS-CA (blue), to the detection of transient MDS-CAs (red), and to the observation of the first among 3 successive MDS-CA examinations (persistent MDS-CAs [green]).](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/111/1/10.1182_blood-2007-06-097444/3/m_zh80020811600001.jpeg?Expires=1769096704&Signature=4FI~lJRODLihN30KoAZxdJDiHp9LJe7AF9w4xGfNDpmZMa6nv59~WgbmCwTLut8I4t2M2PVPueatlC2tfc8mzeyRXyIRuLBaTRHlTHFrFyTSgcMyupzJD3IrH4ZEOdAbB4scQCAfDYyQba5eTxUtznwmBN9vuUd7vWvF0g4F0PkRn1xtZmLjMhGyUeWBJ0X1V5uFj27e0CYOJllzCE3pbM~Te-mZUxd25~~UidFpEIrYq2B6A1j3Fx8j2MWOZQVlzGXaTupTp8ke9qR5ZI3s78hWqZge3e-eC5QXTYUGFApL1BqwQ4USjOAwTl03EfEjZIT86Z4fqc4lUbSXxUUCHA__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)