Abstract
Hypoxia, which commonly associates with respiratory and cardiovascular diseases, provokes an acute inflammatory response. However, underlying mechanisms are not well understood. Here we report that red blood cells (RBCs) induce hypoxic inflammation by producing reactive oxygen species (ROS) that diffuse to endothelial cells of adjoining blood vessels. Real-time fluorescence imaging of rat and mouse lungs revealed that in the presence of RBC-containing vascular perfusion, hypoxia increased microvascular ROS, and cytosolic Ca2+, leading to P-selectin–dependent leukocyte recruitment. However, in the presence of RBC-free perfusion, all hypoxia-induced responses were completely inhibited. Because hemoglobin (Hb) autoxidation causes RBC superoxide formation that readily dismutates to H2O2, hypoxia-induced responses were lost when we inhibited Hb autoxidation with CO or nitrite, or when the H2O2 inhibitor, catalase was added to the infusion to neutralize the RBC-derived ROS. By contrast, perfusion with RBCs from BERK-trait mice that are more susceptible to Hb autoxidation and to hypoxia-induced superoxide production enhanced the hypoxia-induced responses. We conclude that in hypoxia, increased Hb autoxidation augments superoxide production in RBCs. Consequently, RBCs release H2O2 that diffuses to the lung microvascular endothelium, thereby initiating Ca2+-dependent leukocyte recruitment. These findings are the first evidence that RBCs contribute to hypoxia-induced inflammation.
Introduction
Hypoxia is associated with inflammatory diseases, such as acute lung injury (ALI) or cardiovascular conditions with low cardiac output. It is therefore capable of inducing an inflammatory response1 that could further impair organ function through leukocyte accumulation and increased capillary leak.2 However, the mechanisms directly linking hypoxia to inflammation remain unclear. Possible mechanisms include hypoxia-induced activation of the transcription factor, hypoxia-inducible factor-1 (HIF-1), triggering the expression of proinflammatory genes,3 and increased production of mitochondrial reactive oxygen species (ROS), which activate endothelial secretion of leukocyte adhesion receptors, thereby promoting the inflammatory response.4,5 As reviewed,6 the processes that are generally considered a source for ROS include the mitochondrial, the xanthine/xanthine oxidase and the nicotinamide adenine dinucleotide phosphate oxidase systems
Another potential source for ROS that is frequently neglected is the red blood cell (RBC). RBCs contain the largest pool of O2 and are in intimate contact with lung capillaries. The RBC source for ROS is particularly relevant under hypoxic conditions, which causes a dramatic increase in the rate of hemoglobin (Hb) autoxidation,7,8 resulting in increased RBC production of superoxide and hydrogen peroxide. It has been shown that, although RBCs contain an extensive antioxidant system, including superoxide dismutase, catalase, glutathione peroxidase, and thioredoxin, under hypoxic conditions RBC-derived ROS can damage the cell membrane9 and leak of the RBC.10 Under hypoxic conditions, these effects of RBC-generated ROS have been attributed to the increased ROS production coupled with the increased affinity of Hb for the red cell membrane in its deoxygenated quaternary conformation.11,12 With Hb bound to the membrane, the generated ROS can leak of the RBC without being scavenged by the cytoplasmic antioxidant enzymes.10 However, it is not known whether Hb autoxidation in hypoxia yields sufficient RBC-derived ROS to be effective as endothelial activators.
Here we investigated the role of the RBC as a ROS source in the microvascular bed, using real-time fluorescence imaging of the lung that enables time dependent detection of cellular responses in intact alveolocapillary microvessels.5 We exposed lungs to hypoxia while quantifying responses in endothelial cells in situ in lung venular and septal capillaries in terms of ROS production, cytosolic Ca2+ (Ca2+cyt), NO levels, and leukocyte accumulation. These studies revealed that hypoxia induced endothelial proinflammatory responses in a strictly RBC-dependent manner, indicating, for the first time, a role for RBC-derived ROS in hypoxic microvascular pathology.
Methods
Animals
Sprague-Dawley (500 g) rats were purchased from Charles River Breeding Laboratories (Portage, MI). BERK-trait mice were obtained as a gift from Dr M. Fabry (Albert Einstein College of Medicine, New York, NY). This mouse contains 100% human α-globin, 15% human βS-globin, and 85% mouse β-globin.13,14 C57BL/6J (C57BL; The Jackson Laboratory, Bar Harbor, ME) mice were used as control.
Fluorescent dyes and reagents
We purchased fura 2AM, 2′,7′-dichlorofluorescein-diacetate (DCFH-DA) and 4-amino-5-methylamino-2′,7′-difluorofluorescein (DAF-FM di-acetate) from Invitrogen (Carlsbad, CA); catalase, polyethylene glycol catalase, sodium nitrite, sodium azide, sodium cyanate, 1,2-Bis(2-aminophenoxy)ethane-N,N,N′,N′-tetra-acetic acid tetrakis(acetoxymethyl ester), and NG-nitro-L-arginine methyl ester (L-NAME) from Sigma-Aldrich (St Louis, MO); and carbon monoxide (CO) from Airgas (Paterson, NJ). Vehicle for dyes and other agents was N-2-hydroxyethylpiperazine-N′-2-ethanesulfonic acid (HEPES) buffer (150 mM Na+, 5 mM K+, 1.0 mM Ca2+, 1 mM Mg2+, and 20 mM HEPES, pH 7.4) containing 4% dextran (70 kDa) and 1% fetal bovine serum at pH 7.4 and osmolarity of 295 mosM. Mouse antirat P-selectin mAb, RMP-1 was a gift of Dr A.C. Issekutz (Department of Pediatrics, Dalhousie University, Halifax, NS). Goat antirat αIIb IgG (10 μg/mL; Santa Cruz Biotechnology, Santa Cruz, CA) was used as control antibody.
Lung preparation
Using our reported methods,15 we established the isolated, perfused lung preparation using lungs of the anesthetized rat or mouse (3.5% halothane inhalation and 35 mg/kg intraperitoneal sodium pentobarbital). Through cannulae inserted in the pulmonary artery and the left atrium, we perfused the lung vasculature at 37°C. For rat lung, we perfused with homologous rat blood. For mouse lung, we perfused with a leukocyte-free RBC suspension (20% hematocrit) in HEPES buffer. We held pulmonary artery (Ppa) and left atrial pressures constant at 10 and 2 cmH2O, respectively. Perfusion rates were 14 and 1 mL/min for rat and mouse lungs, respectively. Under baseline conditions, we held the lungs at constant inflation at airway pressure of 5 cmH2O with a gas mixture of 30% O2, 5% CO2, and 65% N2.
Single microvascular perfusion
To avoid hemolysis in the imaged microvessel, we filled a reservoir with hemolysis-free, freshly isolated and HEPES-buffer resuspended RBCs. We then directly pump-perfused these RBCs into the imaged microvessels through a microcatheter placed in a small branch of the pulmonary vein. The infused RBCs did not recirculate. In separate experiments, we centrifuged samples of wild-type (WT) or BERK-trait RBC collected from the microcatheter effluent to determine free Hb. No free Hb was detectable, indicating that perfusing RBCs through the microcatheter did not cause hemolysis. The microcatheter procedure was not required in mouse lungs because perfusion with RBC-HEPES did not cause hemolysis as determined by the aforementioned centrifugation method.
To investigate the effect of leukocyte and platelets, we infused isolated leukocytes in combination with isolated platelets into the experimental capillary. For leukocyte isolation 5 mL of whole blood was centrifuged and platelet-rich plasma was removed. The buffy coat was separated and 15 μL of 0.05% fluorescent dye Rhodamine 6G per 1 mL was added. After centrifugation (2000g, 10 minutes), leukocytes were separated and resuspended with 10 mL Ca2+-free HEPES (0.5 × 109 leukocytes/mL) and reinjected shortly before venular imaging. For platelet isolation, 5 mL whole blood was mixed with 1.5 mL phosphate-buffered saline containing 15.2 μM citric acid, 30 μM trisodium citrate, 40 μM dextrose, and 1.5 μg PGE1. After centrifugation of the resulting blood mixture, 500 μL platelet-rich plasma was centrifuged again (2000g, 10 minutes). The supernatant was removed. The pellet containing platelets was resuspended with 2 mL HEPES (0.2 × 109 platelets/mL) and reinjected before imaging was performed.
Hypoxia induction
In preliminary experiments, inflating lungs with hypoxic gas failed to decrease the lung's venous pO2 below normoxic levels, probably because O2 diffusing from the ambient air across the exposed lung surface oxygenated the blood. Hence, to prevent this O2 diffusion, we covered the lungs with gas-tight plastic as in a previous study.16 In plastic-wrapped lungs, switching the inflation gas to a hypoxic mixture containing 95% N2 and 5% CO2 decreased pO2 of the lung venous blood from 175 plus or minus 9 mmHg at baseline, to 22 plus or minus 4 mmHg (P < .05; n = 6). The ensuing increase of pulmonary arterial pressure from 9 plus or minus 2 cm H2O to 13 plus or minus 4 cmH2O (P < .05; n = 5) indicated the presence of hypoxic pulmonary vasoconstriction. Blood pCO2 was constant throughout (39 ± 6 mmHg).
ROS, Ca2+cyt, and NO imaging
We viewed venular capillaries by a CCD camera (Coolsnap, Photometrics, Tucson, AZ) mounted on an epifluorescence microscope (Nikon, Melville, NY) fitted with a 40× water-immersion objective (Nikon). We quantified capillary fluorescence using image analysis software (Metafluor; Molecular Devices, Sunnyvale, CA). For quantification of ROS, Ca2+cyt, and NO in endothelial cells of capillary venules, we loaded the cells by 20-minute capillary infusions of the dyes DCFDH-DA (20 μM), fura-2 AM (10 μM), and DAF-FM (10 μM), respectively, as previously described.5
RBC procedures
Blood was collected by cardiac puncture and centrifuged (2000g at 4°C for 10 minutes). To remove white cells, the supernatant and the buffy coat were separated. The remaining RBC-rich pellet was resuspended with HEPES and centrifuged again. This procedure was repeated 3 times. A small portion of isolated RBCs were labeled with fluorescein isothiocyanate (FITC) as previously described.17 The native and FITC-labeled RBCs were resuspended in HEPES and reinfused. In several experiments we modified the isolated RBCs by the following procedures before microinfusing them into experimental microvessels: (1) CO. To replace O2 bound to Hb with CO, the RBCs were flushed with 100% CO for 5 minutes. Excess CO was then removed by flushing with N2. Because of the slow off rate for CO,18 CO stays bound to Hb. (2) Azide. To inhibit RBC catalase, RBCs were treated with 1 mM azide for 10 minutes.19 (3) Nitrite. To oxidize Hb, RBCs were treated with 5 mM nitrite for 5 minutes. In the presence of O2, nitrite oxidizes Hb producing nitrate20 ; hence, no reduction of nitrite to NO takes place. Methemoglobin formation was indicated by a color change. Excess azide and nitrite were removed by suspending the cells in buffer and centrifuging the suspension. Then, supernatant containing the unreacted nitrite was removed. (4) Cyanate. To inhibit Hb binding to the cytoplasmic end of membrane band 3, RBCs were treated with 250 μM sodium cyanate for 10 minutes. Cyanate reacts with the alpha amino groups of Hb,21 inhibiting the binding of Hb to the membrane.22,23 The excess cyanate was removed by suspending the cells in buffer and centrifuging the suspension. The supernatant containing unreacted cyanate was removed.
Heme degradation products
Rat RBCs were lysed in water and the Hb concentration determined spectrophotometrically. The Hb concentration was adjusted to 50 μM followed by determination of fluorescence (excitation, 321 nm; emission, 465 nm). Oxyhemoglobin (50 μM) in 50 mM in potassium phosphate buffer was transferred to a septum-sealed cuvette. While slowly stirring the solution, the gas phase above the solution was flushed with argon until the hemoglobin was 50% deoxygenated. The cuvette was sealed and incubated at 37°C for 12 hours. The control sample was incubated without deoxygenation of oxyhemoglobin. Heme degradation products were determined by fluorescence quantification (excitation, 321 nm; emission, 465 nm) as described.19,24,25
Determination of microhemodynamics and leukocyte-endothelial interactions by intravital fluorescence microscopy
RBC velocity and leukocyte kinetics were analyzed offline from the digital recordings using image analysis software (MetaMorph, Molecular Devices). For RBCs, we determined mean velocity of 30 FITC-labeled cells passing a defined vascular locus. For leukocytes, we defined rolling for cells flowing at the vessel margin at a velocity less than 50% of the mid-vessel blood velocity. We defined adherent leukocytes as cells that did not move for 30 seconds.
Statistics
Data are mean plus or minus SE. Group comparisons were made using ANOVA on rank data followed by the Dunn test. Repeated measurements were tested using Mann-Whitney Rank Sum test. Statistical analyses were conducted by computer software (SigmaStat; Jandel SPSS, Chicago, IL) with significance accepted at P less than .05.
Results
Endothelial ROS
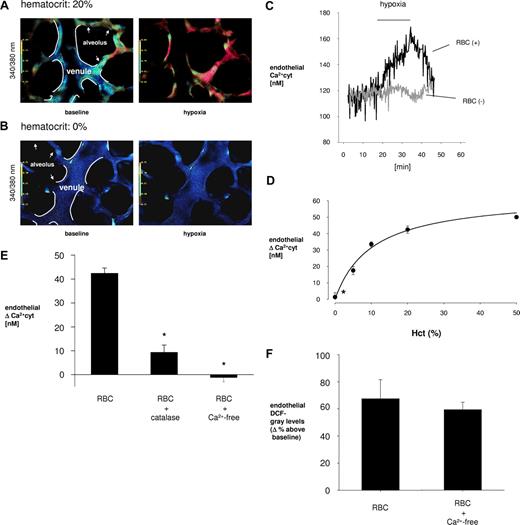
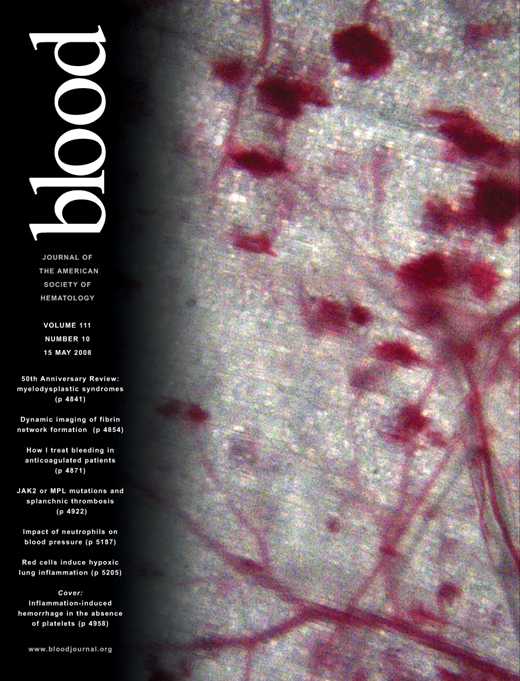
We detected endothelial ROS in terms of DCF fluorescence in DCFH-DA-loaded capillaries of rat lungs. During baseline inflation, a 30-minute capillary perfusion with isolated, HEPES resuspended RBCs at hematocrit of 20% evoked low-grade, fluorescence in sporadic endothelial cells (Figure 1A left). In the same capillaries, hypoxic inflation increased endothelial fluorescence almost throughout the capillary (Figure 1A right), indicating increase in endothelial ROS levels. During the 30-minute hypoxic period, the fluorescence increase commenced in approximately 10 minutes and then continued to increase progressively (Figure 1C).
Endothelial ROS in lung microvessels in situ. (A,B) Color-coded endothelial DCF fluorescence in venules (V) and septal capillaries (S) under normoxic (left) and hypoxic (right) conditions. Vessel margins are depicted (white lines). The alveolar septum is indicated (arrows). Venules were given RBC-containing perfusion at indicated hematocrits. (C) Tracings of DCF fluorescence intensity from an identical endothelial cell at baseline and hypoxic conditions. Perfusate was RBC-free or RBC-containing (hematocrit, 20%) with or without catalase (50 U/mL) replicated 5 times. (D) Hematocrit (Hct) dependency of endothelial DCF fluorescence. Data obtained after 30 minutes of hypoxia are mean plus or minus SE (n = 4 each point; *P < .05 vs hematocrit of 20%). (E) Group data are for hypoxia-induced responses in venules given RBC-containing perfusions (hematocrit, 20%). The unfilled bar corresponds to pO2 of 40 mmHg attained after 17 minutes of hypoxia. The bar immediately to the right corresponds to pO2 of 21 mmHg at 30 minutes of hypoxia exposure. For the other bars, RBCs were perfused together with catalase (50 U/mL) or RBCs were pretreated with the indicated agents (L-NAME, 250 μM; azide, 1 mM; nitrite, 5 mM). Data are mean plus or minus SE; n = 5 for each bar (*P < .05 vs untreated RBC perfusion at pO2 of 21 mmHg, hematocrit of 20%). (F) Data are for venules after 30 minutes of hypoxia. RBC indicates RBCs from wild-type (WT) and BERK-trait (BT) mice were perfused (hematocrit, 20%) in WT and BT lungs as indicated. Catalase (50 U/mL) was included in the perfusion as indicated. Data are mean plus or minus SE; n = 5 for each group (*P < .05 vs first bar; §P < .05 vs 3rd bar).
Endothelial ROS in lung microvessels in situ. (A,B) Color-coded endothelial DCF fluorescence in venules (V) and septal capillaries (S) under normoxic (left) and hypoxic (right) conditions. Vessel margins are depicted (white lines). The alveolar septum is indicated (arrows). Venules were given RBC-containing perfusion at indicated hematocrits. (C) Tracings of DCF fluorescence intensity from an identical endothelial cell at baseline and hypoxic conditions. Perfusate was RBC-free or RBC-containing (hematocrit, 20%) with or without catalase (50 U/mL) replicated 5 times. (D) Hematocrit (Hct) dependency of endothelial DCF fluorescence. Data obtained after 30 minutes of hypoxia are mean plus or minus SE (n = 4 each point; *P < .05 vs hematocrit of 20%). (E) Group data are for hypoxia-induced responses in venules given RBC-containing perfusions (hematocrit, 20%). The unfilled bar corresponds to pO2 of 40 mmHg attained after 17 minutes of hypoxia. The bar immediately to the right corresponds to pO2 of 21 mmHg at 30 minutes of hypoxia exposure. For the other bars, RBCs were perfused together with catalase (50 U/mL) or RBCs were pretreated with the indicated agents (L-NAME, 250 μM; azide, 1 mM; nitrite, 5 mM). Data are mean plus or minus SE; n = 5 for each bar (*P < .05 vs untreated RBC perfusion at pO2 of 21 mmHg, hematocrit of 20%). (F) Data are for venules after 30 minutes of hypoxia. RBC indicates RBCs from wild-type (WT) and BERK-trait (BT) mice were perfused (hematocrit, 20%) in WT and BT lungs as indicated. Catalase (50 U/mL) was included in the perfusion as indicated. Data are mean plus or minus SE; n = 5 for each group (*P < .05 vs first bar; §P < .05 vs 3rd bar).
During the hypoxic period, an increase in endothelial ROS was associated with progressive decrease in blood pO2. Thus, 17 minutes after induction, when pO2 was 40 mmHg, DCF intensity increased 18% plus or minus 7% above baseline (Figure 1E unfilled bar). However, after 30 minutes, when pO2 was 22 mmHg, the intensity increased further to 67% plus or minus 14% above baseline (Figure 1E first filled bar from left). Subsequent reinstatement of baseline inflation decreased the fluorescence to control levels within approximately 10 minutes (Figure 1C). This recovery response was attributable to the fact that endothelial cells in situ expel DCF,5 causing fluorescence decrease after relief of the ROS-generating stimulus.
In marked contrast to these responses in RBC-perfused vessels, during perfusion with RBC-free vehicle, the switch from baseline to hypoxic inflation failed to increase endothelial DCF fluorescence (Figure 1B,C). These findings indicate that RBC determined the hypoxia-induced endothelial ROS increase in these capillaries.
Perfusion of capillaries at different RBC concentrations for 30 minutes indicated that the hypoxia-induced endothelial ROS increase was hematocrit dependent (Figure 1D). The relationship was nonlinear, indicating that the RBC effect was detectable even at the physiologically low hematocrit of 10%. Indeed, endothelial fluorescence responses were not statistically different for groups perfused with RBCs at 10%, 20%, and 50% hematocrit. Only severe hematocrit reductions caused significant decrease of the hypoxia-induced effect (Figure 1D).
To determine the specific ROS responsible for the enhanced endothelial fluorescence, we perfused the capillaries with RBCs at 20% hematocrit together with catalase, the cell-impermeable H2O2-hydrolyzing agent. In separate experiments, we infused RBCs that we previously treated with azide, the cell-permeable inhibitor of RBC catalase.26 Catalase blocked the hypoxia-induced increase of endothelial fluorescence (Figure 1C,E), indicating that the effect resulted from paracrine transfer of H2O2 from RBCs to endothelial cells. Azide-treated RBCs augmented the hypoxia-induced endothelial DCF response (Figure 1E), indicating that inhibition of RBC catalase by azide increased RBC-derived H2O2. Given alone under baseline conditions, catalase had no effects on endothelial DCF fluorescence (not shown). These findings indicated that the endothelial DCF responses in hypoxia were attributable to RBC-derived H2O2. To determine the role of NO, we infused the NO synthase inhibitor, L-NAME together with RBCs. The lack of an L-NAME effect on the hypoxia-induced endothelial DCF response (Figure 1E) indicated that NO was not involved.
Hypoxia generates ROS in conjunction with Hb autoxidation, which increases markedly during partial deoxygenation of Hb.27 To determine whether this reaction was responsible for the ROS transferred to endothelial cells, we infused lung capillaries with RBCs pretreated with CO or nitrite. CO displaces O2 from Hb and nitrite oxidizes Hb. These modified Hb do not have bound O2 and, therefore, do not undergo autoxidation to produce ROS. In both groups, the pretreated RBCs failed to evoke the endothelial fluorescence increase in hypoxia (Figure 1E), pointing to hypoxia-induced Hb autoxidation as the mechanism underlying the enhanced ROS release from RBCs.
To further test the autoxidation hypothesis, we established conditions in which hypoxia produces proportionally more deoxygenated Hb and increased Hb autoxidation. For this purpose, we conducted studies on the BERK-trait mouse. The O2 binding curve of the BERK-trait Hb is shifted to the right relative to WT Hb. Because of this lower O2 affinity, hypoxia-induced desaturation of Hb down to oxygenation levels of 50% to 60% maximizes the rate of Hb autoxidation.28 Consistent with this expectation, BERK-trait Hb undergoes more rapid autoxidation.29 Compared with RBCs from WT mice, capillary infusions of BERK-trait RBC in lungs of BERK-trait, or WT mice induced more than a 2-fold increase in the hypoxia-induced DCF fluorescence in capillary endothelium (Figure 1F). Again, inclusion of catalase in the perfusion markedly abrogated the hypoxia-induced effect for BERK-trait RBCs (Figure 1F), further affirming the role of RBC-derived H2O2 in these responses.
Heme degradation
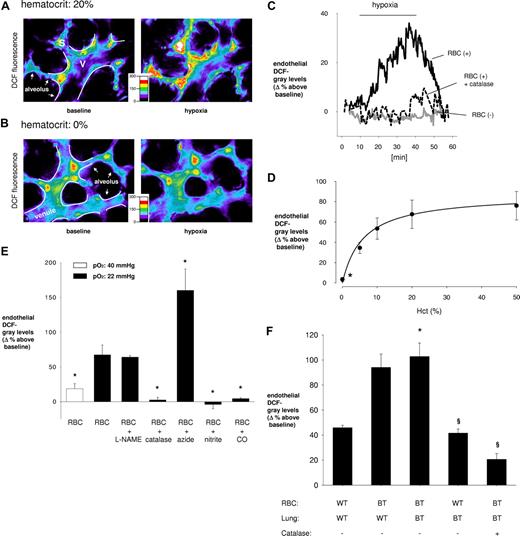
Although Hb is responsible for the production of RBC ROS, most of these ROS are quenched by catalase, superoxide dismutase, and glutathione peroxidase in the RBC cytosol.19 The transfer of RBC ROS to lung microvascular endothelium is therefore dependent on the fraction of the ROS that escape the cytosolic antioxidants in RBCs. To detect this fraction, we quantified fluorescent heme degradation products that form in RBC as a result of Hb autoxidation.26 Formation of these fluorescent products is enhanced by inhibition of RBC catalase19 but is not affected by extracellular oxidants. In our experiments, enhanced autoxidation of Hb resulting from hypoxia increased heme degradation (Figure 2A). In the lung perfusion experiment, the hypoxia-induced enhanced DCF fluorescence in endothelial cells was associated with higher levels of heme degradation in the perfused RBC (Figure 2B). This directly links Hb autoxidation to the increased endothelial DCF fluorescence. Consistent with the increased DCF fluorescence after azide treatment, heme degradation was dramatically increased for azide-treated RBCs (Figure 2C).
Heme degradation products in rat RBCs. Fluorescence of heme degradation products is shown for Hb incubated (12 hours, 37°C) at pO2 of 100 (normoxic) or 21 (hypoxic) mmHg (n = 4; A), Hb of RBC perfused through lungs inflated under normoxic and hypoxic conditions (n = 4; B), and Hb of nontreated and azide- (C) or cyanate- (D) treated RBCs. The endothelial DCF response is also shown for cyanate-treated RBCs (E) and perfused through lungs inflated under normoxic and hypoxic conditions (n = 3). Data are mean plus or minus SE (#P < .05 vs baseline [panels A,B, 1st bar]; *P < .05 vs hypoxic RBC [panel C, 1st bar]; **P < .05 vs hypoxic RBC [panel E, 1st bar]).
Heme degradation products in rat RBCs. Fluorescence of heme degradation products is shown for Hb incubated (12 hours, 37°C) at pO2 of 100 (normoxic) or 21 (hypoxic) mmHg (n = 4; A), Hb of RBC perfused through lungs inflated under normoxic and hypoxic conditions (n = 4; B), and Hb of nontreated and azide- (C) or cyanate- (D) treated RBCs. The endothelial DCF response is also shown for cyanate-treated RBCs (E) and perfused through lungs inflated under normoxic and hypoxic conditions (n = 3). Data are mean plus or minus SE (#P < .05 vs baseline [panels A,B, 1st bar]; *P < .05 vs hypoxic RBC [panel C, 1st bar]; **P < .05 vs hypoxic RBC [panel E, 1st bar]).
Cyanate-reacted RBCs
The heme degradation and DCF fluorescence data implied that ROS generated by Hb autoxidation leaked of the RBCs. RBCs possess high levels of cytosolic superoxide dismutase and catalase that are likely to quench ROS generated by Hb autoxidation. However, it is possible that the leakage of ROS from RBC involves Hb binding to band 3 of the red cell membrane.22,30 The assumption is that ROS generated near the surface of the RBC membrane escape the cell before being quenched by antioxidant enzymes in the RBC cytosol.10 To test this possibility, we used cyanate to react with the terminal α-amino groups of Hb.21 This reaction inhibits Hb binding to the membrane22,23 and would therefore be expected to decrease both the heme degradation and the capillary DCF fluorescence response during hypoxia. Our experiments indicate that, with cyanate-reacted RBCs, the hypoxia-induced increase in heme degradation was not significant (Figure 2D). At the same time, the in vitro pretreatment of RBCs with cyanate inhibited the hypoxic-induced increase in endothelial DCF fluorescence (Figure 2E). These results establish a role of Hb-membrane binding in ROS release from RBCs.
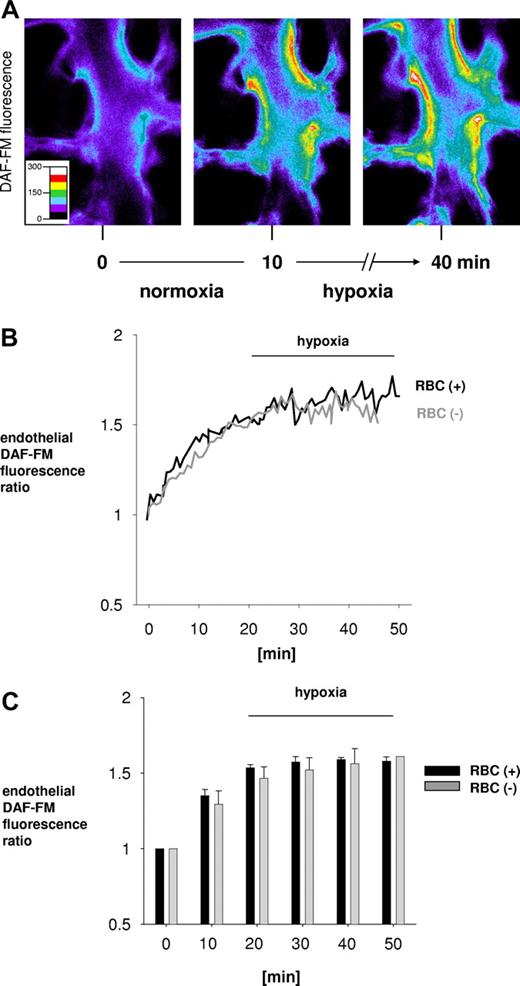
Endothelial Ca2+
Because hypoxia-induced cell-signaling effects are not known in situ, we quantified Ca2+cyt and NO in endothelial cells of rat lung using the dyes fura 2 and DAF-FM, respectively.5,31 Ca2+cyt responses were similar to those of DCF fluorescence in that, in the presence of RBCs at 20% hematocrit, Ca2+cyt progressively increased during the hypoxic period and subsequently declined after switching back to baseline conditions (Figure 3A,C). The Ca2+cyt response to hypoxia was hematocrit dependent (Figure 3B,D), and the response was inhibited by addition of catalase in the RBC-containing perfusion (Figure 3E). Further, perfusion of RBC at 20% hematocrit in Ca2+-free vehicle completely blocked the hypoxia-induced Ca2+cyt response (Figure 3E) but not the increase in endothelial DCF fluorescence (Figure 3F).
Endothelial Ca2+cyt. Data are mean plus or minus SE; n = 5 for each bar (*P < .05 vs first bar). (A,B) Pseudocolor-coded 340:380 ratio for fura 2-loaded capillary endothelial cells under baseline (left) and hypoxic (right) conditions. Vessel margins are depicted (white lines). Alveolar septum is indicated (arrows). Venules are perfused RBC-containing or RBC-free solutions as indicated. (C) Tracings show time-dependent changes in the presence or absence of RBCs in vascular perfusion replicated 6 times. (D) Hematocrit (Hct) dependency of endothelial Ca2+ after 30 minutes of hypoxia exposure. *P < .05 vs HCT: 20%. (E) Bars represent venular group data for indicated perfusion conditions 30 minutes after hypoxic lung inflation. RBC indicates hematocrit = 20%; catalase, 50 U/mL; Ca2+-free, perfusion was Ca2+ depleted. (F) Bars represent RBC-containing perfusions under control and Ca2+-free conditions.
Endothelial Ca2+cyt. Data are mean plus or minus SE; n = 5 for each bar (*P < .05 vs first bar). (A,B) Pseudocolor-coded 340:380 ratio for fura 2-loaded capillary endothelial cells under baseline (left) and hypoxic (right) conditions. Vessel margins are depicted (white lines). Alveolar septum is indicated (arrows). Venules are perfused RBC-containing or RBC-free solutions as indicated. (C) Tracings show time-dependent changes in the presence or absence of RBCs in vascular perfusion replicated 6 times. (D) Hematocrit (Hct) dependency of endothelial Ca2+ after 30 minutes of hypoxia exposure. *P < .05 vs HCT: 20%. (E) Bars represent venular group data for indicated perfusion conditions 30 minutes after hypoxic lung inflation. RBC indicates hematocrit = 20%; catalase, 50 U/mL; Ca2+-free, perfusion was Ca2+ depleted. (F) Bars represent RBC-containing perfusions under control and Ca2+-free conditions.
To test whether the Ca2+cyt response during hypoxia could be induced by blood cells other than RBCs, in the experimental microvessel we infused leukocytes and platelets. However, because in 2 experiments the infusion of leukocytes and platelets alone did not change endothelial Ca2+cyt concentrations during hypoxia (baseline, 115 ± 5 nM; hypoxia, 116 ± 6 nM), we did not pursue further studies. Plasma may contain antioxidants that potentially scavenge the ROS leaking of RBCs during hypoxia. We therefore perfused the experimental venule with whole blood. In hypoxia, this infusion increased endothelial Ca2+cyt 48% plus or minus 8% above baseline (P < .05; n = 3). Taking these findings together, we interpret that the hypoxia-induced endothelial Ca2+cyt increase resulted from external Ca2+ entry induced by RBC-derived H2O2 and not from nonspecific leukocyte or plasma factors.
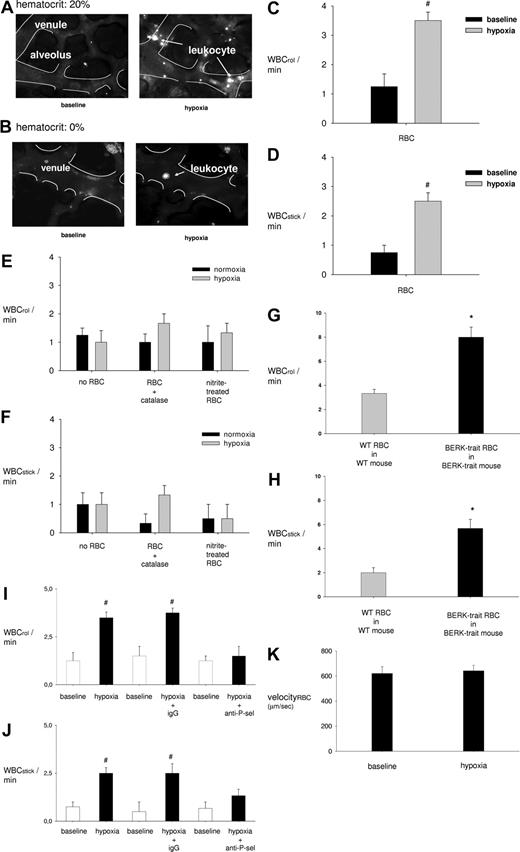
Endothelial NO
The progressive increase of capillary DAF fluorescence at baseline reflected ongoing NO production in endothelial cells (Figure 4). Hypoxia abolished the progressive increase of DAF fluorescence both during RBC-containing and RBC-free perfusions (Figure 4B,C), indicating that hypoxia suppressed NO production in these capillaries in an RBC-independent manner.
DAF fluorescence showing endothelial NO production in lung venular capillaries. (A) Capillaries loaded with DAF-FM. Images were obtained under normoxic conditions (left) and 0 (middle) and 30 (right) minutes after switching to hypoxia. (B) Tracings of DAF-FM fluorescence in a single endothelial cell in a venular capillary that was perfused at either 0% (gray) or 20% (black) hematocrit. (C) Group data show DAF-FM fluorescence as ratio of initial (0 minutes). Data are mean plus or minus SE; n = 4 each bar.
DAF fluorescence showing endothelial NO production in lung venular capillaries. (A) Capillaries loaded with DAF-FM. Images were obtained under normoxic conditions (left) and 0 (middle) and 30 (right) minutes after switching to hypoxia. (B) Tracings of DAF-FM fluorescence in a single endothelial cell in a venular capillary that was perfused at either 0% (gray) or 20% (black) hematocrit. (C) Group data show DAF-FM fluorescence as ratio of initial (0 minutes). Data are mean plus or minus SE; n = 4 each bar.
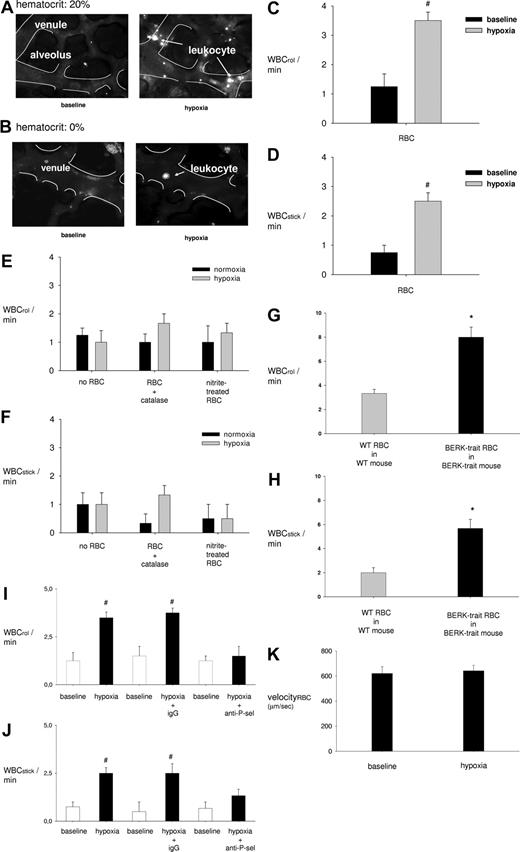
Leukocyte adhesion
In venular capillaries perfused with RBCs in combination with leukocytes under baseline conditions, most rhodamine 6G-labeled leukocytes flowed freely, with only few becoming immobilized by endothelial adherence (Figure 5A left). By contrast, hypoxia markedly increased endothelial leukocyte adherence in the presence of RBCs (Figure 5A right) but not when RBCs were excluded from the capillary perfusion (Figure 5B right). The group data show that, in the presence of RBCs, hypoxia enhanced 3-fold the numbers of both rolling (Figure 5C) and sticking (Figure 5D) leukocytes on the endothelium. The effects were RBC dependent because, in vessels given RBC-free perfusion, the rolling (Figure 5E) and sticking (Figure 5F) responses were completely blocked. These responses to hypoxia were also inhibited in the presence of nitrite- or catalase-treated RBCs (Figure 5E,F) but were augmented in the presence of BERK-trait RBCs (Figure 5G,H). In septal capillaries also, the rate of leukocyte adherence increased from 1.9 plus or minus 0.4/min during baseline to 6.0 plus or minus 0.7/min during hypoxia (n = 4). This response was also inhibited when leukocytes were infused either in combination with catalase (3.3 ± 0.8/min, n = 4) or in combination with nitrite-treated RBC (2.4 ± 0.8/min, n = 4).
Leukocyte-endothelial cell interactions in lung capillaries. (A,B) Images show rhodamine-6G–labeled leukocytes (white dots) in venular capillaries margins of which are outlined (white lines). At hematocrit of 20%, whereas few leukocytes adhere to the venular endothelium under baseline conditions (top left), leukocyte attachment to the endothelium is greater after 30 minutes of hypoxia (top right). By contrast, at hematocrit of 0% hypoxia causes no leukocyte adhesion (bottom right). (C-K) Group data show leukocyte rolling (WBCrol/min) and sticking (WBCstick/min) rates and RBC velocity (k) for normoxia (baseline) and after 30 minutes of hypoxia (hypoxia) under the indicated conditions. Vessels were perfused at 20% hematocrit except as indicated. anti–P-sel indicates P-selectin mAb. #P < .05 vs baseline (panels C,D,I,J); *P < .05 versus WT-RBC in WT-lung (1st bar, panels G,H).
Leukocyte-endothelial cell interactions in lung capillaries. (A,B) Images show rhodamine-6G–labeled leukocytes (white dots) in venular capillaries margins of which are outlined (white lines). At hematocrit of 20%, whereas few leukocytes adhere to the venular endothelium under baseline conditions (top left), leukocyte attachment to the endothelium is greater after 30 minutes of hypoxia (top right). By contrast, at hematocrit of 0% hypoxia causes no leukocyte adhesion (bottom right). (C-K) Group data show leukocyte rolling (WBCrol/min) and sticking (WBCstick/min) rates and RBC velocity (k) for normoxia (baseline) and after 30 minutes of hypoxia (hypoxia) under the indicated conditions. Vessels were perfused at 20% hematocrit except as indicated. anti–P-sel indicates P-selectin mAb. #P < .05 vs baseline (panels C,D,I,J); *P < .05 versus WT-RBC in WT-lung (1st bar, panels G,H).
Leukocyte rolling and sticking responses to hypoxia were also completely blocked when we included the mAb, RMP-1 that inhibits leukocyte binding to P-selectin (Figure 5I,J). Infusion of a nonspecific, isotype-matched mAb had no inhibitory effect (Figure 5I,J), indicating that, in the presence of RBC, hypoxia caused P-selectin–dependent venular leukocyte accumulation. The baseline RBC velocity remained unchanged during hypoxia (Figure 5K), ruling out decreases in velocity as contributing to leukocyte adherence. Taken together, these findings indicate that, in hypoxia, RBC-derived H2O2, resulting from hemoglobin autoxidation-induced leukocyte accumulation in lung venules.
Discussion
Our findings indicate that hypoxia increased endothelial DCF fluorescence of lung microvessels in a hematocrit-dependent manner. We point out that hypoxia caused no changes of DCF fluorescence in capillaries given RBC-free perfusion, indicating that intrinsic mechanisms of endothelial ROS production were not activated. Importantly, the hypoxia-induced response was blocked by adding catalase to RBC-containing perfusion. Because endothelial cells,32 including those of lung capillaries,5 do not internalize catalase unless the enzyme is given in complex with polyethylene glycol, the DCF inhibition indicates that catalase hydrolyzed H2O2 in the extracellular space of the vascular lumen, not in the endothelial cytosol. Taking these findings together with the hematocrit dependence, we conclude that, in hypoxia, RBC-derived H2O2 diffused to lung microvessels, increasing endothelial DCF fluorescence.
To determine underlying RBC mechanisms, we considered the role of Hb autoxidation in which electron transfer from iron to heme-bound O2 induces superoxide production.8 The bulk of the superoxide anions are dismutated by superoxide dismutase to H2O2. This process is slow under normoxic conditions but increases markedly with the onset of hypoxia. Subsequently, autoxidation decreases progressively as decreasing O2 levels fail to sustain ROS production. Autoxidation under hypoxic conditions has been attributed to increased flexibility in the heme pocket of partially oxygenated Hb.33,34 This flexibility facilitates the nucleophilic displacement of bound O2 by the distal histidine, forming superoxide.27
We tested the role of Hb autoxidation in several experiments in which we perfused RBC-containing Hb that could not be autoxidized. Thus, because of the higher affinity of Hb for CO, in CO-equilibrated RBC, CO replaces O2, thereby blocking autoxidation.18 We also reacted RBCs with nitrite, which oxidizes Fe(II) hemes to Fe(III) hemes that do not bind O2.20 Being already oxidized, Fe(III) hemes do not undergo autoxidation. Accordingly, these modifications completely blocked the hypoxia-induced increase of endothelial DCF fluorescence (Figure 1E).
The importance of Hb autoxidation in the DCF response was revealed in BERK-trait mice that possess Hb with diminished O2 affinity,28 which more readily becomes partially oxygenated and is therefore more prone to Hb autoxidation during hypoxia.8,27 Our findings indicate that perfusion with BERK-trait RBC augmented the DCF fluorescence. Responses to BERK-trait RBC were similar in BERK-trait or WT lungs, ruling out the involvement of nonspecific factors in the endothelial response. Hence, in hypoxia, Hb autoxidation was responsible for the production of RBC-derived H2O2.
The bulk of superoxide anions formed in RBC are dismutated by superoxide dismutase to H2O2, which is neutralized by catalase, glutathione peroxidase, or thioredoxin. These very efficient antioxidant systems present in the RBCs would be expected to neutralize even the elevated ROS generated during hypoxia. To demonstrate that the ROS generated can, nevertheless, escape from the RBCs and diffuse to endothelial cells, we inhibited RBC catalase with azide and thereby showed a marked increase in the DCF fluorescence (Figure 1E).
As a measure of ROS that are not neutralized by RBC antioxidants, we quantified heme degradation. These degradation products are produced when non-neutralized H2O2 reacts with Hb.4 This is the same pool of non-neutralized H2O2 that leaks of the RBCs to the microvessels. Heme degradation increased when we perfused RBCs in hypoxic lungs, and it increased further when RBC catalase was inhibited by azide, consistent with the observed increase in DCF fluorescence.
Our heme degradation studies suggest an explanation of how ROS escape the extensive RBC antioxidant system. Of the heme degradation products formed in RBCs, 90% have been shown to be formed on the RBC membrane (E.N., J.M.R., unpublished observations, 2007). We point out that the membrane anion channel, band 3, is also a site where Hb binds.23 This suggests that the primary site of heme degradation is in the membrane-associated fraction of Hb. Consequently, the ROS produced on the membrane may be less accessible to the cytoplasmic antioxidant enzymes catalase and superoxide dismutase. These considerations indicate that ROS generated on the RBC membrane are well situated to escape cytosolic antioxidants and to diffuse of the RBCs.
To test this hypothesis, we carried out lung perfusion experiments with cyanate-reacted RBCs. Cyanate diffuses into the red cell and reacts with the terminal α-amino groups on Hb.21 This reaction is known to inhibit the binding of Hb to the membrane.23 Consistent with our expectation, we show here that perfusion with cyanate-reacted RBCs blocked hypoxia-induced increases in both heme degradation and endothelial DCF fluorescence. These results are attributable to decrease in the H2O2 that is not neutralized by cytosolic antioxidants in the cyanate-reacted RBC, hence resulting in decreased diffusion of H2O2 from RBCs to microvessels.
From these findings, we conclude that during hypoxia increased autoxidation of membrane-bound Hb increases the production of RBC-derived H2O2 on the RBC membrane. This H2O2 escaped the RBC antioxidant system and diffused to the adjoining endothelium.
Interpreting rates of NO consumption by RBC, Aslan et al concluded that ROS release from RBC is minimal in hypoxia.35,36 However, NO consumption data might not directly represent superoxide production because NO passes through the RBC membrane and rapidly reacts with both oxyHb or deoxyHb. This effect accounts for the bulk of the NO consumption by RBC and could explain why Aslan et al35,36 did not see different NO consumption rates in normoxia and hypoxia. However, we agree with these authors that, under normoxic conditions, ROS release is minimal from RBCs. In our studies, transfer of ROS from RBCs to capillaries was undetectable under normoxic conditions. It is only when RBC ROS production was increased in hypoxia that the ROS transferred from RBCs to microvascular endothelium. Consistent with the increase in ROS production by sickle cell RBC reported by Aslan et al,36 we detected increased ROS transfer when we used BERK-trait mice that express human sickle cell Hb.
The hypoxia-induced ROS released from RBC increased endothelial Ca2+cyt in lung microvessels (Figure 3). Similar to DCF fluorescence, the Ca2+cyt effect was hematocrit dependent and was also blocked by catalase. Because Ca2+-free infusion abrogated the Ca2+cyt, but not the DCF response, we interpret that RBC-derived H2O2 activated external Ca2+ entry, causing the Ca2+cyt increase. These findings are the first evidence that, in hypoxia, endothelial Ca2+cyt increases secondary to a paracrine effect of RBCs on microvessels.
In the presence of RBCs, hypoxia also induced lung microvascular leukocyte recruitment. The leukocyte recruitment was abrogated in the absence of RBCs, as also under conditions that abrogated the increase of endothelial DCF fluorescence, namely, perfusion with nitrite-, or CO-treated RBCs, or addition of catalase to RBC-containing perfusion. The leukocyte recruitment was also abrogated in the presence of a P-selectin blocking mAb. Consistent with previous reports attesting to the ability of exogenous H2O2 to mobilize endothelial P-selectin,37,38 our findings indicate that the leukocyte recruitment resulted from RBC-derived H2O2 and that it was endothelial P-selectin dependent.
Studies by Wood et al also support this mechanism.39 These authors reported that, in conscious rats, hypoxia increased leukocyte adherence in the mesenteric circulation in a ROS-dependent manner. Although other possible sources for these ROS need to be considered, we suggest that, in the experiments of Wood et al,39 the hypoxia-induced ROS were RBC derived and the ROS caused leukocyte responses by present mechanisms. Because leukocyte accumulation in microvessels signifies the onset of the inflammatory response, our present findings are the first direct evidence that hypoxia induces a proinflammatory response in the lung.
It is important to consider that artifactual hemolysis in the blood-perfused lung could cause endothelial ROS increases in hypoxia. In the absence of superoxide dismutase or catalase, free Hb could generate hydroxyl radicals or superoxide anions by autoxidation or the Fenton reaction. To eliminate these possibilities, we incorporated a critical modification of our perfused lung model. Thus, we filled a reservoir with hemolysis-free, freshly isolated and HEPES buffer resuspended RBCs. These RBCs were then directly infused into the imaged microvessels through a venous microcatheter. The critical point of our technical modification is that, in our system, the experimental RBCs did not recirculate because they passed through the blood vessel just once. Therefore, they were not exposed to the hemolysis-inducing effects of the lung perfusion circuit. Our failure to detect free Hb in samples of RBC collected from the microcatheter effluent indicates that hemolysis was most definitely not present in our experimental field and therefore could not have affected our findings.
Another potential consideration is that, during hypoxia, RBC-endothelial interactions could induce an endothelial Ca2+ influx, thereby activating endothelial nicotinamide adenine dinucleotide phosphate oxidase and ROS production. However, CO- and nitrite-treated RBCs failed to induce endothelial ROS increases. Further, increasing hematocrit from 10% to 50% did not increase the hypoxia-induced augmentation of endothelial DCF fluorescence. Therefore, these fluorescence responses were probably not determined by blood viscosity. Moreover, RBC velocity in capillaries did not differ between normoxic and hypoxic conditions. These findings, together with the catalase inhibition data discussed earlier, rule out the presence endothelial mechanisms secondary to RBC-endothelial interactions or shear dependent effects.
The role of blood cells other than RBCs in the hypoxia-induced endothelial ROS response is unlikely because the response was induced in microvessels perfused with RBC alone. Moreover, the infusion of isolated leukocytes and platelets did not affect the ROS-induced endothelial Ca2+cyt increase. We also show that there was no difference in the endothelial Ca2+cyt response in microvessels perfused with whole blood or RBCs alone, thereby ruling out potential antioxidants in plasma as modifiers of the RBC-induced endothelial response to hypoxia.
Our findings might be relevant to clinical conditions in which hypoxia decreases O2 tension in the systemic venous return, thereby augmenting preexisting lung inflammation. Therefore, although hypoxia might not be solely adequate to increase leukocyte counts in the bronchoalveolar lavage, to the extent that leukocytes were recruited to the lung vasculature our findings indicate that RBC-dependent mechanisms are sufficient to set up a proinflammatory response in hypoxia. The extent to which secondary stimuli augment this response to cause lung disease requires further consideration.
An Inside Blood analysis of this article appears at the front of this issue.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
This work was supported by NIH grants HL57556 and HL69514 (J.B.), and in part by the intramural research program of the National Institute on Aging of the NIH.
National Institutes of Health
Authorship
Contribution: R.K. obtained the lung data; E.N. obtained the heme degradation data; J.M.R. supervised the RBC studies; J.B. supervised the overall project; R.K., J.M.R., and J.B. prepared the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Jahar Bhattacharya, 630 West 168th Street, BB 8-812, New York, NY 10032; e-mail: jb39@columbia.edu.


![Figure 2. Heme degradation products in rat RBCs. Fluorescence of heme degradation products is shown for Hb incubated (12 hours, 37°C) at pO2 of 100 (normoxic) or 21 (hypoxic) mmHg (n = 4; A), Hb of RBC perfused through lungs inflated under normoxic and hypoxic conditions (n = 4; B), and Hb of nontreated and azide- (C) or cyanate- (D) treated RBCs. The endothelial DCF response is also shown for cyanate-treated RBCs (E) and perfused through lungs inflated under normoxic and hypoxic conditions (n = 3). Data are mean plus or minus SE (#P < .05 vs baseline [panels A,B, 1st bar]; *P < .05 vs hypoxic RBC [panel C, 1st bar]; **P < .05 vs hypoxic RBC [panel E, 1st bar]).](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/111/10/10.1182_blood-2007-09-113902/6/m_zh80080818370002.jpeg?Expires=1763768842&Signature=IUKGf~taBlU6tvs8htFRA~1IkJnwxVs-DlPCK2YNtPTYHCLfcgYzlWt8Puzaw8lHd~uIO-OX-A76Zjc61CUH3h7JfBwbadg7alDtabuSahCVIH8nETrNRp3Po7fgetGtX4r-fJ1Hh0NXqasuVGb1764qjX-RyZAnUnyeMOybDQzZUWhfsmERFVELGehJrksGv0c7RG-D8mJjeqvxb6KsKPVkdOBUA67E1CYRKEP8NTYTT9niTM4~wXoJd-5T2CHBP6RXFnEeOuh722XtdKzwFyd1t37Z5d6d2N0dbGi8auIgLl3fpd86we9z8a71nfBIGUydYIjQI7HY3yH9XRl-bw__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)


![Figure 2. Heme degradation products in rat RBCs. Fluorescence of heme degradation products is shown for Hb incubated (12 hours, 37°C) at pO2 of 100 (normoxic) or 21 (hypoxic) mmHg (n = 4; A), Hb of RBC perfused through lungs inflated under normoxic and hypoxic conditions (n = 4; B), and Hb of nontreated and azide- (C) or cyanate- (D) treated RBCs. The endothelial DCF response is also shown for cyanate-treated RBCs (E) and perfused through lungs inflated under normoxic and hypoxic conditions (n = 3). Data are mean plus or minus SE (#P < .05 vs baseline [panels A,B, 1st bar]; *P < .05 vs hypoxic RBC [panel C, 1st bar]; **P < .05 vs hypoxic RBC [panel E, 1st bar]).](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/111/10/10.1182_blood-2007-09-113902/6/m_zh80080818370002.jpeg?Expires=1763768843&Signature=PA4cl2A-~AD8WaFgUjdWKp0nNl6WfJLk1K1QCFOZwscQ9FqPTwnZ0kNfTPWg9MAgFAeYbwWOGeIvNn2gVSmgzDHHpQ-a8eV1qWz4g3q6a663IRHZFcKh7DdL73LRP7CXQz0v1wvCZUL3hbVA2jXzpm9H5rCNw7TGBN~wrPdam8s3ZkaJaq7hViUclINHw~eecbs4-VXB4jR53LUHi2OoBFzfAPAUaMf2Hj4nstH6jSXWT1VaaF5SXeey1SgS5cHr4SpPFVmxJnDfRvFDhfp~vUXHZtetvt9KuLUG8RSNhI7kLW7QuDjKA1hd648p5ty0RdsKE~eOb--qGvHggxgKnA__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)