In this issue of Blood, Syrjala and coworkers highlight that sexual recovery in long-term survivors after allogeneic stem-cell transplantation may well be the most frequent late effect ever reported.
The number of long-term survivors of hematopoietic cell transplantation (HCT) is increasing rapidly; worldwide, more than 45 000 patients receive HCT each year. Patients with leukemias who survive without recurrent malignancy for 2 years after allogeneic HCT currently have an 89% probability of surviving for 5 or more years. Research on late effects has increased, and systematic information on routine monitoring and management of health care needs is available to guide oncologists or primary care physicians. Much of the research on HCT survivors has focused on major medical events rather than daily health issues and symptoms. Late deaths, second cancers, and employment have been evaluated in large cohort studies.1-3 Several uncontrolled cross-sectional cohort studies have documented generally good quality of life among adults who survive 5 to 20 years after HCT.1-3
Sexual dysfunction is widely noted in studies of quality of life following systemic cancer treatment, particularly following the use of alkylating agents in HCT. But few studies have examined the nature of this dysfunction or followed survivors over time to determine whether function improves, stabilizes, or declines with continued recovery. Although sexual problems also occur in a large percentage of the healthy population, particularly among women, sexual function in cancer survivors after HCT has rarely been compared with that of case-matched controls.
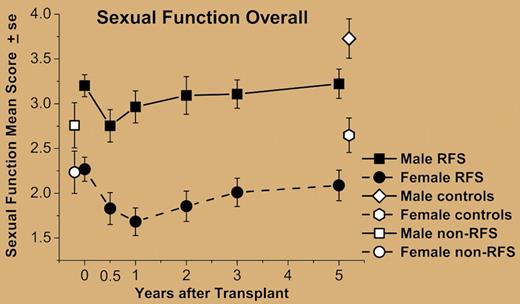
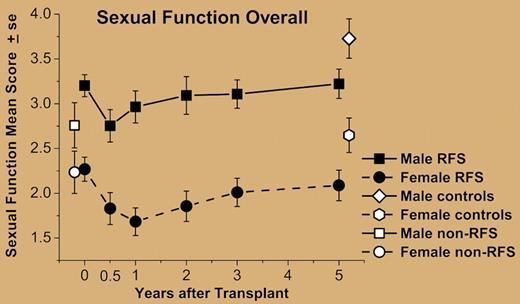
In this issue of Blood, the Seattle group reports on a major study on sexuality following HCT. In a previous case-control cohort, they already reported that 10-year survivors had more sexual problems than control individuals had.4 Syrjala and colleagues now provide the results of a prospective evaluation of sexual function in myeloablative HCT survivors through 5 years after treatment. They identified the trajectory of recovery from the hypothesized 6-month nadir of function after HCT, as well as comparing survivors' 5-year sexual function and residual sexual problems to those of case-matched controls. Adults completed measures before HCT (n = 161), with survivors followed at 6 months and 1, 2, 3, and 5 years. At 5 years, case-matched controls also completed assessments. Analyses indicated that men and women differed both in rates of being sexually active across time and in overall sexual function. Both sexes declined in sexual activity rates and sexual function from pre-HCT to 6 months (see figure). Although sexual activity recovered by 1 year in nearly two-thirds of male patients, only half of women recovered by 2 years. Men improved from their 6-month nadir in sexual function by 2 years, whereas women did not improve by 5 years. Both male and female survivors were below controls in rates of sexual activity and sexual function at 5 years. Most women reported sexual problems (80% of survivors vs 61% of controls); in contrast, 46% of male survivors (vs 21% of male controls) reported problems. Thus, despite some recovery, sexual dysfunction remained a major problem for men and women after HCT.
Sexual function in male and female relapse-free survivors (RFS) from before transplant (n = 109) to 5 years after transplant (n = 80; Figure 3 of Syrjala et al). Both males and females declined in average sexual function from pretransplant to 6 months. Females did not improve from 6-month posttransplant levels by 5 years and remained below matched controls. Males improved by 2 years, but remained below their respective controls at 5 years.
Sexual function in male and female relapse-free survivors (RFS) from before transplant (n = 109) to 5 years after transplant (n = 80; Figure 3 of Syrjala et al). Both males and females declined in average sexual function from pretransplant to 6 months. Females did not improve from 6-month posttransplant levels by 5 years and remained below matched controls. Males improved by 2 years, but remained below their respective controls at 5 years.
This study shows that sexual dysfunction is one of the most frequent late complications occurring after HCT, and the authors are to be congratulated for doing such an outstanding analysis. I would, however, stress 2 points: first, although the authors focused on hormonal levels and somatic parameters, neither of these 2 items can capture the complexity of human sexuality and satisfaction. Second, it would be of great interest to see the trajectory of recovery of sexual function in similar patients who did not undergo HCT.
Conflict-of-interest disclosure: The author declares no competing financial interests. ■