Abstract
Background and aims. In CLL, TL has been associated to outcome. However a larger patient sample and an analysis on a blinded validation series are required to fully establish the independent prognostic value of TL and to define its impact on prognostic subgroups defined according to established predictors. These issues have been addressed on a CLL learning cohort and validated on an independent blinded cohort, overall accounting for 401 CLL patients. Also, we have tested TL as a risk factor of Richter’s Syndrome (RS), an extremely severe event that most of the currently available biomarkers fail to predict.
Methods. The learning series (LS) included 191 patients from the university of Torino (UT), while the blinded validation series (BVS) included 210 patients from University of Eastern Piedmont (UEP). TL was assessed on PBMC collected at diagnosis by Southern blotting and no biological or clinical feature of BVS patients was available to the laboratory performing the analysis. Detailed clinical history, clinical parameters at diagnosis as well as VH-mutational status, cytogenetics, CD38 expression and Zap-70 were available for the vast majority of patients and employed together with TL as covariates for multivariate survival analysis.
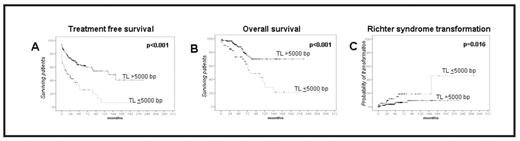
Results. The two series showed no differences for any clinical and biological features except age that was slightly higher in the BVS series. Also TL distribution was similar in the two series (median TL 6024 and 5959 bp respectively). By applying ROC analysis and Youden’s index to the LS we identified a cut-off point of 5000bp segregating 26% (104/401) of patients in the high-risk subgroup. TL was a powerful and independent outcome predictor for both TFS (24.6 vs 73 months p<.001, Fig.1A) and OS (105.5 vs 281 months p<0.001, Fig. 1B). The same cut-off was then applied to the BVS and again TL emerged as strong predictor for TFS (15.2 vs 130.8 months; p<.001) and OS (79.8 vs not reached; p<.001). Multivariate analysis in the BVS selected TL as an independent predictor for both TFS (p=.002) along with peripheral blood lymphocytes (p<.001), CD38 expression (p<.001), beta-2-microglobulin levels (p=.001), and unfavorable FISH karyotype (p=.046), and OS (p.035) (along with age >65 years, p<.001 and advanced Binet stage p=.015). The strict biopsy policy adopted at UEP in case of suspected RS allowed to demonstrate that TL≤5000 acts as an independent predictor also for this event (five-year risk: 18.9% vs 6.4%; p=.016 HR 2,70) (Fig 1C). Finally we analyzed how TL performed in conjunction to established prognostic indicators: TL segregated a CLL group displaying short TFS and OS despite being characterized by Binet A (p<.001), IGHV-homology< 98% (p<.001), CD38<30% (p<.001) and ZAP70<20% (p<.001) and favorable FISH (p<.001). Also, among CLL carrying unfavorable prognosticators, TL<5000 bp identified a CLL subgroup with longer OS despite being characterized by age >65 years (p=.004), Binet stage B-C (p<.001), or unfavorable cytogenetics (p=.001).
Conclusions. These results demonstrate that TL is a powerful independent predictor of multiple outcome events in CLL and contributes to refine the prognostic assessment of CLL when utilized in combination with other prognostic markers. We thus recommend a more widespread use of this biomarker in CLL.
Disclosures: No relevant conflicts of interest to declare.
Author notes
Corresponding author