Abstract
Introduction: Survival gains in follicular lymphoma (FL) have been variably attributed to improved first line and salvage therapies, and a decreasing frequency of histologic transformation (HT). Although ASCT is often used in patients (pts) with transformed lymphoma (TL), optimal pt selection and factors predictive of outcome are unclear. Although immunohistochemistry (IHC) has been applied to prognostication in de novo DLBCL, few studies have investigated IHC as a prognostic factor in TL. The purpose of this analysis was to review outcomes using ASCT for TL at the Cleveland Clinic Taussig Cancer Insitute (CCTCI) in light of modern IHC-based pathologic analysis.
Methods: All pts undergoing ASCT for diffuse large B-cell lymphoma from 2003–2008 at CCTCI (n=130) were identified. IHC analysis for markers CD10, BCL2, BCL6, and MUM-1 was available for 56 pts, who were analyzed further. Pts with TL (n=25) were compared as a group to de novo cases (n=31).
Baseline characteristics were compared using Fisher’s exact and Wilcoxon rank-sum tests. Relapse-free and overall survival (RFS and OS) were estimated with the Kaplan-Meier method and compared via log-rank test. Cox proportional hazards analysis was used to examine features predicting outcome after ASCT.
Results: Median age was 57 years. Of 25 TL pts, 16 had prior FL, 1 each had small lymphocytic lymphoma and nodular LP Hodgkin lymphoma, and 7 presented with coexistent DLBCL and FL in the same biopsy specimen. Among 18 TL pts with metachronous presentation, HT occurred at a median of 26 months (range, 8–198 months).
Pathologic characteristics (%) are:
| Group . | CD10 . | BCL6 . | MUM-1 . | BCL2 . | GCB phenotype* . | MedianKI67 index . | t(14;18) . |
|---|---|---|---|---|---|---|---|
| * Criteria from Hans et al, Blood2004;103(1):275–82 | |||||||
| TL | 84 | 95 | 38 | 84 | 92 | 70 | 8/10 |
| de novo | 61 | 88 | 43 | 63 | 71 | 80 | 1/8 |
| P value | .08 | .62 | 1.0 | .18 | .09 | .63 | .02 |
| Group . | CD10 . | BCL6 . | MUM-1 . | BCL2 . | GCB phenotype* . | MedianKI67 index . | t(14;18) . |
|---|---|---|---|---|---|---|---|
| * Criteria from Hans et al, Blood2004;103(1):275–82 | |||||||
| TL | 84 | 95 | 38 | 84 | 92 | 70 | 8/10 |
| de novo | 61 | 88 | 43 | 63 | 71 | 80 | 1/8 |
| P value | .08 | .62 | 1.0 | .18 | .09 | .63 | .02 |
Age and disease status at time of transplant were similar between groups. Three de novo pts and 2 TL patients underwent ASCT during first remission; all others underwent ASCT for relapsed/refractory disease.
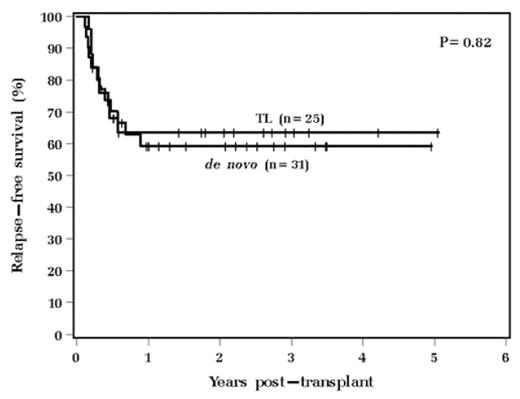
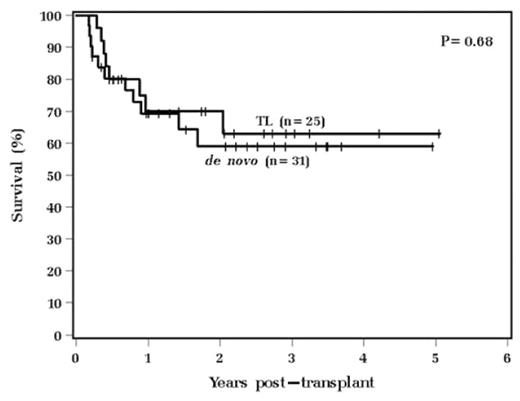
With a median follow-up of 25 months, 4 year RFS was 64% vs. 59% (p=.82) and OS 63% vs. 59% (p=.68) for TL and de novo pts, respectively (see Figures 1 and 2).
No IHC feature predicted RFS or OS. Elevated LDH at time of ASCT predicted poor RFS (HR 4.6, p=.008) and OS (HR 6.3, p=.005) on multivariate analysis, and increasing number of prior regimens predicted poor RFS only (HR 1.4, p=.003).
Conclusions: TL resembled de novo DLBCL in terms of IHC characteristics, but a higher proportion of TL cases bore the t(14;18) translocation.
ASCT was effective in treating TL, with a 4-year RFS and OS exceeding 60%. This was indistinguishable from outcomes for de novo DLBCL pts treated with ASCT over the same period. Baseline characteristics were similar between TL and de novo pts.
Survival in FL may be improving in part due to good outcomes using ASCT for TL. Confirmation of our observed RFS/OS among TL pts requires longer follow-up, given the ongoing risk of relapse of indolent disease. Outcome after ASCT cannot be predicted by IHC, and novel approaches are needed to improve pt selection and elucidate the biology of HT.
Disclosures: No relevant conflicts of interest to declare.
Author notes
Corresponding author