Abstract
INTRODUCTION: In 10% of acute myeloid leukemia (AML) patients the recurrent balanced translocation t(8;21) places the RUNX1 (AML1) gene next to RUNX1T1 (ETO) gene resulting in the generation of a RUNX1-RUNX1T1 fusion protein. While in mouse models this protein has failed to produce leukemia alone, alternative splicing of exon 9a of the RUNX1-RUNX1T1 fusion transcript has recently (
HYPOTHESIS: We hypothesized that i) the fusion of RUNX1 to RUNX1T1 alters exon 9a splicing balance, ii) Fusion transcripts containing exon 9a is involved in leukemogenesis in RUNX1-RUNX1T1 positive AML patients, and iii) the ratio between fusion transcripts with and without exon 9a may have prognostic significance.
MATERIALS AND METHODS: Real-time quantitative PCR analysis was performed using primer-probe sets discriminating between the RUNX1-RUNX1T1 fusion transcript as well as the RUNX1T1 transcript containing exon 9a (R+9a) or lacking exon 9a (R-9a), respectively. Twenty-three diagnosis and 117 follow-up samples from 14 RUNX1-RUNX1T1 positive patients and diagnosis samples from 13 RUNX1-RUNX1T1 negative AML patients, as well as from 29 normal donors were included in the study.
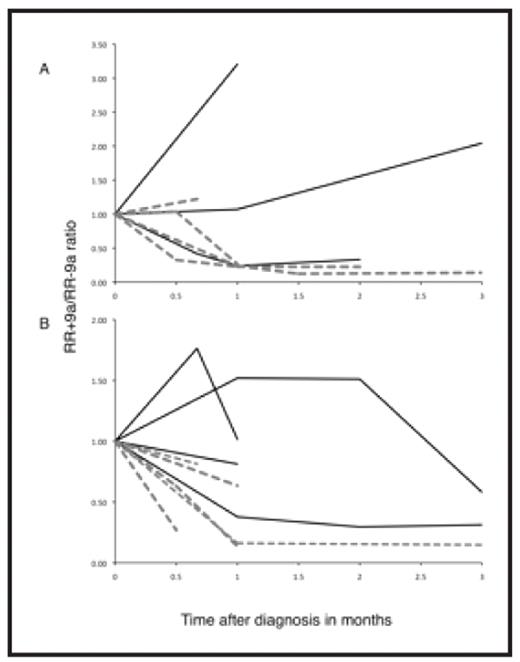
RESULTS: Levels of the native RUNX1T1 mRNAs were expectedly low in both healthy donors and RUNX1-RUNX1T1 negative AML patients, allowing us to define a threshold, above which R+9a and R-9a expression in RUNX1-RUNX1T1+ patients truly reflected RUNX1-RUNX1T1 fusion transcript expression. Thus, median RUNX1-RUNX1T1 expression was a factor 500 higher than the BM threshold and a factor 104 higher than the PB threshold. The ratios between R+9a and R-9a transcripts were within a relatively narrow range in normal donors and RUNX1-RUNX1T1 negative patients (0.017 to 0.11, median 0.06). By contrast, the R+9a/R-9a ratios in RUNX1-RUNX1T1 positive AML patients were significantly higher (range 0.05–0.46, median 0.17), (Wilcoxon’s rank sum test, P<0.001), with 12/14 patients displaying R+9a/R-9a ratios above the normal range in either bone marrow (BM) or peripheral blood (PB). More importantly, patients who achieved a continuous complete remission (CCR) displayed a more rapid disappearance of the RR+9a compared to RR-9a (Wilcoxon’s rank sum test of individual patient slopes BM: P=0.07, PB: P=0.014), further corroborating the notion that deregulated RUNX1-RUNX1T1 splicing is part of leukemogenesis (Figure).
CONCLUSION: Deregulated RUNX1-RUNX1T1 splicing is part of the leukemogenic process in the majority of RUNX1-RUNX1T1 positive AML patients. We suggest that analysis of splice variant kinetics during cytoreduction may, if validated in larger studies, be a useful way to identify patients prone to relapse.
Splice variant kinetics during cytoreductive treatment in BM (A) and PB (B). Black lines: patients with later relapse. Grey broken lines: patients remaining in CCR. X-axis: time after diagnosis, y-axis: RR+9a/RR-9a splice variant ratio relative to ratio at diagnosis.
Disclosures: No relevant conflicts of interest to declare.
Author notes
Corresponding author