Abstract
BACKGROUND: Arthropathy is the most common complication of severe factor VIII deficiency and causes chronic pain, functional disability and increased cost of care. Early institution of primary prophylaxis (PP) was found to prevent hemophilic arthropathy at age 6 years in a prospective randomized clinical trial including 65 boys (
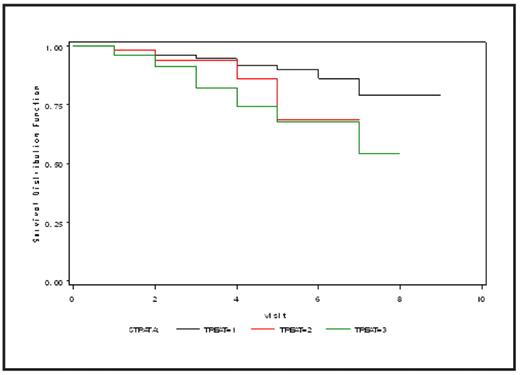
METHODS: Eligibility for this analytic project included boys with factor VIII < 1% entered onto the UDC study at or before 36 months of age. Treatment was clinically determined and defined as prophylactic which could be primary (PP, initiated at or before 36 months), secondary (SP, initiated at or following 42 months), or indeterminate (IP, initiated between 36 and 42 months); or episodic (E, without routine prophylaxis). A target joint was defined as one with four or more bleeding events within 6 months. Kaplan-Meier curves were used to evaluate survival without target joint development over time; Cox modeling was employed to assess risk factors for target joint development. Univariate and multivariable analyses were used to model risk factors for bleeding.
RESULTS: Of 603 eligible boys, treatment included: PP in 252 (42%), SP in 73 (12%), E in 240 (40%). 38 boys (6%) with IP were excluded from the analysis. In comparison to children treated with E, those on PP were, on average: older (2.17 vs 1.87 years, p < 0.0001); more likely to have had a bleeding event (96 vs 91%, p=0.002); more likely to have received home infusions (90 vs 49%, p < 0.0001); and more likely to have suffered an intracranial hemorrhage (11.3 vs 4.1%, p=0.02). Despite their increased experience with joint and other bleeding events, during the period of prospective observation, children on PP had significantly less joint bleeding (OR 0.51, CI 0.39–0.66, p < 0.0001) and showed improved survival time without onset of a target joint (p = 0.002 overall, and 0.004 between PP and E, figure 1). Results for muscle or any bleeding were similar. In multivariable analysis PP exerted the greatest protective effect on risk of target joint development (hazard ratio 0.38, 95% CI 0.22–0.66, P = 0.001). Factors associated with E therapy included non-white race (p < 0.0001) and insurance coverage other than commercial (p = 0.004), although these factors were not associated with poor joint outcomes.
CONCLUSION: In a large population of children with severe hemophilia A on the CDC UDC registry, PP prevents joint and other bleeding and delays target joint development. Factors limiting application of PP must be explored and addressed.
Disclosures: No relevant conflicts of interest to declare.
Author notes
Corresponding author