Abstract
Background: The prognostic significance of lymphocyte counts and immune status has been carefully examined in lymphoid malignancies, but the importance of the lymphocyte count in chronic myeloid neoplasms is less clear. In a recent analysis of MDS cases associated with deletion of chromosome 5q (Holtan SG et al AmJHem 2008 Epub 12Jun), we observed that an ALC >1.2 × 109 cells/L at diagnosis is independently associated with improved survival. The prognostic value of ALC in MDS not associated with del(5q) is unknown.
Methods: We reviewed the medical records of patients without del(5q) diagnosed with MDS at our institution over a 10-year period and gathered data on complete blood counts and leukocyte differentials, bone marrow findings, and clinical course. Inclusion criteria included diagnosis within 6 months prior to initial consultation at our institution and <20% marrow blasts. Patients were classified according to the International Prognostic Scoring System (IPSS) and the WHO-classification based Prognostic Scoring System (WPSS).
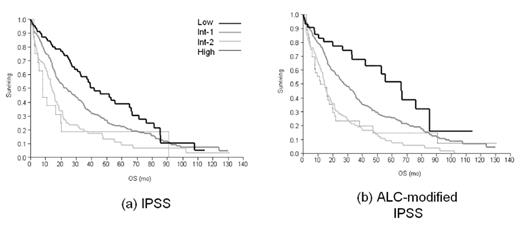
Results: The median age of the 503 included patients (360 M, 143 F) was 69 years (range 20–91). Median follow-up was 14 months, and 65% of patients were known to have died with an overall median survival of 36 months. Cytogenetic results as classified by the IPSS were favorable in 326 (65%) patients, intermediate in 112 (22%), and poor in 65 (13%). Both IPSS and WPSS accurately stratified patients, but the WPSS was better at identifying the lowest and highest risk patients. Survival by IPSS risk group was as follows: low-risk disease (n=95, median survival 41.8 months), intermediate-1 (n=285, 23.6 months), 106 with intermediate-2 (n=106, 14.1 months), and high-risk (n=17, 8.05 months). WPSS risk groups included very low risk (n=87; median survival 71.9 months), low risk (n=149, 28.8 months), intermediate risk (n=85, 19.3 months), high risk (n=143, 14.4 months), and very high risk (n=39, 8.8 months). In univariate analysis, factors associated with poorer survival included advanced age (p = 0.0012), higher-risk WHO subtype (p<0.0001), increased marrow blast percentage (p<0.0001), poor-risk karyotype (p<0.0001), higher IPSS score or WPSS score (p<0.0001), lower hemoglobin (p<0.0001), lower MCV (p=0.03), lower ALC (p=0.001), and lower platelets (p=0.001). Factors not associated with survival included sex and ANC. In a multivariate model including only baseline CBC parameters, hemoglobin >10 g/dL (p < 0.001), MCV >96 fl (p = 0.0493), ALC >1.2 × 109/L (p = 0.0449), and platelet count >100 × 109/L (p = 0.0046) were associated with improved survival. A high baseline ALC also maintained independent prognostic significance in a multivariate model against the IPSS (RR 0.746, 95% CI: 0.598, 0.933, p = 0.0099), and the raw WPSS score (RR 0.791, 95% CI 0.633, 0.987, p=0.037) but not the WPSS group (p=0.0794). There was no significant difference in the distribution of IPSS scores between the ALC >1.2 × 109 cells/L and the ALC ≤ 1.2 × 109 cells/L groups, although there were significantly more WPSS high risk patients in the low baseline ALC group (p = 0.0163). The creation of an ALC-modified IPSS score by adding 0.5 point for an ALC ≤ 1.2 × 109 cells/L resulted in a significant increase in median overall survival of the low risk group (41.8 months versus 66.1 months, p < 0.001, Figure 1).
Conclusion: ALC is a novel and easily obtained prognostic marker in MDS that provides information complementary to existing prognostic scoring systems.
Kaplan-Meier curves based upon IPSS (a) and the ALC-modified IPSS (b), where 0.5 point was added for an ALC ≤ 1.2 × 109 cells/L.
Kaplan-Meier curves based upon IPSS (a) and the ALC-modified IPSS (b), where 0.5 point was added for an ALC ≤ 1.2 × 109 cells/L.
Disclosures: No relevant conflicts of interest to declare.
Author notes
Corresponding author