Abstract
Introduction: Primary care physicians are typically the first physicians who see patients with thrombocytopenia. There are currently no data to document which patients who present with isolated thrombocytopenia or immune thrombocytopenic purpura (ITP) are referred to hematologists. The published ASH Practice Guideline on ITP (
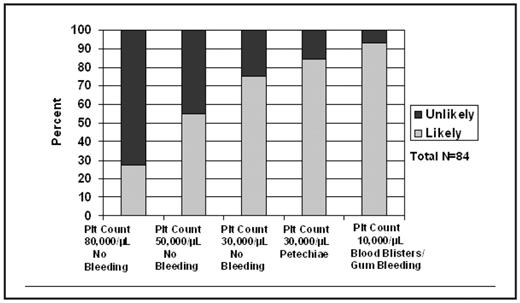
Methods: A survey was conducted in collaboration with the Oklahoma Physicians Resource-Research Network (OKPRN). The mission of the OKPRN is to provide community physicians with access to information and research opportunities to enhance their practices and to generate new knowledge through practice-based research. OKPRN family physicians (N=127) were asked to complete a short eight-item questionnaire consisting of five patient vignettes with varying degrees of thrombocytopenia and bleeding symptoms. For each vignette, the physician was to decide when or if he/she would send the patient to a hematologist for further management using a four point likert scale. The response categories were ‘very unlikely’, ‘unlikely’, ‘likely’, and ‘very likely’. The response scale was dichotomized (unlikely vs likely) to graphically display results across all five patient vignettes.
Results: There was a 66% (84/127) response rate. Fifty-one percent (43/84) of the responders had been practicing family medicine between 6–20 years, 37% (31/84) for more than 20 years, and 12% (10/84) had been practicing between 1–5 years. Sixty-one percent (51/84) responded that there was a hematologist that they routinely called on the phone for advice and/or sent referrals, and 81% (68/84) practiced within 50 miles of a hematologist. Figure 1 shows as a patient’s thrombocytopenia became more severe, the likelihood of referral to a hematologist increased. Seventy-five percent of the respondents surveyed were ‘likely’ to send a patient with moderate thrombocytopenia (platelet count 30,000/μL) without bleeding symptoms to a hematologist. The likelihood of referral increased to 85% when the moderate thrombocytopenia was associated with mild bleeding symptoms, and over 90% when a patient presented with severe thrombocytopenia (platelet count 10,000/μL) and bleeding symptoms.
Based on clinical vignettes, how likely or unlikely is a family practitioner to send a patient to a hematologist for further management?
Based on clinical vignettes, how likely or unlikely is a family practitioner to send a patient to a hematologist for further management?
Conclusion: Results from the OKPRN survey documented that patients with isolated thrombocytopenia and a platelet count of 80,000/μL would infrequently be referred to a hematologist while patients with platelet counts of ≤30,000/μL would almost always be referred, especially if there were bleeding symptoms. Results from this survey validate assumptions that ITP patients with moderate to severe thrombocytopenia are managed by hematologists, not primary care physicians. These data are important to define the scope of practice of hematology.
Disclosures: Terrell:Amgen Inc: Consultancy, Research Funding. George:Amgen Inc: Consultancy, Research Funding.
Author notes
Corresponding author