Abstract
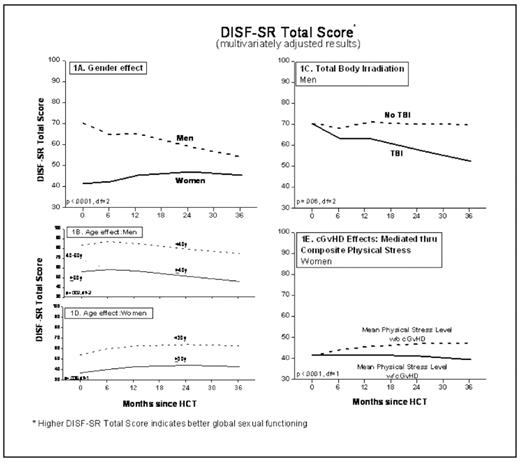
Sexual dysfunction is a multidimensional problem caused by both physiologic and psychosocial factors. Yet little is known about the longitudinal trends of sexual functioning in HCT survivors, or the clinical or psychosocial factors associated with decline. Using a longitudinal study design, we administered the Derogatis Interview for Sexual Functioning (DISF-SR), the Global Sexual Satisfaction Index (GSSI), and the City of Hope-QOL instrument at 5 time points to a large cohort of patients undergoing HCT at City of Hope (COH): prior to HCT, at 6m, 1y-, 2y-, and 3y-post-HCT. DISF-SR assessed 5 domains of sexual functioning (Cognition/Fantasy, Arousal, Behavior/Experiences, Orgasm, and Drive/Relationship), and a Total score. GSSI elicited patients’ subjective appraisal of sexual satisfaction. The COH-QOL instrument was used to obtain self-reported levels of anxiety, distress, depression, pain, physical strength, and sleep changes, which were converted to composite scores of mental and physical stress. Long-term trends of sexual functions were estimated using the Generalized Estimating Equation. We examined the effects of sociodemographic factors, primary diagnosis, HCT conditioning regimens, disease status at HCT, presence of cGvHD, and composite mental and physical stress levels on the longitudinal trends of DISF-SR, the Total score, and GSSI. The cohort included 312 adults (median age at HCT 48y; 56% males) undergoing autologous (n=175) or allogeneic (n=137) HCT for hematologic malignancies or severe aplastic anemia; 144 patients completed the 3y sexual survey (participation rate at 3 years=75%). GSSI (general sexual satisfaction) declined significantly after HCT (p=0.001) for both men and women, and remained depressed over the 3-y study period, with 40% reporting poor or worse sexual satisfaction level at 3y. There were no significant differences between men and women in terms of general sexual satisfaction level. However, the degree of sexual dysfunction as measured by DISF-SR was worse in women than in men for all domains, and for Total score (p<.001) at all post-HCT time points (Fig. 1A). Furthermore, assessment of DISF-SR scores revealed that while men experienced a persistent decline in satisfaction with Orgasm and Drive/Relationship (p<0.05), women did not demonstrate a significant decline in sexual function in any of the domains post-HCT. Gender-specific multivariate analyses revealed certain subgroups that were more vulnerable to a decline in sexual functions after HCT. Notably, older age (≥40y) (Fig. 1B), being married, and TBI exposure in men (Fig. 1C), and older age (≥30y) (Fig. 1D), being overweight, and greater mental and/or physical stress in women were factors identified as significantly associated with decreased sexual functioning following HCT. Although cGvHD was not directly related to DISF-SR or GSSI, presence of cGvHD was accompanied by worse mental and physical composite scores (p<0.0001). Lower mental and/or physical composite scores in turn were significantly related to lower sexual functions for all domains of DISF-SR, the Total score (Fig. 1E) and GSSI in women (p<0.05). Thus, women may be vulnerable to the effects of cGvHD mediated through mental and/or physical stress, in turn resulting in compromised sexual functions and satisfaction after HCT. This study should inform healthcare providers that patients undergoing HCT require more attention to their sexual QOL within the first year after HCT. Routine inquiry of patients’ sexual health should be included in follow-up exams after HCT, especially for those at high risk (i.e. TBI-exposed men and those with cGvHD), with the ability to offer a multidisciplinary approach to managing this distressing complication.
Disclosures: No relevant conflicts of interest to declare.
Author notes
Corresponding author