Abstract
Vitamin K antagonists (VKA) are widely used in the treatment and primary and secondary prevention of thromboembolism. Although these drugs have shown to be effective, the associated risk of bleeding is an important limitation. We hypothesized that minor bleeding could be associated with the risk of major bleeding. Even early minor bleeding, i.e. within the first 30 days of VKA therapy, could be an indicator for an increased risk of major bleeding. On the other hand, early minor bleeding could lead to intensified monitoring of VKA therapy and consequently improved quality of anticoagulation, thereby modifying the risk of major bleeding.
To evaluate the supposed association between minor and major bleeding in patients on VKA, a cohort of 6758 consecutive patients in whom VKA therapy was controlled by a Dutch anticoagulant clinic was retrospectively studied. Differences in risk of major bleeding between patients without early minor bleeding and patients with early minor bleeding were evaluated by multivariable Cox proportional hazard regression analysis, also taking into consideration differences in individual time within target range of anticoagulation (ITTR).
Overall, 19.9% of the patients (N=1348) had a minor bleeding, corresponding with an incidence rate (IR, expressed per 100 person-years) of 25.1 (95%CI, 23.8 to 26.5). In 4.4% of the patients (N=300), minor bleeding had occurred within the first 30 days of VKA therapy. Major bleeding had occurred in 1.8% of the patients (N=119); IR=1.8 (95%CI, 2.9 to 3.8).
The risk of a major bleeding was significantly higher in patients with early minor bleeding (IR=4.8; 95%CI, 2.6 to 8.3), compared to patients without early minor bleeding (IR=1.7; 95%CI, 1.4 to 2.0); hazard ratio=2.4 (95%CI, 1.4 to 4.4; P=0.003).
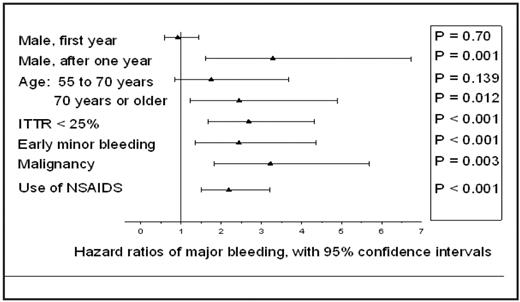
Taking the achieved level of anticoagulation into consideration, major bleeding occurred significantly more frequently in patients with a poor response to VKA, defined as individual time within target range (ITTR) of less than 25% of the total treatment time (lowest quintile of patients); hazard ratio=2.7 (95%CI, 1.7 to 4.3; P<0.001). Figure 1 shows the adjusted hazard ratios for all risk indicators that were independently associated with major bleeding. In addition to early minor bleeding and ITTR < 25%, age, gender, malignancy and the use of NSAIDs were also associated with major bleeding.
As already indicated by the increased risk of major bleeding in patients with early minor bleeding, as well as in patients with a poor response to VKA, a risk modification after early minor bleeding due to intensified monitoring of VKA therapy, resulting in improved quality of anticoagulation is not plausible. In fact, ITTR in patients with an early minor bleeding was 40% versus 42% in patients without early minor bleeding (p=0.07). Furthermore, INR in patients with an early minor bleeding were more frequently above 5.0 (9%) than in patients without early minor bleeding (7%; p< 0.01).
Our findings confirm the hypothesis of early minor bleeding as independent risk indicator and contradicts the assumption of a risk modifying effect. In fact, reduced ITTR and early minor bleeding were both strong independent risk indicators for major bleeding.
Adjusted hazard ratios of major bleeding from multivariable Cox proportional hazards regression analysis.
Adjusted hazard ratios of major bleeding from multivariable Cox proportional hazards regression analysis.
Disclosures: No relevant conflicts of interest to declare.
Author notes
Corresponding author