Abstract
In contrast to previous notions of the help-independency of memory CD8 T cells during secondary expansion, here we show that CD4 help is indispensable for the re-expansion of once-helped memory CD8 T cells, using a hematopoietic cell–specific dominant minor histocompatibility (H) antigen, H60, as a model antigen. H60-specific memory CD8 T cells generated during a helped primary response vigorously expanded only when rechallenged under helped conditions. The help requirement for an optimal secondary response was confirmed by a reduction in peak size by CD4 depletion, and was reproduced after skin transplantation. Helpless conditions or noncognate separate help during the secondary response resulted in a significant reduction in the peak size and different response kinetics. Providing CD4 help again during a tertiary challenge restored robust memory expansion; however, the repeated deprivation of help further reduced clonal expansion. Adoptively transferred memory CD8 T cells did not proliferate in CD40L−/− hosts. In the CD40−/− hosts, marginal memory expansion was detected after priming with male H60 cells but was completely abolished by priming with peptide-loaded CD40−/− cells, suggesting the essential role of CD40 and CD40L in memory responses. These results provide insight into the control of minor H antigen-specific CD8 T-cell responses, to maximize the graft-versus-leukemia response.
Introduction
Minor histocompatibility (H) antigens are naturally processed peptide fragments derived from proteins with polymorphisms that generate differential major histocompatibility complex (MHC)–presenting epitopes.1 They are recognized as foreign during allotransplantation between MHC-matched subjects, resulting in the induction of specific CD4 and CD8 T-cell responses that can lead to life-threatening graft-versus-host disease (GVHD); however, they have also been found to exert a graft-versus-leukemia (GVL) effect.2 Therefore, characterization of the immune response to minor H antigens with specific expression on hematopoietic lineage cells is necessary to apply the minor H antigen–specific T-cell response most productively toward eradicating malignant leukemic cells while suppressing GVHD.
Allo-reactive CD8 T cells are major effectors of rejection after allogeneic transplantation. The CD8 T-cell response to antigen exposure generally involves an initial expansion phase followed by a contraction phase and a memory phase.3-5 During this process, help conferred by CD4 T cells is essential for generating the CD8 T-cell response to noninflammatory Th-dependent antigens, such as minor H antigens, although the timing and mechanism of delivery of this help to CD8 T cells is controversial. CD40 and CD40L are believed to be major mediators of CD4 help. Signaling through CD40 via an interaction with CD40L expressed on activated CD4 T cells activates antigen-presenting cells (APCs), which subsequently increases their antigen presentation and costimulatory capacity, priming CD8 T cells directly.6-9
In contrast to noninflammatory antigen stimuli, infection with a pathogenic organism gives rise to Th-independent CD8 T cells primed via direct APC activation through pattern recognition receptor signaling.8,10 However, even then, the memory CD8 T cells generated in the absence of CD4 help may show impaired secondary expansion after antigen re-encounter.11-13 Thus, CD4 help is required for the generation of proliferation-competent memory CD8 T cells, regardless of the CD4 help–dependent or –independent nature of their specific antigens. However, the consensus obtained through many studies is that CD4 help is dispensable when memory CD8 T cells, generated under CD4 help–sufficient conditions, mount a recall response.12,14,15
Previous investigations of the need for CD4 help in CD8 memory cell expansion and function have relied primarily on infection and/or adoptive transfer of T-cell receptor (TCR) transgenic models. In this study, we used H60, a naturally occurring hematopoietic cell–specific minor H antigen,16 to investigate whether memory CD8 T cells specific for a Th-dependent antigen function without CD4 help upon the induction of secondary expansion. H60 induces an exceptionally dominant CD8 T-cell response in a B6 anti-BALB.B setting to the extent that the response competes well with allo-MHC responses in haplo-identical transplantation.4,17 However, its substantial immunodominance is CD4 help dependent: it was shown to be subordinate to the others without cognate CD4 help.17 This result prompted us to characterize the CD8 T-cell response to H60 as a single antigen, in the absence of complex antigenic competition. Previously, we found that an H60-specific primary CD8 T-cell response was not mounted in CD40- or CD40L-deficient mice, whereas supplementation with normal CD4 T cells in CD40L-deficient mice restored the responsiveness, suggesting a requirement for CD40/CD40L-mediated CD4 help in the induction of an H60-specific response.18 In this study, we focused on the effects of the presence or absence of CD4 help on the development of an H60-specific memory response. Our results illustrate the essential role of cognate CD4 help during this memory response. The results also show that both CD40 and CD40L are required for the expansion of H60-specific CD8 memory T cells but that the role of CD40 expressed by CD8 memory T cells is insignificant.
Methods
Mice
C57BL/6 (B6), C.B10-H2b/LiMcdJ (BALB.B), B6.SJL-PtprcaPep3b/BoyJ (Ly5.1), B6.129P2-Tnfrsf5tm1Kik/J (CD40-deficient), and B6.129S2-Tnfsf5tm1Imx/J (CD40L-deficient) mice were purchased from The Jackson Laboratory (Bar Harbor, ME). The congenic mouse strain, B6.C-H60c/DCR, was a kind gift from Dr Derry Roopenian (The Jackson Laboratory). The mice were maintained under specific pathogen-free conditions at the Center for Animal Resource Development of Seoul National University College of Medicine and were used for experiments at ages between 6 and 12 weeks. Animal experimental procedures were approved by IACUC (Institutional Animal Care and Use Committee) of Seoul National University, Korea.
Immunization and adoptive transfer
A splenocytes suspension was prepared from the stimulator mice and 2 × 107 cells were injected intraperitoneally into each responder mouse. To prepare peptide-loaded cells, the peptides were incubated with the splenocytes at a 1 μM concentration. The peptides loaded onto the splenocytes were LTFNYRNL (H60) and GLNGPDIYKGVYQFKSVEFD (Gp61). CD8 T cells from Ly5.1 congenic mice immunized with male H60 splenocytes (H60 cells) more than 30 days before were purified by MACS according to the manufacturer's instructions (Miltenyi Biotec, Auburn, CA). The purity of the CD8 T cells was confirmed by flow cytometry, and, when the purity was above 90%, the cells were transferred to adoptive hosts (3 × 106 cells/mouse).
Antibodies and flow cytometry
Fresh peripheral blood lymphocytes (PBLs) from the immunized mice were incubated at 4°C for 30 minutes in staining buffer (1×PBS containing 0.1% bovine serum albumin and 0.1% sodium azide) containing phycoerythrin (PE)–labeled H60-peptide (LTFNYRNL)/H-2Kb tetramer (H60-tetramer) and other fluorescence-labeled antibodies. The stained cells were analyzed using a FACSCalibur equipped with CellQuest software (BD Pharmingen, San Diego, CA). The H60-tetramer was obtained as described previously.4 The antibodies used for flow cytometry are as follows: anti-CD11a mAb (M17/4; eBioscience, San Diego, CA), anti-mCD4 mAb (RM4-5; eBioscience), anti-mCD8 mAb (53-6.7; eBioscience), anti-CD45.1 mAb (A20; eBioscience), and anti–IFN-γ mAb (XMG1.2: eBioscience).
Mixed lymphocyte culture
Splenocytes (2 × 107) from immunized mice were cultured with 3 × 107 irradiated male H60 congenic splenocytes in 10 mL culture media (Dulbecco modified Eagle medium [DMEM] containing 5% FBS [Hyclone, South Logan, UT], and β2-mercaptoethanol [Sigma-Aldrich, St Louis, MO]) for 7 days in the presence of 50 U/mL IL-2. CD8 effector cells from the mixed lymphocyte culture (MLC) were tested for cytotoxicity and IFN-γ secretion.
Cytotoxicity assay and IFN-γ secretion analysis
The modified 51Cr release and the IFN-γ secretion assays are described elsewhere.4 Splenocytes from immunized mice were used instead of MLC cells when ex vivo IFN-γ secretion assays were performed. For peptide loading, 51Cr-labeled T2-Kb cells were incubated with 1 μM synthetic peptides for 30 minutes at 37°C and then washed twice with phosphate-buffered saline (PBS). The synthetic peptide for VSV was RGYVYQGL. CD8 effector cells from the MLC were stimulated in the presence of CD8-depleted B6 splenocytes and relevant peptides (1 μM) for 4 hours.
Antibody treatment for CD4 depletion and blockade of the CD40-CD40L interaction
Mice were injected intraperitoneally with ascites of anti–mouse CD4 Ab (GK1.5) at 1 and 3 days before immunization. Purified CD154 (CD40L)–blocking antibody (MR-1; Bio Express, West Lebanon, NH) was injected intraperitoneally into the mice (0.5 mg/mouse) at the time of immunization with male H60 cells and 2 more times at 3-day intervals.
Skin graft
Full thickness body skin grafts (∼1 cm2) from male or female H60 congenic mice (H60-skin) were transplanted onto the shaved backs of recipient mice. The left half of each recipient's back was grafted with skin from either female or male H60 congenic mice (H60-skin) and the right half was grafted with skin from female B6 mice as a syngeneic control. The skin graft was secured with an adhesive bandage for the first 7 days. Graft survival was monitored daily by visual inspection, and PBLs from the grafted mice were stained weekly with H60-tetramer.
Statistical analysis
Statistical calculations and t tests were performed using GraphPad Prism program version 4 (GraphPad Software, San Diego, CA).
Results
The primary H60-specific CD8 T-cell response is CD4 help dependent
Splenocytes from male H60 congenic mice could be used as a source of Y chromosome–derived H-2b–restricted CD8 and CD4 epitopes (HY-Uty/H-2Db and HY-Dby/H-2Ab, respectively), in addition to the congenic H60 locus–derived H-2b–restricted CD8 T-cell epitope (H60/H-2Kb). Therefore, the immunization of female B6 mice with male or female H60 cells was suggested to be a convenient means to control the provision of CD4 help under normal conditions. We confirmed the Th dependency of the H60-specific response by priming female B6 mice with male (helped) or female (helpless) H60 cells and then monitoring the expansion of H60-specific CD8 T cells in the immunized mice. When we measured the frequency of H60-specific CD8 T cells by staining PBLs from the immunized mice with H60-tetramer, a minimal percentage of H60-tetramer–binding (H60-tetramer+) CD8 T cells was detected in the mice that were immunized under helpless conditions over the entire primary response period (∼1% of CD8 T cells, at most, on day 10 after immunization). However, H60-tetramer+ CD8 T cells were clearly detected in the blood of the mice immunized under helped conditions; the maximum frequency of H60-tetramer+ cells ranged from 7% to 15% of CD8 T cells on day 10 after immunization, demonstrating the help dependency of the H60-specific primary CD8 T-cell response. The frequency subsequently dropped to a maintenance level (0.8%-2% of the CD8 T cells) during the resting stage, beginning 28 days after immunization (Figure 1A). Meanwhile, HY-Uty tetramer+ CD8 T cells were detected at negligible levels throughout the primary response period, confirming the dominance of the H60-specific CD8 T-cell response over that specific for HY-Uty (data not shown).
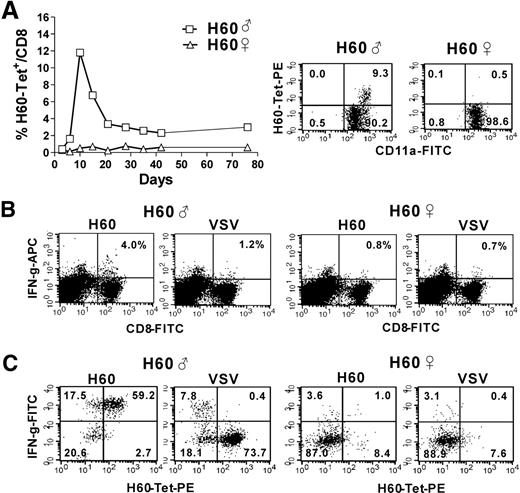
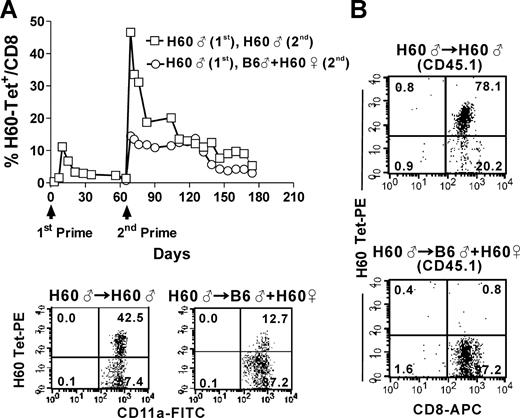
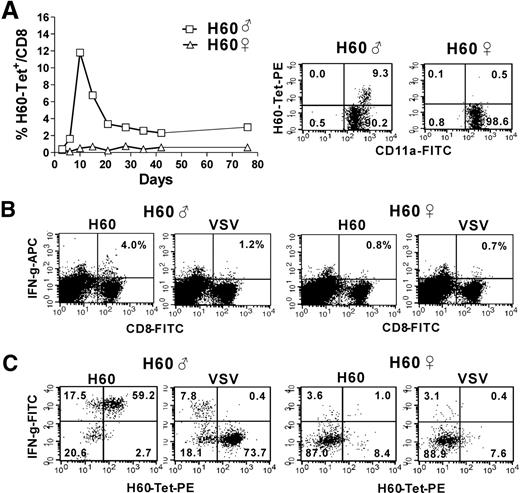
Primary H60-specific CD8 T cell response in the presence or absence of CD4 help. (A) Female B6 mice were immunized with male or female H60 cells and pooled PBLs from the immunized mice (12 mice per group) were stained with H60-tetramer-PE, anti–CD8-APC, and anti–CD11a-FITC. The proportion of H60-tetramer+ CD11a+ cells among the CD8+ cells is plotted. Representative flow cytometric data (gated for CD8+ cells) showing the peak primary response (day 10 after immunization) from more than 10 independent experiments are shown. (B) Splenocytes from mice immunized with male or female H60 cells were prepared on day 10 after immunization and tested ex vivo for IFN-γ production after stimulation with H60-peptide and VSV-peptide (control peptide). The cells were surface-stained with anti–CD8-FITC and anti–CD4-PE, and intracellular staining was performed with APC-conjugated anti–IFN-γ mAb. Representative flow cytometric data from 3 independent experiments are shown. The values in the upper right quadrants indicate IFN-γ–producing cells as a percentage of CD8 T cells. (C) Splenocytes from mice immunized with male or female H60 cells were cultured with irradiated male H60 splenocytes (mixed lymphocyte culture, MLC) for 7 days, and the CD8 effector T cells from each MLC were tested for IFN-γ. The cells were surface stained with H60-tetramer and anti–CD8-APC, and were stained for intracellular IFN-γ with FITC-conjugated mAb. Representative flow cytometric data from 3 independent experiments are shown (gated for CD8+ cells).
Primary H60-specific CD8 T cell response in the presence or absence of CD4 help. (A) Female B6 mice were immunized with male or female H60 cells and pooled PBLs from the immunized mice (12 mice per group) were stained with H60-tetramer-PE, anti–CD8-APC, and anti–CD11a-FITC. The proportion of H60-tetramer+ CD11a+ cells among the CD8+ cells is plotted. Representative flow cytometric data (gated for CD8+ cells) showing the peak primary response (day 10 after immunization) from more than 10 independent experiments are shown. (B) Splenocytes from mice immunized with male or female H60 cells were prepared on day 10 after immunization and tested ex vivo for IFN-γ production after stimulation with H60-peptide and VSV-peptide (control peptide). The cells were surface-stained with anti–CD8-FITC and anti–CD4-PE, and intracellular staining was performed with APC-conjugated anti–IFN-γ mAb. Representative flow cytometric data from 3 independent experiments are shown. The values in the upper right quadrants indicate IFN-γ–producing cells as a percentage of CD8 T cells. (C) Splenocytes from mice immunized with male or female H60 cells were cultured with irradiated male H60 splenocytes (mixed lymphocyte culture, MLC) for 7 days, and the CD8 effector T cells from each MLC were tested for IFN-γ. The cells were surface stained with H60-tetramer and anti–CD8-APC, and were stained for intracellular IFN-γ with FITC-conjugated mAb. Representative flow cytometric data from 3 independent experiments are shown (gated for CD8+ cells).
Next, we confirmed the Th dependency of the H60-specific response in a functional aspect. Splenocytes from the mice immunized under helped or helpless conditions were tested ex vivo for IFN-γ production in response to H60-peptide. Intracytoplasmic staining for IFN-γ production demonstrated that CD8 T cells from the helpless mice rarely responded to H60 stimulation, while 3% to 4% of those from the helped mice responded (Figure 1B). Then, we performed a modified IFN-γ secretion assay using CD8 effector cells from MLCs. The purpose was first to amplify in vitro the CD8 T cells reactive to H60 in vivo, especially those perhaps present in the helpless mice, and second to test whether tetramer-binding cells after the in vitro amplification would represent functionally active CD8 T cells. MLCs were performed using splenocytes from the immunized mice and irradiated male H60 splenocytes. Results from the IFN-γ secretion assays demonstrated that most of the H60-tetramer+ CD8 T cells present in the MLC of splenocytes from the helped mice produced IFN-γ in response to H60 stimulation, revealing a correlation between the tetramer-binding and functionally active cells (Figure 1C). In contrast, few IFN-γ–producing cells were detected even after MLC in the case of the splenocytes from the helpless mice. Altogether, these results indicate the requirement for help from HY-Dby–specific CD4 T cells during the induction of a primary H60-specific CD8 response.
CD4 help is absolutely required for an appropriate H60-specific memory response
We next investigated the effect of the presence of CD4 help on the secondary expansion of H60-specific memory CD8 T cells generated under helped conditions. To this end, female B6 mice, primed previously with male H60 cells, were divided into 2 groups. One group was boosted under helped conditions, whereas the other was boosted under helpless conditions (injected intraperitoneally with male vs female H60 cells, respectively) 70 days after primary immunization (the primary H60-specific CD8 T-cell response had left the contraction phase and entered the resting memory stage). Tetramer staining of PBLs to check for H60-specific CD8 T cells revealed a typical recall response5,19 only in the mice that had been boosted under helped conditions: the expansion of H60-tetramer+ cells (up to 40%-50% of the peripheral CD8 T cells) was detected 7 days after the second immunization (Figure 2A). After that peak, the percentage decreased rapidly up to 14 days after secondary immunization and was maintained at an easily detectable level (> 15% of the CD8 T cells) for more than 2 months. In contrast, the peak frequency of H60-tetramer+ cells during the helpless secondary response was similar to or less than that obtained during the helped primary response (6%-10%). The difference in the secondary peak frequencies between the helped and helpless recall responses was mirrored in the differences in both the specific cytotoxic effects and IFN-γ secretion levels of the 2 types of H60-reactive CD8 effector cells (Figure 2B,C). Both functional activities of the CD8 effectors were 2- to 3-fold higher in the MLC cells of the splenocytes undergoing a helped secondary response compared with those in the cells undergoing a helpless one. The difference in functional activities between the 2 types of CD8 T cells was also confirmed in ex vivo IFN-γ secretion assays (Figure S1, available on the Blood website; see the Supplemental Materials link at the top of the online article). Thus, the full development of an H60-specific memory CD8 T-cell response also depends on CD4 help.
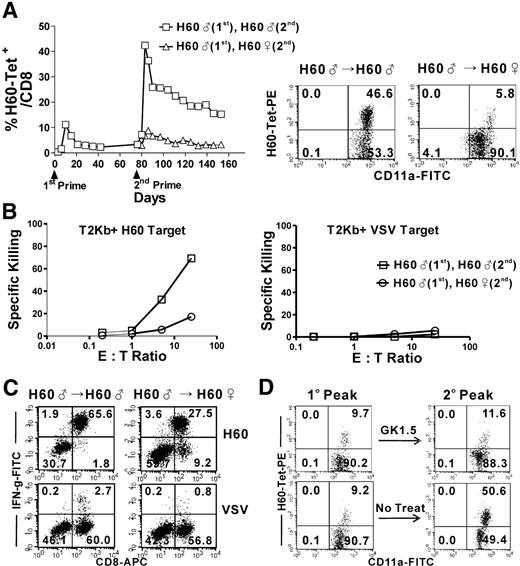
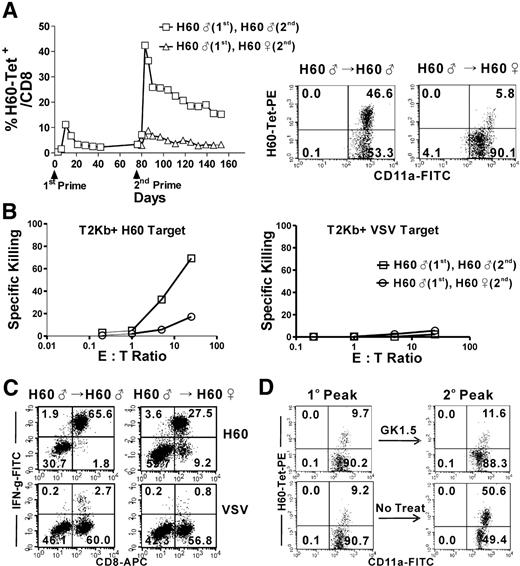
CD4 help is required for the appropriate development of a secondary H60-specific CD8 T-cell response. (A) Mice that had been previously immunized with male H60 cells were boosted with male or female H60 cells. PBLs from the twice-challenged mice (6 mice per group) were periodically checked for the binding of H60-tetramer, and the proportion of H60-tetramer+ CD11a+ cells among the CD8+ cells was plotted. Representative data from more than 10 experiments conducted on day 7 after secondary immunization are shown (gated for CD8+ cells). (B,C) CD8 effector cells from MLCs of splenocytes from the boosted mice on day 7 after secondary immunization were tested for specific cytotoxicity (B) and IFN-γ production (C) after stimulation with H60-peptide and VSV (control)–peptide. (D) The mice that had been previously immunized with male H60 cells were depleted of CD4 T cells by treatment with GK1.5 before boosting with male H60 cells. The FACS data showing the peak days for the primary (day 10 after primary immunization) and secondary (day 7 after secondary immunization) responses are compared. FACS data obtained from nondepleted mice (no treat) are shown as a control. The FACS data were gated for the CD8 T cells and are representative of 3 independent experiments.
CD4 help is required for the appropriate development of a secondary H60-specific CD8 T-cell response. (A) Mice that had been previously immunized with male H60 cells were boosted with male or female H60 cells. PBLs from the twice-challenged mice (6 mice per group) were periodically checked for the binding of H60-tetramer, and the proportion of H60-tetramer+ CD11a+ cells among the CD8+ cells was plotted. Representative data from more than 10 experiments conducted on day 7 after secondary immunization are shown (gated for CD8+ cells). (B,C) CD8 effector cells from MLCs of splenocytes from the boosted mice on day 7 after secondary immunization were tested for specific cytotoxicity (B) and IFN-γ production (C) after stimulation with H60-peptide and VSV (control)–peptide. (D) The mice that had been previously immunized with male H60 cells were depleted of CD4 T cells by treatment with GK1.5 before boosting with male H60 cells. The FACS data showing the peak days for the primary (day 10 after primary immunization) and secondary (day 7 after secondary immunization) responses are compared. FACS data obtained from nondepleted mice (no treat) are shown as a control. The FACS data were gated for the CD8 T cells and are representative of 3 independent experiments.
To verify the help-dependent nature of the H60-specific CD8 memory response, we induced a secondary response in mice that had been depleted of CD4 T cells. From this point on, all experiments involving a secondary response were performed using mice that had reached the resting memory stage (at least 40 days after primary immunization with male H60 cells). Female B6 mice in the resting memory stage were treated with GK1.5, a CD4-depleting antibody, twice before being boosted with male H60 cells, and PBLs from the mice were stained with H60-tetramer to compare the peak frequency of H60-tetramer+ CD8 T cells to that of cells obtained from nondepleted/boosted mice (Figure 2D). Full expansion of H60-specific CD8 T cells, which was observed in the latter mice (maximum of 45%-50% of the CD8 T cells), did not occur in the former (10%-20%). Taken together, these results show the crucial role of CD4 help in mounting an optimal CD8 memory response.
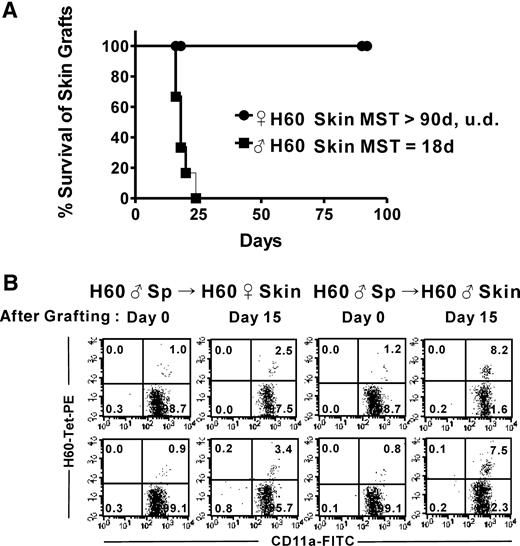
CD4 help dependency in the memory response induced by skin grafting
We next addressed whether CD4 help is required for the induction of an H60-specific CD8 memory response when skin grafting is used as the boosting method. To this end, female B6 mice in the resting memory stage underwent transplantation with male or female H60-skin, and PBLs from the grafted mice were stained with H60-tetramer. The male H60-skin grafts were rejected within 18 days on average, whereas the female H60-skin grafts remained accepted for more than 90 days (Figure 3A). The percentage of H60-tetramer+ cells in the mice grafted with male H60-skin increased from 0.6% to 1.0% before grafting to a maximum of 7% to 8% (15 days after grafting). In contrast, the percentage in the mice that underwent transplantation with female H60-skin peaked at 2% to 3% (Figure 3B). This confirms that skin transplantation induces a less vigorous proliferation of H60-specific CD8 T cells compared with spleen cell immunization.4 Our results also show that CD4 help affects the magnitude of expansion of H60-specific memory CD8 T cells and the outcome after skin transplantation.
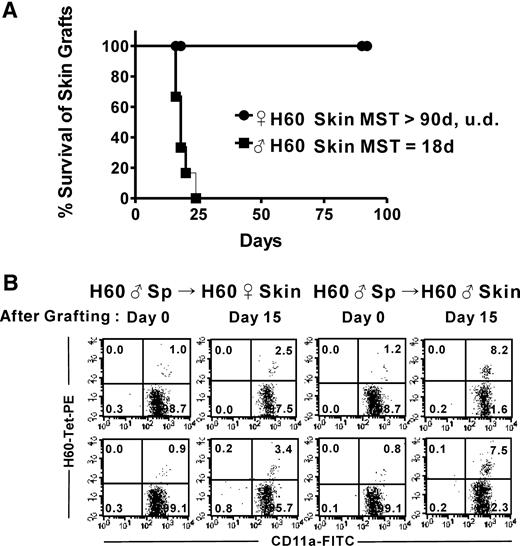
Requirement for CD4 T-cell help in the memory response is reproduced when mice are restimulated by skin transplantation. Mice that had been previously immunized with male H60 cells were transplanted with skin from male or female H60 congenic mice. (A) Mice were observed longer than 90 days after the transplantation. The data are pooled from 3 independent experiments (n = 6, P < .001). Mean survival time (MST) for each group is indicated (UD, undefined). (B) The mice were eye-bled on day 0, before skin transplantation, and on day 10 after skin transplantation. PBLs were stained with H60-tetramer-PE, anti–CD8-APC, and anti–CD11a-FITC. Flow cytometric analyses were done (gated for CD8+ cells); the data are representative of 3 independent experiments.
Requirement for CD4 T-cell help in the memory response is reproduced when mice are restimulated by skin transplantation. Mice that had been previously immunized with male H60 cells were transplanted with skin from male or female H60 congenic mice. (A) Mice were observed longer than 90 days after the transplantation. The data are pooled from 3 independent experiments (n = 6, P < .001). Mean survival time (MST) for each group is indicated (UD, undefined). (B) The mice were eye-bled on day 0, before skin transplantation, and on day 10 after skin transplantation. PBLs were stained with H60-tetramer-PE, anti–CD8-APC, and anti–CD11a-FITC. Flow cytometric analyses were done (gated for CD8+ cells); the data are representative of 3 independent experiments.
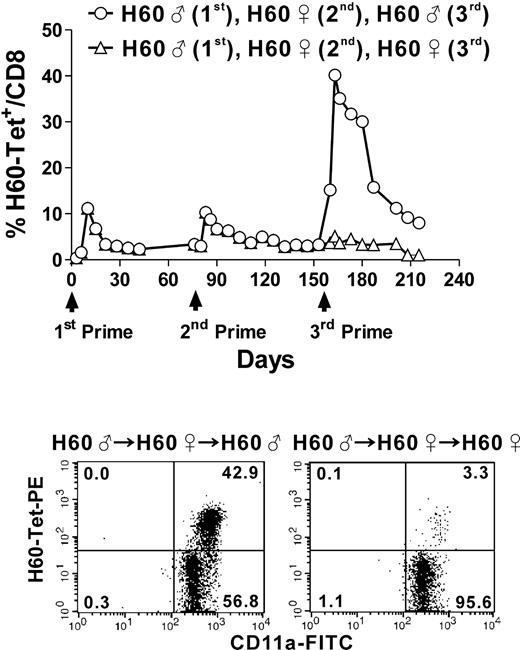
The responsiveness of H60-specific CD8 T cells to further challenge is imprinted during the primary response
A lack of CD4 help during the primary CD8 T-cell response has been shown to induce nonresponsiveness in CD8 T cells to further stimulation.20,21 Thus, we examined whether the H60-specific CD8 memory T cells that had been unable to undergo vigorous expansion during a helpless secondary response had acquired any properties leading to nonresponsiveness to a subsequent challenge. To test this, we immunized mice that had gone through a helpless secondary response with male or female H60 cells, and the frequency of H60-tetramer+ CD8 T cells was monitored along with the development of a tertiary response. When CD4 help was provided again during the tertiary response, the H60-specific cells showed robust expansion (up to 40%-45% of the CD8 T cells; Figure 4). However, a lack of CD4 help upon the tertiary challenge after a helpless secondary response reduced the maximum frequency of H60-tetramer+ cells to approximately 3% of the CD8 T cells. This demonstrates that, during the helpless secondary response, the H60-specific CD8 T cells maintained their capacity for re-expansion upon the encounter of the same antigen; that is, the fate decision of the H60-specific CD8 T cells in terms of their responsiveness/nonresponsiveness to further challenge was fixed during the primary response.14
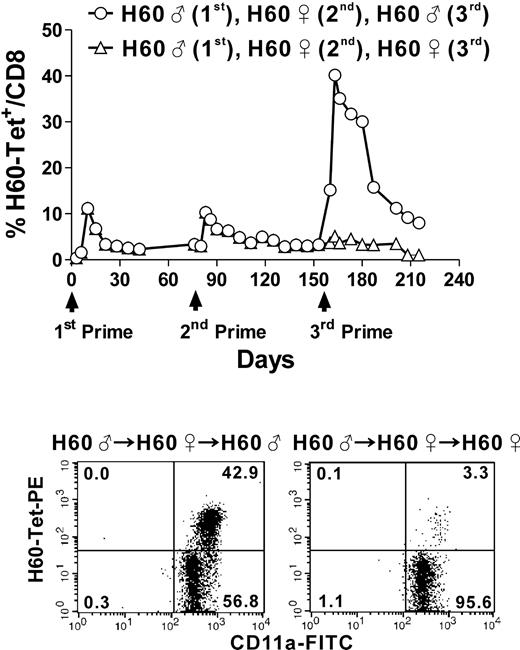
Providing CD4 help again to memory CD8 T cells that had not undergone an appropriate secondary response restored memory cell expansion during the tertiary response. Mice that had not been provided with CD4 help during the secondary response were immunized with male or female H60 cells as a tertiary challenge. The percentage of H60-tetramer+ CD11a+ CD8 T cells was plotted after periodic staining of PBLs from the immunized mice (3 mice per group). Representative FACs data from 3 independent experiments (gated for CD8+ cells) are shown.
Providing CD4 help again to memory CD8 T cells that had not undergone an appropriate secondary response restored memory cell expansion during the tertiary response. Mice that had not been provided with CD4 help during the secondary response were immunized with male or female H60 cells as a tertiary challenge. The percentage of H60-tetramer+ CD11a+ CD8 T cells was plotted after periodic staining of PBLs from the immunized mice (3 mice per group). Representative FACs data from 3 independent experiments (gated for CD8+ cells) are shown.
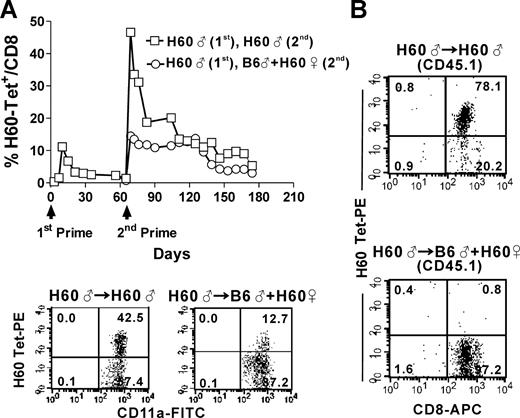
Cognate and noncognate CD4 help has qualitatively and quantitatively different effects on the CD8 memory T-cell response
Based on the aforementioned results, we hypothesized that the role of CD4 help during memory responses would be to encourage the expansion of proliferation-competent CD8 T cells by providing soluble cytokines in the vicinity of H60-reactive CD8 T cells. Therefore, we investigated whether CD4 T-cell activation via noncognate recognition of different APCs from those that memory CD8 T cells recognize would support memory expansion to the same extent as cognate CD4 help, because separately activated CD4 T cells would supply soluble cytokines to the memory CD8 T cells nearby. To test the effects of separate and cognate CD4 help on the memory CD8 T-cell response, we boosted mice in the resting memory stage with a mixture of female H60 cells and male B6 cells (separate-help) or with male H60 cells (cognate-help), and compared the peak burst sizes of the 2 secondary responses. The peak frequency of H60-tetramer+ cells was quite low when separate-help was provided (∼13% of the CD8 T cells). Moreover, the overall kinetics of the secondary response provided with separate-help differed significantly from that observed with cognate-help: low peak frequencies were maintained for more than 1.5 months and then gradually declined, rather than precipitously dropping off as was observed when cognate-help was delivered (Figure 5A).
Separate and cognate help lead to qualitatively and quantitatively different H60-specific memory CD8 T-cell responses. (A) B6 mice that had been immunized with male H60 cells were boosted with male H60 cells or a mixture of male B6 and female H60 cells. PBLs from the immunized mice (5 mice per group) were stained periodically with H60-tetramer-PE, anti–CD8-APC, and anti–CD11a-FITC, and the percentage of H60-tetramer+ CD11a+ CD8 T cells was plotted. The FACs results from day 7 postsecondary immunization are shown (gated for CD8+ cells). The data are taken from 1 of 5 independent experiments. (B) Female B6 mice were adoptively transferred with CD8 T cells purified from female Ly5.1 (CD45.1+) mice that had been immunized with male H60 cells 40 days earlier and then challenged with male H60 cells or a mixture of male B6 and female H60 cells. PBLs from the challenged adoptive hosts were stained with H60-tetramer-PE, anti–CD8-APC, and anti–CD45.1-FITC and flow cytometric analysis was performed after gating for the CD45.1+ cells. The data are representative of 2 independent experiments.
Separate and cognate help lead to qualitatively and quantitatively different H60-specific memory CD8 T-cell responses. (A) B6 mice that had been immunized with male H60 cells were boosted with male H60 cells or a mixture of male B6 and female H60 cells. PBLs from the immunized mice (5 mice per group) were stained periodically with H60-tetramer-PE, anti–CD8-APC, and anti–CD11a-FITC, and the percentage of H60-tetramer+ CD11a+ CD8 T cells was plotted. The FACs results from day 7 postsecondary immunization are shown (gated for CD8+ cells). The data are taken from 1 of 5 independent experiments. (B) Female B6 mice were adoptively transferred with CD8 T cells purified from female Ly5.1 (CD45.1+) mice that had been immunized with male H60 cells 40 days earlier and then challenged with male H60 cells or a mixture of male B6 and female H60 cells. PBLs from the challenged adoptive hosts were stained with H60-tetramer-PE, anti–CD8-APC, and anti–CD45.1-FITC and flow cytometric analysis was performed after gating for the CD45.1+ cells. The data are representative of 2 independent experiments.
To differentiate the memory CD8 T cells from primary activated CD8 T cells, we adoptively transferred CD45.1+ CD8 T cells purified from Ly5.1 (CD45.1+) mice in the resting memory stage after male H60 cell immunization into female B6 mice (adoptive memory hosts), and induced an H60-specific memory response in the adoptive hosts under either cognate- or separate-help conditions. Staining of PBLs from the primed adoptive hosts for CD45.1 marker expression and H60-tetramer–binding by the CD8 T cells revealed that, although most of the CD45.1+ CD8 T cells (> 70%) bound H60-tetramer in the presence of cognate-help, H60-tetramer+ CD8 T cells were rare in the CD45.1+ population when separate-help was provided (Figure 5B). This indicates a clear difference in the ability of the 2 types of CD4 help to support memory CD8 T-cell expansion given a limited starting number (3 × 106) of CD45.1+ memory CD8 T cells. Together, these data show that cognate and separate CD4 help lead to qualitatively and quantitatively different CD8 memory responses. This difference may be due to a direct cellular interaction among CD4 T cells, APCs, and CD8 T cells that is possible only under cognate CD4 help conditions.
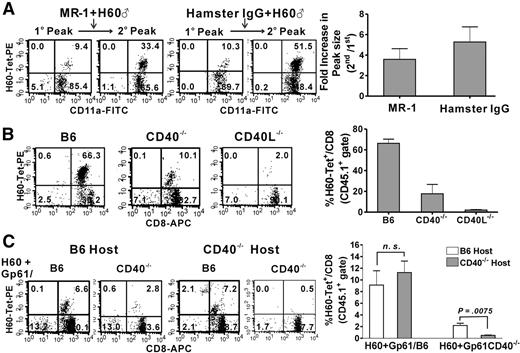
Both CD40 and CD40L are required for the expansion of H60-specific CD8 memory T cells; however, the role of CD40 expressed by APCs cannot be substituted for CD40 expressed by memory CD8 T cells
CD40 and CD40L are considered to be major mediators of CD4 help through the cognate 3-cell (CD4 T-cell, APC, and CD8 T-cell) interaction.6,9,22,23 In most cases, the role of CD40-CD40L engagement and the significance of CD40L expression by CD4 T cells have been examined in CD40L−/− mice. However, the necessity of CD40 expressed by APCs in the production or recall expansion of memory CD8 T cells is controversial.24-27 We previously found that an H60-specific CD8 T-cell response could not be induced in CD40−/− or CD40L−/− mice but that supplementation of normal CD4 T cells into CD40L−/− mice restored responsiveness.18 Here, we examined whether CD40 and CD40L, especially CD40 expressed by host APCs, are necessary for the recall expansion of H60-specific memory CD8 T cells.
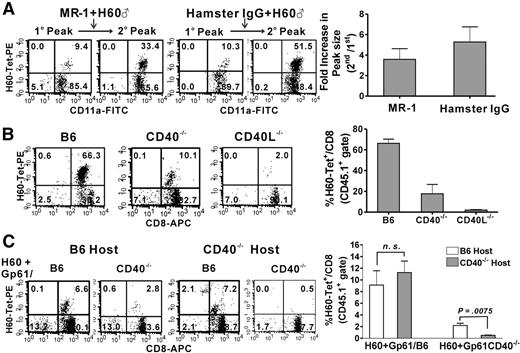
First, we investigated the effect of a CD40L-blocking Ab (MR-1) on the H60-specific CD8 memory response. Female B6 mice in the resting memory stage were treated with 0.5 mg MR-1 at the time of boosting with male H60 cells and at 2 additional time points thereafter, and the peak burst size of H60-tetramer+ CD8 T cells during the secondary response was determined. MR-1 treatment reduced the peak size of the secondary response (∼33% of the CD8 T cells on average) and, thereby, the fold-increase of the secondary peak relative to the primary peak (3.5-fold), compared with the values (∼52% and 5.2-fold, respectively) obtained using hamster IgG-treated control mice (Figure 6A). This implies that the blockage of the CD40-CD40L interaction hampers the normal expansion of H60-specific memory CD8 T cells and that treatment with MR-1 might be insufficient to block the interaction completely.
CD40 and CD40L are both required for the induction of an H60-specific CD8 memory response. (A) Either 0.5 mg MR-1(anti-CD40L mAb) or hamster IgG was injected intraperitoneally into mice that had been previously immunized with male H60 cells at the time of boosting with male H60 cells and 2 times afterward at 3-day intervals. PBLs were stained on day 7 after boosting. FACs data obtained at the primary and secondary peaks are shown in parallel (gated for CD8+ cells). The fold-increase in peak size between the secondary and primary responses is plotted, and the error bars represent the standard deviation (SD). The data are representative of 3 independent experiments. (B) CD8 T cells purified from Ly5.1 (CD45.1+) congenic mice that had been previously immunized with male H60 cells were adoptively transferred to female B6, CD40L−/−, and CD40−/− hosts. The adoptive hosts were then primed with male H60 cells, and the PBLs were stained with H60-tetramer-PE, CD8-APC, and CD45.1-FITC. The FACs data shown are taken from 1 of 4 independent experiments and were obtained on day 7 after priming (gated for CD45.1+ cells). The percentage of H60-tetramer+ cells among the CD45.1+ CD8 T cells in the adoptive hosts is plotted and error bars represent the SD. (C) CD40−/− or B6 adoptive hosts transferred with memory CD45.1+ CD8 T cells were primed with peptide (H60 + Gp61)–loaded splenocytes from CD40−/− or normal B6 mice. Representative FACS data shown were obtained after staining of the PBLs on day 10 after priming with peptide-loaded cells. The percentage of H60-tetramer+ cells among the CD45.1+ CD8 T cells in the B6 or CD40−/− adoptive hosts is plotted with error bars representing the SD (NS, not significant). Representative data were taken from 5 independent experiments.
CD40 and CD40L are both required for the induction of an H60-specific CD8 memory response. (A) Either 0.5 mg MR-1(anti-CD40L mAb) or hamster IgG was injected intraperitoneally into mice that had been previously immunized with male H60 cells at the time of boosting with male H60 cells and 2 times afterward at 3-day intervals. PBLs were stained on day 7 after boosting. FACs data obtained at the primary and secondary peaks are shown in parallel (gated for CD8+ cells). The fold-increase in peak size between the secondary and primary responses is plotted, and the error bars represent the standard deviation (SD). The data are representative of 3 independent experiments. (B) CD8 T cells purified from Ly5.1 (CD45.1+) congenic mice that had been previously immunized with male H60 cells were adoptively transferred to female B6, CD40L−/−, and CD40−/− hosts. The adoptive hosts were then primed with male H60 cells, and the PBLs were stained with H60-tetramer-PE, CD8-APC, and CD45.1-FITC. The FACs data shown are taken from 1 of 4 independent experiments and were obtained on day 7 after priming (gated for CD45.1+ cells). The percentage of H60-tetramer+ cells among the CD45.1+ CD8 T cells in the adoptive hosts is plotted and error bars represent the SD. (C) CD40−/− or B6 adoptive hosts transferred with memory CD45.1+ CD8 T cells were primed with peptide (H60 + Gp61)–loaded splenocytes from CD40−/− or normal B6 mice. Representative FACS data shown were obtained after staining of the PBLs on day 10 after priming with peptide-loaded cells. The percentage of H60-tetramer+ cells among the CD45.1+ CD8 T cells in the B6 or CD40−/− adoptive hosts is plotted with error bars representing the SD (NS, not significant). Representative data were taken from 5 independent experiments.
Second, we performed adoptive transfer experiments to substantiate the role of CD40 and CD40L in the memory expansion of H60-specific CD8 T cells. We adoptively transferred CD45.1+ memory CD8 T cells to CD40−/− and CD40L−/− hosts and tracked the CD45.1+ H60-tetramer+ CD8 T cells after priming with male H60 cells. In the CD40L−/− hosts, CD45.1+ H60-tetramer+ CD8 T cells were rare after priming (∼2.0% of the CD45.1+CD8+ T cells), which confirms the crucial role of CD40L in the memory expansion of H60-specific CD8 T cells.18 However, CD45.1+ H60-tetramer+ CD8 T cells were detected more frequently (10%-30% of the CD45.1+CD8+ T cells; 18% on average) in the CD40−/− hosts, even though the values were significantly lower than those (60%-75% of the CD45.1+CD8+ T cells; 67% on average) in control B6 wild-type (WT) hosts (Figure 6B). This shows that CD40 expressed by host APCs plays a role in the memory expansion of H60-specific CD8 T cells. However, marginally normal CD40 function appears to be supplemented in the CD40−/− hosts, probably by male H60 cells used for priming or the transferred CD45.1+ memory CD8 T cells, or both.
It has been reported that CD4 T cells can deliver help directly to CD8 T cells via CD40 expressed on activated CD8 T cells.24 To test whether memory CD8 T-cell expansion can occur when CD40 is present only on memory CD8 T cells, we primed adoptive CD40−/− hosts with splenocytes from CD40−/− mice after peptide loading and compared the extent of expansion of CD45.1+ H60-tetramer+ CD8 T cells with that in CD40−/− hosts primed with peptide-loaded WT splenocytes. Experiments included B6 adoptive hosts as controls. Gp61 peptide from LCMV was coloaded with H60 peptide onto splenocytes as the H-2Ab–restricted CD4 epitope, replacing the HY-Dby CD4 epitope, because our preliminary experiments showed that the immunization of B6 mice with splenocytes loaded with Gp61 instead of HY-Dby induced a stronger H60-specific CD8 T-cell response (data not shown). Overall, an H60-specific CD8 T-cell response was weakly induced by immunization with the peptide-loaded splenocytes compared with immunization with H60 cells. Therefore, a 2-fold greater number (6 × 106) of CD45.1+CD8 T cells was adoptively transferred to detect CD45.1+ H60-tetramer+ CD8 T cells (9% of CD45.1+ CD8 T cells on average) in B6 adoptive hosts primed with the peptide-loaded WT splenocytes (Pep/WT-cells; Figure 6C). Priming with peptide-loaded CD40−/− splenocytes (Pep/CD40−/−-cells), however, resulted in a low degree (3% on average) of CD45.1+ H60-tetramer+ CD8 T-cell expansion in the B6 hosts, implying a more significant CD40 role played by priming cells than by host APCs in the case of challenge with peptide-loaded cells. In line with this, immunization with Pep/WT-cells induced a detectable level (11% on average) of their expansion in the CD40−/− hosts. However, expansion was barely detectable in the CD40−/− hosts (0.5% on average) after immunization with Pep/CD40−/−-cells, that is, in the case in which both priming cells and host APCs lacked CD40 expression (Figure 6C). This indicates that CD40 expressed by memory CD45.1+ CD8 T cells plays no role in the expansion of H60-specific memory CD8 T cells. Moreover, these data, together with those obtained from the immunization of CD40−/− adoptive hosts with H60 cells, demonstrate the involvement of direct- and cross-presentation pathways in H60-specific CD8 memory responses. Together, our data clearly show that CD40L and CD40 play roles in the memory expansion of H60-specific CD8 T cells.
Discussion
In this study, we characterized the H60-specific CD8 memory T-cell response, focusing on the effects of the presence or absence of CD4 help on the expansion of memory CD8 T cells upon restimulation, as well as the underlying mechanism. Our results demonstrate the requirement of cognate CD4 help for the reactivation and secondary expansion of once-helped H60-specific memory CD8 T cells and the involvement of both CD40 and CD40L in memory expansion.
Several studies have suggested that once memory CD8 T cells have been generated under CD4 help-sufficient conditions, CD4 help is dispensable for the rapid expansion of those cells during a recall response.11,12,28 However, the CD4-helped memory CD8 T cells generated against H60 in this study remained dependent on CD4 help for their re-expansion after a second challenge. Moreover, the necessity of CD4 help for the proper development of each memory response was emphasized by the continued downsizing of the burst peak caused by a consecutive lack of CD4 help during the tertiary response after a helpless secondary response. The discrepancies between our results and those from previous studies may be ascribed to the use of different experimental antigens. Whereas we strictly confined the delivery of our specific antigen to a cell-based form, such as splenocyte injection or skin transplantation, most previous studies have used inflammatory infectious antigens that can directly activate DCs via pattern recognition receptors.29-31 In line with this, memory CD8 T cells expressing HY-specific Tg TCRs have been found to expand highly when cotransferred with CD4 T cells into RAG-deficient HY-expressing BM chimeric hosts, compared with the single transfer of memory CD8 T cells.15 Therefore, CD8 T cells reactive to Th-dependent antigens may be more reliant on continuous CD4 help from the primary through the recall response. Our findings, which focus on endogenous recall responses to a naturally occurring minor H antigen, are pertinent to understanding how immunity is generated and maintained in response to “endogenous” noninflammatory stimuli encountered during transplantation, and how it can be exploited for use in anti-tumor therapy.
Despite the reported role of CD4 help as a supplier of soluble cytokines to CD8 T cells, such as IL-2,32-34 IL-4,35 and IL-15,36 the cellular interaction mediated by the cognate recognition of APCs by CD4 and CD8 T cells and the involvement of CD40 and CD40L was found to be more important for the development of an H60-specific CD8 T cell memory response. The requirement for CD40L was readily confirmed by our adoptive transfer experiments (Figure 6A), probably because of its expression on CD4 T cells. However, the significance of CD40 in memory expansion was revealed only when both the hosts and priming cells were CD40-deficient (Figure 6B).
A direct CD40-CD40L interaction between CD4 and CD8 T cells has been described as a mechanism for the delivery of help to HY-specific TCR Tg CD8 T cells.24 However, the direct involvement of CD40 expressed by CD8 T cells has not been reproduced in other primary or memory responses,26,27,37 and the difference has been ascribed to a difference in the nature of the model antigen (Th-dependent vs Th-independent). Despite the Th-dependent nature of H60 and HY, the H60-specific CD45.1+ memory CD8 T cells from the WT background were unable to compensate for the lack of CD40 in the hosts and priming-cells (peptide-loaded CD40−/− splenocytes), confirming the insignificant role of CD40 expressed by memory CD8 T cells in their expansion. The reason for this difference is not clearly understood, but it might be due to differences in the experimental settings (using monoclonal TCR Tg CD8 T cells vs. polyclonal T cells and testing of the primary response vs. the memory response). Alternatively, CD40−/− HY-TCR Tg CD8 T cells themselves may be defective in terms of activation.
Boosting WT mice with peptide-pulsed CD40−/− or WT DCs resulted in memory CD8 T cell responses with similar levels of cytotoxicity, suggesting that when memory CD8 T cells are generated in a CD4 help- and CD40-sufficient environment, their reactivation does not require CD40 expression on DCs.27 According to our results showing that memory expansion was abolished only when both the adoptive hosts and immunizing cells lacked CD40 expression, the presence of CD40 in the host likely compensated for the lack of CD40 on the immunizing DCs, resulting in a similar degree of cytotoxic activity in the reactive CD8 T cells between restimulation with WT and CD40−/− DCs. Based on our data, CD40 appears to play a significant role in the reactivation of memory CD8 T cells, at least against the Th-dependent antigen H60.
We noticed several differences between the H60-specific primary and secondary responses. The primary CD8 response induced by male H60 cell immunization was not detected in CD40−/− hosts18 or in CD40−/− hosts adoptively transferred with naive CD45.1+ CD8 T cells (data not shown), whereas memory cell expansion was detected in CD40−/− adoptive hosts given the same challenges. Moreover, treatment with 0.5 mg MR-1, which was sufficient to completely block the primary response in our preliminary tests (data not shown), only partly reduced the memory expansion of the H60-specific CD8 T cells. These differences could have been due to the increased precursor frequency of H60-reactive cells available for the memory response,38 on top of their high precursor frequency in the naive pool.17 Moreover, there could be qualitative differences between the naive and memory CD8 T cells that render the memory CD8 T cells more sensitive to antigen stimulation. Memory CD8 T cells, generated in the presence of CD4 help, have been reported to express high levels of CD27, and the ligation of CD27 during restimulation has been shown to increase secondary expansion and autocrine IL-2 production.39 Whatever the reason for these differences, the absolute requirement for CD4 help and the involvement of CD40 and CD40L in producing an optimal H60-specific CD8 response is preserved between the primary and memory responses. It is well known that CD4 help during the primary response gives CD8 T cells a high capacity for expansion upon rechallenge. Our results raise the question as to what program is encoded into memory CD8 T cells by CD4 help during the secondary response.
In summary, we report here the necessity of CD4 help for the memory expansion of H60-specific cells, and the involvement of CD40 and CD40L in that process. This study is the first to follow the endogenous response of CD8 T cells specific for a dominant minor H antigen expressed on hematopoietic cells. Our results should provide guidance for maximizing the graft-versus-leukemia response after bone marrow transplantation.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
We thank Dr Derry Roopenian (The Jackson Laboratory) for critically reviewing this manuscript.
This study was supported by grants from the Korea Science and Engineering Foundation (R01-2006-000-10 565-0) and Seoul National University Hospital (03-2005-030), and was performed under BK21 program of Korea.
Authorship
Contribution: S.J.R. performed experiments, analyzed data, and wrote the paper; K.M.J. helped design and perform experiments and analyzed data; H.S.Y. and S.K. performed experiments; T.W.K. and J.C. helped design research; and E.Y.C. designed research, interpreted data, and wrote the paper.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Eun Young Choi, Department of Biomedical Sciences, Biomedical Science Bldg, Rm 310, Seoul National University College of Medicine, 103 Daehang-ro, Seoul 110-799, Korea; e-mail: eycii@snu.ac.kr.
References
Author notes
*S.J.R. and K.M.J. contributed equally to this manuscript.