Abstract
Proteasome inhibition is a validated strategy for therapy of multiple myeloma, but this disease remains challenging as relapses are common, and often associated with increasing chemoresistance. Moreover, nonspecific proteasome inhibitors such as bortezomib can induce peripheral neuropathy and other toxicities that may compromise the ability to deliver therapy at full doses, thereby decreasing efficacy. One novel approach may be to target the immunoproteasome, a proteasomal variant found predominantly in cells of hematopoietic origin that differs from the constitutive proteasome found in most other cell types. Using purified preparations of constitutive and immunoproteasomes, we screened a rationally designed series of peptidyl-aldehydes and identified several with relative specificity for the immunoproteasome. The most potent immunoproteasome-specific inhibitor, IPSI-001, preferentially targeted the β1i subunit of the immunoproteasome in vitro and in cellulo in a dose-dependent manner. This agent induced accumulation of ubiquitin-protein conjugates, proapoptotic proteins, and activated caspase-mediated apoptosis. IPSI-001 potently inhibited proliferation in myeloma patient samples and other hematologic malignancies. Importantly, IPSI-001 was able to overcome conventional and novel drug resistance, including resistance to bortezomib. These findings provide a rationale for the translation of IPSIs to the clinic, where they may provide antimyeloma activity with greater specificity and less toxicity than current inhibitors.
Introduction
The ubiquitin-proteasome pathway is used by eukaryotes as the major mechanism for regulated intracellular proteolysis. As such, it plays an important role in cellular homeostasis, and is critical to several processes, including angiogenesis, cell-cycle progression, DNA repair, programmed cell death, and the stress response.1,2 This pathway has become a validated target for cancer therapy with the approval of the proteasome inhibitor bortezomib as a single agent for mantle cell lymphoma3-5 and multiple myeloma (MM).6-8 Modulation of proteasome function is also a rational approach to achieve chemosensitization, and bortezomib with pegylated liposomal doxorubicin has recently been shown to be superior to bortezomib alone against MM.9 These successes have led to studies of the role of bortezomib in the up-front setting in myeloma, and to the introduction in early phase studies of a second generation of irreversible proteasome inhibitors, such as carfilzomib10 and NPI-0052.11,12
In its assembled form, the proteasome consists of a core 20S particle with 4 stacked rings of 7 subunits each. Most cells express the constitutive proteasome variant, in which the 20S core is capped on both ends by a 19S activator complex, which aids in stabilization, ATP-dependent removal of ubiquitin, and unfolding/shuttling of proteins into the core. The inner 2 rings contain β subunits numbered 1 through 7, of which β1, β2, and β5 participate in proteolysis.11-13 These encode the 3 major catalytic activities of the proteasome: chymotrypsin-like (ChT-L), trypsin-like (T-L), and post–glutamyl peptide hydrolyzing, or caspase-like (C-L) activities. One variant of the proteasome that has been described is the immunoproteasome, which differs from the constitutive proteasome in part through the replacement of β1, β2, and β5, with distinct subunits known as β1i, β2i, and β5i, to form the 20Si core.14,15 This variant, which also contains different regulatory subunits known as 11S or PA28,16 has been found to be highly expressed in cells of hematopoietic origin in several species.17-19 Studies of 20Si function have revealed that it generates peptide fragments with more hydrophobic and basic amino acids at the C-terminus,20 which are better suited for presentation to major histocompatability class I molecules, providing the rationale for its name. However, the 20Si also participates in many constitutive proteolytic processes,17,19,21-24 and conversely the 20S proteasome may in some cases generate immunogenic epitopes,25 suggesting that each proteasome variant may provide both housekeeping and specialized functions.
The role that the 20Si plays outside of the immune system is just beginning to be elucidated, with expression levels being correlated to several disease states, including Huntington disease,26 Alzheimer disease,27 and macular degeneration.28 Diseases associated with an aberrant immune response, such as inflammatory bowel disease29,30 and rheumatoid arthritis,31 have also been identified as having increased 20Si expression. This may be due in part to the ability of inflammatory cytokines, such as tumor necrosis factor and interferon-γ, to induce expression and preferential incorporation of β1i, β2i, and β5i into the proteasome.16 Preferential expression of 20Si has also been observed in MM,32 suggesting that specific immunoproteasome inhibition could be a promising therapeutic strategy. While bortezomib, carfilzomib, and NPI-0052, as well as other proteasome inhibitors, have been validated in myeloma and other model systems, all of these appear to target both the constitutive and immunoproteasomes indiscriminately. This lack of specificity may in part explain some of the side effects of these agents, such as peripheral neuropathy and gastrointestinal effects, which may be due to targeting of the constitutive proteasome in these tissues. In contrast, by selectively inhibiting the 20Si, it may be possible to maintain antimyeloma and antilymphoma efficacy while reducing these toxicities, thereby increasing the therapeutic index.
In this work, we describe the identification of a series of immunoproteasome-specific inhibitors (IPSIs) using an in vitro screen, and characterization of a lead compound, IPSI-001, which showed the greatest selectivity between proteasome variants. IPSI-001 induced cell death preferentially in 20Si-containing cells in a dose-dependent fashion through activation of both intrinsic and extrinsic apoptotic pathways. This agent also induced apoptosis in patient-derived myeloma samples, as well as samples from patients with other hematologic malignancies. Importantly, we found that IPSI-001 was able to overcome resistance not only to conventional chemotherapeutics, but also to bortezomib. Although this first generation of IPSIs in a peptidyl-aldehyde backbone has lower potency, they will be useful for proof-of-principle studies, and can be used as a backbone upon which other chemistries can be added, such as boronic acids, to enhance their potency further. Taken together, these data provide a rationale for further study of IPSIs as possible anticancer drugs, especially in the myeloma setting.
Methods
Cell models and cell culture
RPMI 8226, ANBL-6, KAS-6/1, Sup-B8, 8226.Dox40, 8226.LR5, 8226.BR, MM1.S, MM1.R, peripheral blood mononuclear cells (PBMCs), and patient-derived cells were cultured in RPMI 1640 with 2 mM l-glutamine (Invitrogen, Carlsbad, CA). SK-N-MC, HeLa, BT-474, HT-29, and Hs294T cells were grown in DMEM containing l-glutamine and 110 mg/L sodium pyruvate (Invitrogen). SK-N-MC cells were further supplemented with 1× MEM nonessential amino acids. Human pancreatic carcinoma cells (HPACs) were cultured in a 1:1 mixture of Dulbecco modified Eagle and Ham F12 medium containing 1.2 g/L sodium bicarbonate, 2.5 mM l-glutamine, 15 mM HEPES, and 0.5 mM sodium pyruvate supplemented with 0.002 mg/mL insulin, 40 ng/mL hydrocortisone, and 10 ng/mL epidermal growth factor. Single donor human umbilical vein endothelial cells (HUVECs) were maintained with endothelial cell growth medium (PromoCell, Heidelberg, Germany). All cell lines except HUVECs were supplemented with 10% fetal bovine serum (Sigma-Aldrich, St Louis, MO), 100 U/mL penicillin, and 100 μg/mL streptomycin (Invitrogen) and maintained in 5% CO2 at 37°C. Interleukin-6 (IL-6)–dependent cells and purified plasma cells from patients were supplemented with 1 ng/mL IL-6 (R&D Systems, Minneapolis, MN). Patient samples were collected under a protocol approved by the University of North Carolina at Chapel Hill Institutional Review Board. Informed consent was obtained in accordance with the Declaration of Helsinki. Mononuclear cells from bone marrow aspirates or peripheral blood were isolated by density gradient centrifugation over Ficoll-Paque Plus (Amersham Biosciences, Piscataway, NJ). Malignant cells were then isolated by immunomagnetic bead positive selection in a Midi magnetic-activated cell separation (MACS) LS column following the manufacturer's protocol (Miltenyi Biotec, Auburn, CA).10 LNCaP and PC-3 prostate cancer cell pellets were a gift from Dr Young Wang (University of North Carolina at Chapel Hill). MOLT-4, U937, AML-193, and CCRF-CEM cell pellets were a gift from Dr Beverly Mitchell (Stanford Cancer Center, Stanford, CA).
Proteasome purification and competitive binding assays
Isolation of 20S and 20Si preparations from bovine pituitary and spleen was performed as described previously.33,34 Competitive binding profiles of IPSI-001 using [14C]-3,4-dichloroisocoumarin as an active-site probe,33 and competitive binding profiles using VS-L3-AHx3-danysl,10,35 were obtained as described previously.
Inhibitor synthesis
Measurement of proteasome activity
The ChT-L activity in purified proteasome preparations was determined using the substrate carbobenzoxy-glycyl-glycyl-phenylalanyl-para-aminobenzoate. ChT-L activity releases the para-aminobenzoate, which is then quantified as previously described.33,34 C-L activity was determined with the substrate carbobenzoxy-leucyl-leucyl-aspartyl-2-naphthylamide in an analogous fashion.33,34 Studies of 20S and 20Si proteasome activity in vitro in cellular extracts, or in intact cells in culture (in cellulo), were performed as described previously.36
Immunoblotting
Whole-cell extracts were prepared and separated by denaturing gel electrophoresis as described previously.37 The antibodies used included antiactin, anti-JNK, antiubiquitin, and antirat secondary antibodies (Santa Cruz Biotechnology, Santa Cruz, CA), anti-Bax, anti–p-JNK (Thr138/Tyr185), and anti–poly-(ADP-ribose) polymerase (PARP; EMD Biosciences, San Diego, CA), anti–HSC-70 antibodies (Stressgen, San Diego, CA), and antimouse and antirabbit secondary antibodies (Amersham Biosciences).
Cell viability and apoptosis assays
The WST-1 reagent was used to determine cellular viability, whereas detection of apoptotic DNA fragmentation was performed using the Cell Death Detection ELISAPLUS kit (both from Roche Diagnostics, Indianapolis, IN). Fold increase in DNA fragmentation is presented as the mean relative to vehicle-treated controls as described previously.10 Caspase-3, -8, and -9 activation was evaluated using fluorogenic substrates (BioMol, Plymouth Meeting, PA). Externalization of phosphatidyl-serine was examined by annexin V (BioVision, Mountain View, CA) and TO-PRO-3 (Invitrogen) staining, followed by analysis using fluorescence-activated cell sorting (FACS). Drug-specific apoptosis was calculated as follows: [(% live in control − % live in treated)/% live in control]. Changes in the mitochondrial transmembrane potential were determined using the JC-1 dye (Invitrogen). All of these assays were performed as described previously,10 and according to the manufacturer's specifications. In some cases, colorimetric substrates (R&D Systems) were used to examine caspase activation initially following the same protocol as the fluorogenic assays, except samples were then read in a multilabel plate reader (Victor 3V; Perkin-Elmer, Waltham, MA) at 405 nm. Results were expressed as fold activation over the vehicle control.
Results
IPSI-001 inhibits the immunoproteasome
To identify potentially isoform-specific proteasome inhibitors, the 20S and 20Si were purified to homogeneity from pituitary and spleen tissues, respectively.33 These preparations were then used to screen a panel of rationally designed peptidyl-aldehyde inhibitors using substrates specific for the ChT-L and C-L activities.34 The peptidyl-aldehyde version of bortezomib, Z-FL-CHO, showed Ki's of 2.1 and 5.55 μM against the ChT-L activity of the 20Si and 20S proteasomes, respectively (Table 1). By increasing the hydrophobicity of the amino acid in the P1, or C-terminal position, however, greater selectivity could be achieved for the immunoproteasome, in that inhibitory potency was maintained for the immunoproteasome, but decreased for the constitutive proteasome. This was most notable in the case of carbobenzoxy-leucyl-norleucinal (Z-LnL-CHO, or IPSI-001; Figure 1A), which showed a 100-fold preference for the immunoproteasome, with a Ki of 1.03 μM against the ChT-L 20Si activity, compared with 105 μM against the constitutive proteasome (Table 1). IPSI-001 also had a preference for the branched chain amino acid preferring activity of the immunoproteasome, with a Ki of 1.45 μM compared with 239 μM for the constitutive proteasome (Table 1).
IPSI-001 inhibits the immunoproteasome. (A) Chemical structure of IPSI-001. (B) Competitive binding experiment to determine subunit binding profile of IPSI-001 in purified proteasomes from bovine pituitaries (20S) and spleen (20Si). Purified proteasomes were incubated with 10 or 50 μM IPSI-001 or vehicle (Veh) for 20 minutes, and then [14C]-3,4-dichloroisocoumarin was added for an additional 30 minutes. Proteasomes were then separated by denaturing gel electrophoresis and the binding profile was identified using autoradiography. Subunit identifications were made based on the known electrophoretic migration patterns of immunoproteasome and constitutive proteasome subunits. (C) Competitive binding experiment to determine the subunit binding profile of IPSI-001 in ANBL-6 cells. Cells were treated for 4 hours with IPSI-001, followed by addition of the VS-L3-AHx3-dansyl reagent that binds to all unoccupied catalytic subunits. Protein extracts were then separated by denaturing gel electrophoresis and probed by Western blotting using an antidansyl antibody to visualize binding patterns. Antiactin was used as a loading control and anti-β1i was used to confirm the relative position of β1i. (D) In vitro assay for the 3 major catalytic activities of the proteasome in ANBL-6 cell lysates (5 μg) exposed to increasing concentrations of IPSI-001 in triplicate. Representative data are shown as the mean plus or minus standard deviation (SD) from 3 independent experiments. *P < .05 for proteasome inhibitory activity over control. (E) Western blot analysis of the accumulation of polyubiquitinated proteasome substrates in response to 50 μM IPSI-001 treatment in ANBL-6 cells over a period of 24 hours.
IPSI-001 inhibits the immunoproteasome. (A) Chemical structure of IPSI-001. (B) Competitive binding experiment to determine subunit binding profile of IPSI-001 in purified proteasomes from bovine pituitaries (20S) and spleen (20Si). Purified proteasomes were incubated with 10 or 50 μM IPSI-001 or vehicle (Veh) for 20 minutes, and then [14C]-3,4-dichloroisocoumarin was added for an additional 30 minutes. Proteasomes were then separated by denaturing gel electrophoresis and the binding profile was identified using autoradiography. Subunit identifications were made based on the known electrophoretic migration patterns of immunoproteasome and constitutive proteasome subunits. (C) Competitive binding experiment to determine the subunit binding profile of IPSI-001 in ANBL-6 cells. Cells were treated for 4 hours with IPSI-001, followed by addition of the VS-L3-AHx3-dansyl reagent that binds to all unoccupied catalytic subunits. Protein extracts were then separated by denaturing gel electrophoresis and probed by Western blotting using an antidansyl antibody to visualize binding patterns. Antiactin was used as a loading control and anti-β1i was used to confirm the relative position of β1i. (D) In vitro assay for the 3 major catalytic activities of the proteasome in ANBL-6 cell lysates (5 μg) exposed to increasing concentrations of IPSI-001 in triplicate. Representative data are shown as the mean plus or minus standard deviation (SD) from 3 independent experiments. *P < .05 for proteasome inhibitory activity over control. (E) Western blot analysis of the accumulation of polyubiquitinated proteasome substrates in response to 50 μM IPSI-001 treatment in ANBL-6 cells over a period of 24 hours.
To study the binding characteristics of IPSI-001, the purified constitutive proteasome and immunoproteasome, as well as ANBL-6 myeloma cells, were exposed to increasing concentrations of this inhibitor. The purified immunoproteasome was then exposed to [14C]-3,4-dichloroisocoumarin, whereas cells were exposed to vinyl-sulfone-LLL-AHx3-dansyl, both of which bind available proteasome active sites. Protein extracts were then separated by electrophoresis, and subjected either to autoradiography for the former, or to Western blotting with an antidansyl antibody for the latter. Preincubation of purified immunoproteasomes with IPSI-001 prevented subsequent binding of the radioactive probe only to subunit β1i, without an impact on β2i or β5i (Figure 1B right panel), and no binding was seen to constitutive proteasome subunits (Figure 1B left panel). Similarly, in ANBL-6 myeloma cells, which expressed a mixture of the 2 proteasome isoforms, IPSI-001 binding occurred exclusively to β1i (Figure 1C), with no binding to other immunoproteasome or constitutive proteasome subunits.
The consequences of binding of IPSI-001 to proteasome function were studied using ANBL-6 extracts and substrates specific for the ChT-L, T-L, and C-L activities. Low concentrations of IPSI-001 resulted in inhibition of the ChT-L and C-L activities, with sparing of the T-L function (Figure 1D). Increasing concentrations of IPSI-001 provided a further, dose-dependent, decrease in ChT-L activity, though a plateau was reached in C-L activity where concentrations greater than 10 μM produced little additional inhibition. Finally, inhibition of the T-L activity was seen as well, though this occurred only at some of the highest concentrations tested. To examine the impact of immunoproteasome inhibition on cellular protein turnover, Western blotting was performed to examine ubiquitin-protein conjugate levels. Consistent with a role for the immunoproteasome in housekeeping-associated proteolytic functions, IPSI-001 induced a rapid increase in conjugates at 8 hours and lasting up to 24 hours (Figure 1E).
Cytotoxic and proapoptotic impact of IPSI-001
Nonspecific proteasome inhibitors such as bortezomib and carfilzomib that target both the constitutive and immunoproteasomes inhibit cellular proliferation and induce apoptotic cell death. To assess whether inhibition of the 20Si was by itself sufficient to induce similar effects, ANBL-6 cells were exposed to IPSI-001. This reduced the viability of ANBL-6 (Figure 2A) in a dose-dependent fashion within a brief, 24-hour exposure time with a half-maximal inhibitory concentration (IC50) of 30.6 μM, compared with that of bortezomib at 7.2 nM. Reduction in viability was accompanied by the induction of apoptosis, as measured by an increased content of annexin V–positive RPMI 8226 cells (Figure 2B), and by apoptotic DNA fragmentation in ANBL-6 cells (Figure S1A, available on the Blood website; see the Supplemental Materials link at the top of the online article). IPSI-001's cytotoxic activity was compared with other proteasome inhibitors, such as epoxomicin and lactacystin, which are structurally similar to carfilzomib and NPI-0052, respectively (Figure S1B). As expected, IPSI-001 had an IC50 of 30.1 μM, whereas that of bortezomib was 5.8 nM.
Cell death and molecular changes associated with IPSI-001. (A) WST-1 cytotoxicity assay in ANBL-6 cells treated for 18 hours with bortezomib or IPSI-001. The data shown are the mean plus or minus SD from 3 independent experiments. (B) Flow cytometric analysis was performed after annexin V staining in RPMI 8226 cells treated for 24 hours with the indicated concentrations of IPSI-001, with each experiment performed in duplicate. Error bars indicate SD. *P < .05 comparing treated cells over vehicle control. (C) Representative results from 2 independent experiments of a colorimetric activity assay for caspases in RPMI 8226 myeloma cell lysate (100 μg) treated for up to 24 hours with 50 μM IPSI-001. The data shown are the mean plus or minus SD from duplicate experiments. *P < .05 for fold caspase activity over baseline. (D) Western blot analysis for the late-stage apoptotic marker PARP, where the cleaved fragment (CF) represents apoptotic cells compared with the full-length (FL) PARP, which is present in healthy, nonapoptotic ANBL-6 cells. HSC-70 levels were used as a loading control. (E) Protein expression of Bax and IκBα in RPMI 8226 cells after incubation with 50 μM IPSI-001 for 24 hours. Actin levels were used as a loading control. (F) Protein expression of phosphorylated JNK (phospho-JNK) and total JNK in RPMI 8226 cells treated with 25 or 50 μM IPSI-001 for 24 hours.
Cell death and molecular changes associated with IPSI-001. (A) WST-1 cytotoxicity assay in ANBL-6 cells treated for 18 hours with bortezomib or IPSI-001. The data shown are the mean plus or minus SD from 3 independent experiments. (B) Flow cytometric analysis was performed after annexin V staining in RPMI 8226 cells treated for 24 hours with the indicated concentrations of IPSI-001, with each experiment performed in duplicate. Error bars indicate SD. *P < .05 comparing treated cells over vehicle control. (C) Representative results from 2 independent experiments of a colorimetric activity assay for caspases in RPMI 8226 myeloma cell lysate (100 μg) treated for up to 24 hours with 50 μM IPSI-001. The data shown are the mean plus or minus SD from duplicate experiments. *P < .05 for fold caspase activity over baseline. (D) Western blot analysis for the late-stage apoptotic marker PARP, where the cleaved fragment (CF) represents apoptotic cells compared with the full-length (FL) PARP, which is present in healthy, nonapoptotic ANBL-6 cells. HSC-70 levels were used as a loading control. (E) Protein expression of Bax and IκBα in RPMI 8226 cells after incubation with 50 μM IPSI-001 for 24 hours. Actin levels were used as a loading control. (F) Protein expression of phosphorylated JNK (phospho-JNK) and total JNK in RPMI 8226 cells treated with 25 or 50 μM IPSI-001 for 24 hours.
Bortezomib and carfilzomib induce programmed cell death by activating both the intrinsic apoptotic pathway mediated by caspase-9, and the extrinsic pathway mediated by caspase-8–dependent signaling, which then converge on a common effector, caspase-3. We examined whether IPSI-001 also exerted its antiapoptotic effect through activation of intrinsic and extrinsic caspase pathways38 and found that dual caspase-8 and -9 activation was seen in a time-dependent fashion as early as after 4 hours (Figure 2C), which then induced caspase-3 activity. Other consequences of immunoproteasome inhibition included cleavage of PARP (Figure 2D), and depolarization of the trans-mitochondrial membrane potential (Figure S2).
Several mechanisms contribute to the proapoptotic effects of bortezomib, including suppression of nuclear factor kappa B by stabilization of its inhibitor IκB, accumulation of proapoptotic Bax, and activation of c-Jun N-terminal kinase (JNK).39-41 To evaluate the impact of IPSI-001 on these pathways, RPMI 8226 cells were treated with 25 or 50 μM IPSI-001. Increases in Bax and IκBα levels were observed as early as 4 hours later (Figure 2E). Similarly, activation of JNK was also seen (Figure 2F), suggesting that immunoproteasome-specific inhibitors have comparable mechanisms of action as do current nonspecific inhibitors.
Preferential activity of IPSI-001 in immunoproteasome-containing cells
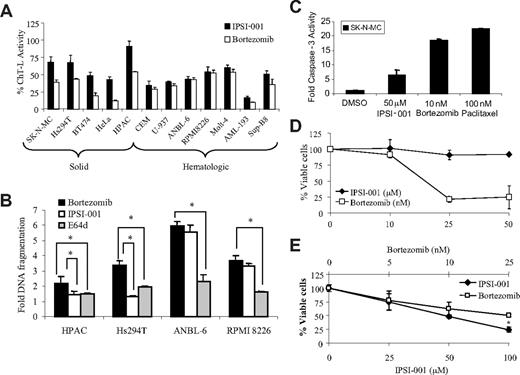
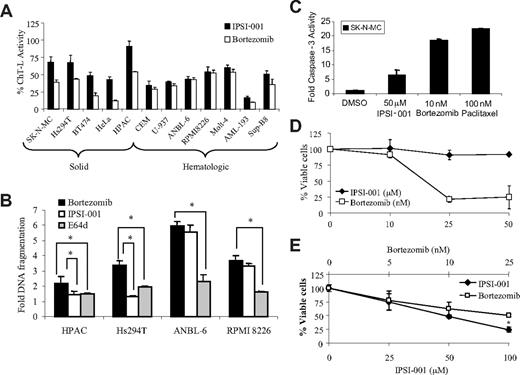
One of the promising aspects of IPSIs is that they should relatively spare cells expressing predominantly constitutive proteasomes. To evaluate this hypothesis, lysates from a panel of cell lines representing solid tumors that predominantly express 20S, and hematologic malignancies that predominantly express 20Si (Figure S3), were studied. Bortezomib at 10 nM was able to induce significant inhibition of the proteasome ChT-L activity in all of these cells (Figure 3A). When ISPI-001 was used at 50 μM, a concentration that inhibited the proteasome in hematologic cell lines to a comparable extent as bortezomib (Figure S1A), however, a lower impact on ChT-L function was seen in solid tumor cells, suggesting relative sparing of the 20S. Proapoptotic activity was then assessed in a smaller sample of 4 cell lines, including the 20Si-containing ANBL-6 and RPMI 8226 myeloma cells, as well as the 20S-containing HPAC pancreatic carcinoma and Hs294T melanoma cells. Bortezomib induced DNA fragmentation in all of these models (Figure 3B), but IPSI-001 concentrations that gave comparable levels of apoptosis in the myeloma cells induced modest, if any, cell death in the solid tumor cells. IPSI-001 is also known as calpeptin, and was originally identified as an inhibitor of the sulfhydryl calcium–activated protease calpain.42 Although the activity of calpains under conditions of normal cellular calcium concentrations is felt to be low,42 it was important to rule out the possibility that the cell death being observed was due to an impact on calpain function. Therefore, cells were also treated with E64d, a cell-permeable agent that is a 20-fold more potent and specific calpain inhibitor than IPSI-001.43 Little to no apoptosis was found in either the solid tumor or MM cell lines exposed to this agent, indicating that inhibition of calpain activity was not sufficient for apoptotic induction by IPSI-001.
IPSI-001 preferentially inhibits the proteasome and induces death in lymphoid-derived cells. (A) The ChT-L activity was measured in vitro in solid tumor (SK-N-MC, Hs294T, BT474, HeLa, and HPAC; lanes 1-5) and hematologic cancer cells (CCRF-CEM, U-937, ANBL-6, RPMI 8226, MOLT-4, AML193, and SupB8; lanes 6-12) by exposing lysates to 50 μM IPSI-001 or 10 nM bortezomib for 15 minutes, followed by incubation with the specific ChT-L activity substrate. The data shown are the mean plus or minus SD from experiments performed in triplicate. (B) HPAC pancreatic adenocarcinoma cells, Hs294T melanoma cells, and ANBL-6 and RPMI 8226 human myeloma cells were exposed to vehicle, 10 nM bortezomib, 25 μM E64d, or 50 μM IPSI-001 for 24 hours. Apoptosis was evaluated using an enzyme-linked immunosorbent assay that detects apoptotic nuclear DNA fragmentation. Cell death was expressed as the fold increase in apoptosis over the vehicle control, which was arbitrarily set at 1.0. Representative data are shown from 3 independent experiments. *P < .05 comparing the inhibitors used. (C) Human SK-N-MC cells were treated for 24 hours with the indicated agents and then cell lysates (30 μg) were measured for caspase-3 activation using a fluorogenic substrate. Representative data are shown from 2 independent experiments, each performed in triplicate, as the mean plus or minus SD. (D) Human umbilical vein endothelial cells (HUVECs) were plated until they were 70% to 80% confluent, and then treated with increasing concentrations of IPSI (μM) or bortezomib (nM) for 24 hours, followed by evaluation by WST-1 for cell viability in triplicate. The data shown are the mean plus or minus SD from experiments performed in triplicate. (E) Human peripheral blood mononuclear cells (PBMCs) were plated and exposed to IPSI-001 and bortezomib. Viable cells were assayed 24 hours later using WST-1 reagent. *P < .05 for IPSI-001 treatment compared with bortezomib.
IPSI-001 preferentially inhibits the proteasome and induces death in lymphoid-derived cells. (A) The ChT-L activity was measured in vitro in solid tumor (SK-N-MC, Hs294T, BT474, HeLa, and HPAC; lanes 1-5) and hematologic cancer cells (CCRF-CEM, U-937, ANBL-6, RPMI 8226, MOLT-4, AML193, and SupB8; lanes 6-12) by exposing lysates to 50 μM IPSI-001 or 10 nM bortezomib for 15 minutes, followed by incubation with the specific ChT-L activity substrate. The data shown are the mean plus or minus SD from experiments performed in triplicate. (B) HPAC pancreatic adenocarcinoma cells, Hs294T melanoma cells, and ANBL-6 and RPMI 8226 human myeloma cells were exposed to vehicle, 10 nM bortezomib, 25 μM E64d, or 50 μM IPSI-001 for 24 hours. Apoptosis was evaluated using an enzyme-linked immunosorbent assay that detects apoptotic nuclear DNA fragmentation. Cell death was expressed as the fold increase in apoptosis over the vehicle control, which was arbitrarily set at 1.0. Representative data are shown from 3 independent experiments. *P < .05 comparing the inhibitors used. (C) Human SK-N-MC cells were treated for 24 hours with the indicated agents and then cell lysates (30 μg) were measured for caspase-3 activation using a fluorogenic substrate. Representative data are shown from 2 independent experiments, each performed in triplicate, as the mean plus or minus SD. (D) Human umbilical vein endothelial cells (HUVECs) were plated until they were 70% to 80% confluent, and then treated with increasing concentrations of IPSI (μM) or bortezomib (nM) for 24 hours, followed by evaluation by WST-1 for cell viability in triplicate. The data shown are the mean plus or minus SD from experiments performed in triplicate. (E) Human peripheral blood mononuclear cells (PBMCs) were plated and exposed to IPSI-001 and bortezomib. Viable cells were assayed 24 hours later using WST-1 reagent. *P < .05 for IPSI-001 treatment compared with bortezomib.
Peripheral neuropathy is one toxicity of bortezomib against which there is no prophylaxis, and for which only symptomatic care and dose reduction or discontinuation is recommended. SK-N-MC cells, which are derived from an Askin tumor representing primitive neuroectodermal tissue, and are used to model neurotoxic drug effects,44-47 were studied. Bortezomib induced a significant increase in caspase-3 activity in these cells, which was comparable with that following exposure to paclitaxel, another neurotoxic drug (Figure 3C). In contrast, IPSI-001 to some extent spared SK-N-MC cells, even at concentrations that had induced almost complete inhibition of the ChT-L activity in hematologic tumor cells. This was reflected by a much lower extent of induction of caspase-3 activity by IPSI-001. Although studies have not been done to directly correlate proteasome inhibitor-mediated neurotoxicity in these cells, these data should give an indication of the probable effect in neural cells. To further assess the impact of IPSI-001 on primary cells, human umbilical vein endothelial cells (HUVECs) were treated with either bortezomib or IPSI-001. A slight decrease in the viable cell population of approximately 10% was observed in HUVECs treated with IPSI-001 at concentrations up to 50 μM (Figure 3D). However, HUVECs incubated with bortezomib had approximately 75% cell death at concentrations higher than 25 nM. Finally, IPSI-001 activity against peripheral blood mononuclear cells (PBMCs) was investigated, and a dose-dependent decrease in cellular viability was observed similar to that after bortezomib exposure (Figure 3E). Together, these findings suggest that IPSIs may have an improved toxicity profile, with a lesser impact on proteasome function and cellular viability in nonhematopoietic tissues than bortezomib, but may induce similar cytopenic effects.
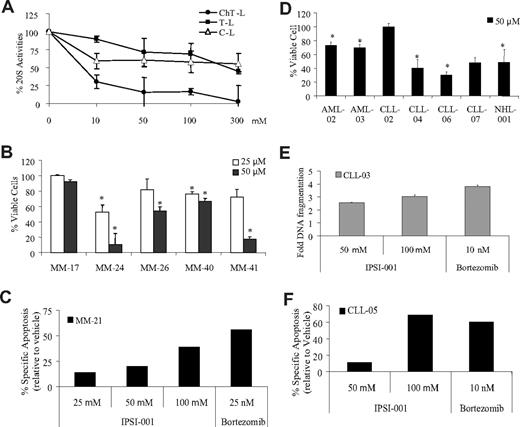
Effect of IPSI-001 in patient-derived samples
The activity of IPSI-001 against MM cell lines suggested that it could be active against primary plasma cells as well. Consistent with the previous in vitro data, IPSI-001 strongly reduced the ChT-L–like activity and modestly reduced C-L activity at low doses (Figure 4A). At higher IPSI-001 concentrations, further ChT-L inhibition was achieved, the C-L activity reached a plateau, and significant T-L inhibition was seen only at the highest drug levels. We then examined whether IPSI-001 had antiproliferative effects against purified patient plasma cells. All of the patient samples showed sensitivity to IPSI-001 treatment for 24 hours, with dose-dependent decreases in the live cell population, even in samples from patients with poor-risk disease harboring chromosome 13 deletions (Figure 4B). To confirm that this decrease was due to induction of apoptosis, flow cytometric analysis using annexin V staining was performed, and showed a dose-dependent increase in programmed cell death (Figure 4C). These experiments were performed on purified CD138+ plasma cells, and the effect of IPSI-001 on other clonal subsets of marrow-derived cells is not yet known.
Multiple myeloma and other primary samples from patients with hematologic malignancies are sensitive to IPSI-001. (A) Cellular extracts (5 μg) from CD33+ acute myeloma leukemia (AML-01) patient cells were exposed to increasing doses of IPSI-001 and proteasome inhibition was assessed using fluorogenic substrates for the ChT-L, T-L, and C-L activities of the proteasome in triplicate. These data are similar to experiments performed in 3 additional CD19+ patient samples. The data shown are the mean plus or minus SD. (B) Purified CD138+ plasma cells from patient samples were treated with 25 and 50 μM IPSI-001 for 24 hours, and the effects on cell viability were examined using the WST-1 reagent in triplicate. All of the samples are from patients with chromosome 13 deletions (MM-17, MM-24, MM-26, MM-40, and MM-41). The data shown are the mean plus or minus SD. *P < .05 compared with vehicle control. (C) Apoptosis was measured in a patient-derived bone marrow aspirate purified for CD138+ cells, which were treated for 24 hours with IPSI-001 or bortezomib, and then evaluated for programmed cell death using annexin V/TO-PRO-3 staining. (D) Purified CD19+ cells or CD33+ cells from patient samples were treated with IPSI-001 for 24 hours, and the effects on cell viability were examined using the WST-1 reagent in triplicate. The data shown are the mean plus or minus SD. *P < .05 compared with vehicle alone treatment. (E) Purified lymphocytes from a CLL patient were treated with IPSI-001 for 24 hours. Apoptosis was evaluated using an enzyme-linked immunosorbent assay that detects apoptotic nuclear DNA fragmentation in triplicate. Cell death is expressed as the fold increase in apoptosis over the vehicle control, which was arbitrarily set at 1.0. The data shown are the mean plus or minus SD. (F) Purified lymphocytes from a CLL patient were treated with IPSI-001. Annexin V–positive cells were measured using flow cytometry and results are displayed as the percentage specific apoptotic population.
Multiple myeloma and other primary samples from patients with hematologic malignancies are sensitive to IPSI-001. (A) Cellular extracts (5 μg) from CD33+ acute myeloma leukemia (AML-01) patient cells were exposed to increasing doses of IPSI-001 and proteasome inhibition was assessed using fluorogenic substrates for the ChT-L, T-L, and C-L activities of the proteasome in triplicate. These data are similar to experiments performed in 3 additional CD19+ patient samples. The data shown are the mean plus or minus SD. (B) Purified CD138+ plasma cells from patient samples were treated with 25 and 50 μM IPSI-001 for 24 hours, and the effects on cell viability were examined using the WST-1 reagent in triplicate. All of the samples are from patients with chromosome 13 deletions (MM-17, MM-24, MM-26, MM-40, and MM-41). The data shown are the mean plus or minus SD. *P < .05 compared with vehicle control. (C) Apoptosis was measured in a patient-derived bone marrow aspirate purified for CD138+ cells, which were treated for 24 hours with IPSI-001 or bortezomib, and then evaluated for programmed cell death using annexin V/TO-PRO-3 staining. (D) Purified CD19+ cells or CD33+ cells from patient samples were treated with IPSI-001 for 24 hours, and the effects on cell viability were examined using the WST-1 reagent in triplicate. The data shown are the mean plus or minus SD. *P < .05 compared with vehicle alone treatment. (E) Purified lymphocytes from a CLL patient were treated with IPSI-001 for 24 hours. Apoptosis was evaluated using an enzyme-linked immunosorbent assay that detects apoptotic nuclear DNA fragmentation in triplicate. Cell death is expressed as the fold increase in apoptosis over the vehicle control, which was arbitrarily set at 1.0. The data shown are the mean plus or minus SD. (F) Purified lymphocytes from a CLL patient were treated with IPSI-001. Annexin V–positive cells were measured using flow cytometry and results are displayed as the percentage specific apoptotic population.
In addition to activity against MM, bortezomib is preclinically active against other hematologic malignancies, so we also sought to examine the impact of IPSI-001 on other models. To that end, purified samples from patients with diffuse large B-cell non-Hodgkin lymphoma (NHL), chronic lymphocytic leukemia (CLL), and acute myeloid leukemia (AML) were treated with 50 μM IPSI-001 for 24 hours, followed by evaluations for viability (Figure 4D). All disease types showed evidence of some level of susceptibility to IPSI-001–induced cell death. One exception was a patient with prolymphocytic leukemia (CLL-02), a variant of CLL that is generally more aggressive and less responsive to treatment that, like one myeloma patient sample (MM-17, Figure 4B), showed only a slight response. As was the case for the plasma cell samples, exposure to IPSI-001 in 2 patient CLL isolates resulted in activation of apoptosis (Figure 4E,F).
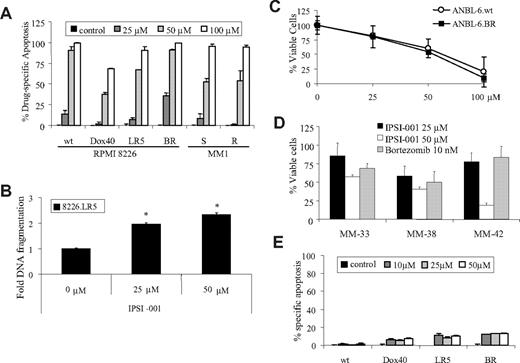
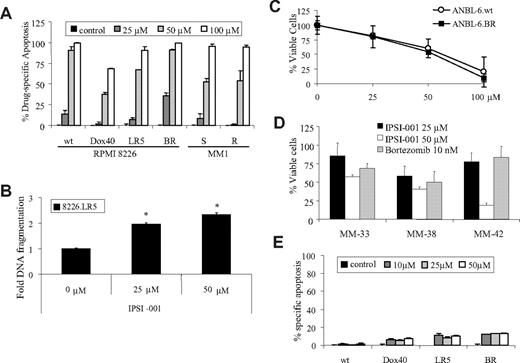
IPSI-001 overcomes chemotherapy resistance and synergizes with dexamethasone
Novel agents that can overcome chemoresistance to other drugs may have greater potential for clinical antitumor activity, and we therefore studied IPSI-001 in several drug-resistance models. RPMI 8226 wild-type cells were compared with their doxorubicin (Dox40)–resistant, melphalan (LR5)–resistant, and bortezomib-resistant (BR) counterparts, and MM1 dexamethasone-sensitive (S) cells were compared with dexamethasone-resistant (R) cells. Doxorubicin- and melphalan-resistant clones did show some decreased sensitivity to IPSI-001, especially at lower doses (Figure 5A), suggesting the possibility of some cross-resistance. However, higher concentrations of IPSI-001 induced substantial apoptosis (Figure 5A) and DNA fragmentation (Figure 5B). Dexamethasone-resistant MM1.R cells showed comparable responses to IPSI-001 as the dexamethasone-sensitive MM1.S cells (Figure 5B). Our group has also developed bortezomib-resistant (BR) myeloma cell lines that show significantly decreased sensitivity to bortezomib (Figure S4).10 Notably, and in contrast to the previous data, 8226.BR cells were even more sensitive to IPSI-001 at lower doses than their wild-type counterparts, supporting the lack of any cross-resistance. The latter possibility was also studied in the independently derived, bortezomib-resistant ANBL-6.BR cells, and compared with wild-type cell populations. Comparable decreases in viable cell populations were found in both ANBL-6.wt and ANBL-6.BR cells after exposure to IPSI-001 (Figure 5C). Importantly, plasmacytes from 3 bortezomib-refractory patients all remained sensitive to 50 μM IPSI-001 and to a higher degree than comparable 10-nM bortezomib exposure, with no significant resistance found even in MM-33, a patient with chromosome 13 deletion (Figure 5D). Lastly, to rule out the possibility that it was the ability of IPSI-001 to inhibit calpains that allowed it to overcome resistance, E64d was again used as a control. Less than 20% apoptosis was observed in all cell lines tested, including wild-type cells (Figure 5E), despite the use of inhibitor levels that were 20-fold more potent than those of IPSI-001. These findings again support the assertion that it is the ability of IPSIs to target the immunoproteasome that is responsible for their activity
IPSI-001 is able to overcome chemotherapy resistance. (A) Drug-free for at least 48 hours; doxorubicin-, melphalan-, and bortezomib-resistant RPMI 8226; and dexamethasone-sensitive and-resistant MM1 multiple myeloma cell lines were exposed to increasing doses of IPSI-001 for 24 hours in duplicate, followed by determination of apoptotic cell populations using dual annexin V/TOPRO-3 staining. The data shown are the mean plus or minus SD from 3 independent experiments. (B) Melphalan-resistant 8226.LR5 cells were treated with IPSI-001 (25 and 50 μM) for 24 hours and apoptosis was measured using a commercial kit for apoptotic DNA fragmentation. The data shown are the mean plus or minus SD. *P < .05 compared with vehicle control. (C) ANBL-6.wt and ANBL-6.BR were compared for their sensitivity to IPSI-001 after a 24-hour exposure using WST-1 proliferation assay. The data shown are the mean plus or minus SD from experiments performed in triplicate. (D) Purified CD138+ plasma cells from patient samples were treated with 25 and 50 μM IPSI-001 for 24 hours, and the effects on cell viability were examined in triplicate. Cytogenetic studies showed that MM-33 had a chromosome 13 deletion and MM-38 had a chromosome 9 deletion and trisomy 11, whereas the MM-42 sample was not evaluated. The data shown are the mean plus or minus SD. (E) RPMI 8226 cell lines resistant to doxorubicin, melphalan, and bortezomib were treated with the calpain inhibitor E64d and analyzed for annexin V staining by flow cytometry. Representative results from 2 independent experiments are shown as the mean plus or minus SD.
IPSI-001 is able to overcome chemotherapy resistance. (A) Drug-free for at least 48 hours; doxorubicin-, melphalan-, and bortezomib-resistant RPMI 8226; and dexamethasone-sensitive and-resistant MM1 multiple myeloma cell lines were exposed to increasing doses of IPSI-001 for 24 hours in duplicate, followed by determination of apoptotic cell populations using dual annexin V/TOPRO-3 staining. The data shown are the mean plus or minus SD from 3 independent experiments. (B) Melphalan-resistant 8226.LR5 cells were treated with IPSI-001 (25 and 50 μM) for 24 hours and apoptosis was measured using a commercial kit for apoptotic DNA fragmentation. The data shown are the mean plus or minus SD. *P < .05 compared with vehicle control. (C) ANBL-6.wt and ANBL-6.BR were compared for their sensitivity to IPSI-001 after a 24-hour exposure using WST-1 proliferation assay. The data shown are the mean plus or minus SD from experiments performed in triplicate. (D) Purified CD138+ plasma cells from patient samples were treated with 25 and 50 μM IPSI-001 for 24 hours, and the effects on cell viability were examined in triplicate. Cytogenetic studies showed that MM-33 had a chromosome 13 deletion and MM-38 had a chromosome 9 deletion and trisomy 11, whereas the MM-42 sample was not evaluated. The data shown are the mean plus or minus SD. (E) RPMI 8226 cell lines resistant to doxorubicin, melphalan, and bortezomib were treated with the calpain inhibitor E64d and analyzed for annexin V staining by flow cytometry. Representative results from 2 independent experiments are shown as the mean plus or minus SD.
Antimyeloma agents are often used in combinations to enhance their antitumor activity, and addition of dexamethasone to bortezomib is one strategy that has shown improved efficacy.48 To determine whether IPSI-001 works in concert with dexamethasone, ANBL-6 cells were treated simultaneously with both drugs for 48 hours. Compared with dexamethasone or IPSI-001 alone, the combination demonstrated a greater antiproliferative effect (Figure S5). Moreover, statistical analysis indicated that a moderate to high degree of synergy was present between the 2 drugs at most concentrations tested (Table S1).
Discussion
Multiple myeloma remains an incurable disease that almost invariably relapses after initial therapy, and though subsequent remissions can be achieved, they typically grow shorter with each successive line of chemotherapy.49 Although it is possible that the efficacy of proteasome inhibitors such as bortezomib is due to their lack of specificity for different proteasome isoforms, it is also likely that this broad inhibitory activity may contribute to the induction of treatment-emergent neuropathy, which can be dose limiting. This led us to consider that targeting the 20Si, which is highly expressed in hematopoietic tissues and contains 3 different proteolytic subunits compared with the constitutive proteasome, could provide efficacy with decreased toxicity. Here, we report the identification of IPSIs that relatively spare the 20S, and the characterization of IPSI-001, the most potent of these agents. IPSI-001 preferentially inhibited immunoproteasome activity in vitro and in lymphoid-derived cell lines and patient-derived samples, induced extrinsic and intrinsic pathways of apoptosis, synergized with dexamethasone, and was able to overcome conventional drug resistance, as well as resistance to bortezomib itself.
IPSI-001 was identified in a screen of peptidyl-aldehyde compounds for favored ChT-L–inhibitory activity against 20Si, and showed a 100-fold preference for this target over the comparable 20S activity (Table 1). In addition, IPSI-001 also exhibited 165-fold preference for the BrAAP activity of the 20Si, which is attributed to the β1 and β1i subunits50 (Table 1). Although the potency of IPSI-001 is not sufficient to warrant in vivo testing or translation into the clinic, its properties will be useful for further validation of the immunoproteasome as a target. Expression of 20Si has been found predominantly in immune tissues,51 but lower levels have also been noted in the brain,27 intestinal epithelium,52 liver,53 and ocular lens.54 In the latter 2, however, expression seems to be related to specific disease states leading to production of inflammatory cytokines known to induce 20Si subunits, suggesting that under normal conditions these would predominantly contain 20S. Moreover, peptide-based drugs such as bortezomib do not pass through the blood-brain barrier,55 implying that central nervous system toxicity would be unlikely with IPSIs as well. This leaves intestinal epithelium as an area of concern for toxicity based on the known expression profiles, but our studies of cell lines derived from such tissues (Figure S3) showed a predominant expression of 20S. Taken together, these findings suggest that IPSIs may indeed have a modest systemic toxicity profile, though they may well retain the hematologic toxicity of agents such as bortezomib, or perhaps even exceed it based on the increased cell death observed in PBMCs treated with IPSI-001 (Figure 3E). Once clinically relevant IPSIs are developed, therefore, it will be important to closely evaluate their tissue distribution and proteasome binding. In addition, studies correlating the level and type of immunoproteasome subunits with the impact of IPSIs will be of great help in further determining their therapeutic index.
Our lead compound, Z-Leu-nLeu-CHO, is also known as calpeptin, which inhibits calpain I and calpain II, proteases important for cell motility and cell cycle progression that play roles in necrosis and apoptosis in some cell line models.42 To rule out the possibility that calpain inhibition was responsible for the induction of apoptosis by IPSI-001 (Figure 3B), as well as its ability to overcome chemotherapy resistance (Figure 5D), we used the sulfhydryl protease inhibitor E64d as a control. These studies showed that calpain suppression was not sufficient to accomplish either of these outcomes by itself, and studies combining bortezomib with E64d showed that this approach did not overcome bortezomib resistance (not shown). In addition, some of the IPSIs we have identified are longer than dipeptides, making them less inhibitory for calpains, and these too overcome resistance (not shown). Ultimately, however, since peptidyl-aldehydes can react with free sulfhydryl groups, the role of calpain inhibition in these processes will be completely ruled out only with peptides based on other chemistries that reduce binding to sulfhydryl groups, such as boronic acids. It is also notable that recent data point to an increase in calpain activity in proteasome-inhibited cells,56 as well as in a cisplatin-resistant melanoma cell line.57 These findings suggest that IPSI-001, or other calpain inhibitors, may prove to be useful in combination therapies where the dual calpain/20Si inhibitory activity may be able to target more pathways of resistance activated by malignant cells.
The ChT-L subunit is the rate-limiting step of proteolysis by the proteasome. Kisselev et al proposed the “bite-chew” method of protein breakdown, whereby the incoming protein is cleaved at ChT-L sites (bite), and C-L sites are allosterically activated. The protein is then further degraded by the C-L and T-L sites (chew), whereas the ChT-L activity is allosterically inhibited, thus completing one cycle.58 NPI-0052 has inhibitory properties against all 3 major proteolytic activities,11 carfilzomib primarily inhibits the ChT-L activity at lower concentrations, but at higher concentrations the T-L and C-L activities are also affected,10 and bortezomib's inhibitory effect is ChT-L > C-L≫T-L. We found that IPSI-001 bound potently and specifically to the β1i subunit (Figure 1B,C) yet had an inhibitory profile similar to bortezomib (Figure 1D). Previous reports have generally attributed proteolytic activities of the 20Si catalytic subunits to their 20S counterparts, a model in which β5i should encode the ChT-L activity.21,59 Of note, Ho et al recently reported development of a β1i (LMP-2)–specific inhibitor that had greater growth inhibitory effects in cell populations with high β1i expression.60 However, the β1i-specific inhibitor developed by Ho et al was found to have ChT-L inhibitory activity, and the authors suggested that overlapping catalytic activities existed for the β1i subunit. The phenomenon of simultaneous inhibition of the ChT-L activity has been reported by 2 other groups who developed constitutive β1 inhibitors with moderate specificity whose activity was attributed to allosteric inhibition of the β5 subunit.61,62 Lastly, a report by Kisselev et al, using a highly specific β1 inhibitor, demonstrated that the dual ChT-L and C-L inhibitory properties were due to (1) the β1 inhibitor binding and inhibiting the C-L activity; (2) binding of the β1 inhibitor to a noncatalytic regulatory site that inhibits the ChT-L activity; and (3) β1 inhibitors allosterically stimulating the T-L activity.63 Given the similar inhibitory profiles of IPSI-001 and the inhibitor developed by Ho et al, we postulate that these β1i inhibitors also bind the noncatalytic, regulatory subunit proposed by Kisselev et al that is present in both 20S and 20Si proteasomes. This possibility is further supported by increased binding potential of IPSI-001 to the β1i subunit in relation to BrAAP activity (Table 1).
In general, plasma cell isolates from patients responded to exposure to IPSI-001 (Figure 4B), but in one patient sample, MM-17, a very modest effect was observed. This patient was found to have harbored disease with deletion of chromosome 13, which is a poor prognostic marker for myeloma, but one that typically responds well to bortezomib. However, deletions of chromosome 13 were also present in samples MM-24, MM-26, MM-33, MM-40, and MM-41, which did respond well. In addition, patient MM-17 had received 2 prior therapies, including bortezomib, and initially responded to therapy but had progressive disease off treatment. Three patients were clinically refractory to bortezomib at the time their cells were isolated (MM-33, MM-38, and MM-42), yet remained sensitive to IPSI-001. Interestingly, MM-33 and MM-42 had plasma cell leukemia that is typically an aggressive myeloma variant, but both responded well to IPSI-001.
In conclusion, our data indicate that the immunoproteasome is a rational target for anticancer therapy in MM. Agents based on IPSI-001, or some of the other IPSIs that have been identified, which would have enhanced potency without losing their specificity, should strongly induce apoptosis in MM and other hematologic malignancies. Moreover, they should relatively spare other tissues not expressing the immunoproteasome, unlike the current generation of nonspecific proteasome inhibitors, possibly thereby providing an improved therapeutic index. The latter could allow for more chronic dosing that could prove useful not just in cancer, but in treating other disorders such as autoimmune diseases and graft rejection that rely in part on antigen presentation that is processed through the immunoproteasome.
An Inside Blood analysis of this article appears at the front of this issue.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
R.Z.O., a Leukemia & Lymphoma Society Scholar in Clinical Research, and a Jefferson Pilot fellow in Academic Medicine, acknowledges support from the Leukemia & Lymphoma Society (White Plains, NY; 6096-07), the Multiple Myeloma Research Foundation (Norwalk, CT), the Greensboro chapter of Golfers Against Cancer (Greensboro, NC), and the National Cancer Institute (R01-CA102278). D.J.K. was supported by the American Cancer Society (Atlanta, GA; PF-07-112-01-CDD 01).
National Institutes of Health
Authorship
Contribution: D.J.K. designed and performed the majority of the research and wrote the manuscript; M.O. performed the initial screen of the peptide aldehydes and the dichloroisocoumarin competitive binding assay; S.A.H. and Q.C. helped with flow cytometric experiments; R.Z.O. and P.M.V. consented patients and obtained their samples; Q.C. and P.M.V. were essential for helping with patient sample purifications; R.Z.O. supervised all the research completed herein and offered valuable suggestions and manuscript editing.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Robert Z. Orlowski, The University of Texas M. D. Anderson Cancer Center, Department of Lymphoma and Myeloma, 1515 Holcombe Blvd, Unit 429, Houston, TX 77030-4009; e-mail: rorlowsk@mdanderson.org.

![Figure 1. IPSI-001 inhibits the immunoproteasome. (A) Chemical structure of IPSI-001. (B) Competitive binding experiment to determine subunit binding profile of IPSI-001 in purified proteasomes from bovine pituitaries (20S) and spleen (20Si). Purified proteasomes were incubated with 10 or 50 μM IPSI-001 or vehicle (Veh) for 20 minutes, and then [14C]-3,4-dichloroisocoumarin was added for an additional 30 minutes. Proteasomes were then separated by denaturing gel electrophoresis and the binding profile was identified using autoradiography. Subunit identifications were made based on the known electrophoretic migration patterns of immunoproteasome and constitutive proteasome subunits. (C) Competitive binding experiment to determine the subunit binding profile of IPSI-001 in ANBL-6 cells. Cells were treated for 4 hours with IPSI-001, followed by addition of the VS-L3-AHx3-dansyl reagent that binds to all unoccupied catalytic subunits. Protein extracts were then separated by denaturing gel electrophoresis and probed by Western blotting using an antidansyl antibody to visualize binding patterns. Antiactin was used as a loading control and anti-β1i was used to confirm the relative position of β1i. (D) In vitro assay for the 3 major catalytic activities of the proteasome in ANBL-6 cell lysates (5 μg) exposed to increasing concentrations of IPSI-001 in triplicate. Representative data are shown as the mean plus or minus standard deviation (SD) from 3 independent experiments. *P < .05 for proteasome inhibitory activity over control. (E) Western blot analysis of the accumulation of polyubiquitinated proteasome substrates in response to 50 μM IPSI-001 treatment in ANBL-6 cells over a period of 24 hours.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/113/19/10.1182_blood-2008-07-171637/7/m_zh80080931270001.jpeg?Expires=1769152897&Signature=Z7Hc9rUymifkAD87Y3y0VnTlV7fEB95jmaG81XTAe~mfKeHgM6RfEwdIUbfHAUB0pFuYv8FyDLgkAZqwgNIRuMFImatVe817NCLO~iscRdjgj50njx-0LtmdVltMFz8PjEZBB1IRNot1EQRV39RmA4WhJ3k9IOtW6NHv~d5OAzgTvoexlMYfcVNvCJpekdocJnBjhz4WgxWdCh7uHiuzI3-2jjdRKZ6fuanRqlk-sbxqT4zCv1wq~N-e0pzgd-AhzNFgBFBnoRi834mAoXFUt9zrxkaJMPjSF-wmNJgt5NExF9loP08HT5MKGUi1ma5UWPf~67aha32f5JGoFo~Y4A__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)


![Figure 1. IPSI-001 inhibits the immunoproteasome. (A) Chemical structure of IPSI-001. (B) Competitive binding experiment to determine subunit binding profile of IPSI-001 in purified proteasomes from bovine pituitaries (20S) and spleen (20Si). Purified proteasomes were incubated with 10 or 50 μM IPSI-001 or vehicle (Veh) for 20 minutes, and then [14C]-3,4-dichloroisocoumarin was added for an additional 30 minutes. Proteasomes were then separated by denaturing gel electrophoresis and the binding profile was identified using autoradiography. Subunit identifications were made based on the known electrophoretic migration patterns of immunoproteasome and constitutive proteasome subunits. (C) Competitive binding experiment to determine the subunit binding profile of IPSI-001 in ANBL-6 cells. Cells were treated for 4 hours with IPSI-001, followed by addition of the VS-L3-AHx3-dansyl reagent that binds to all unoccupied catalytic subunits. Protein extracts were then separated by denaturing gel electrophoresis and probed by Western blotting using an antidansyl antibody to visualize binding patterns. Antiactin was used as a loading control and anti-β1i was used to confirm the relative position of β1i. (D) In vitro assay for the 3 major catalytic activities of the proteasome in ANBL-6 cell lysates (5 μg) exposed to increasing concentrations of IPSI-001 in triplicate. Representative data are shown as the mean plus or minus standard deviation (SD) from 3 independent experiments. *P < .05 for proteasome inhibitory activity over control. (E) Western blot analysis of the accumulation of polyubiquitinated proteasome substrates in response to 50 μM IPSI-001 treatment in ANBL-6 cells over a period of 24 hours.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/113/19/10.1182_blood-2008-07-171637/7/m_zh80080931270001.jpeg?Expires=1769532989&Signature=3UF26ejYJNHaSfjRlDMYZSAVWfF6Y492oQ5kKYxIcIw1gBmeXhn8R0Jf8JB4CslP3C55Z9mcgCHddXlaSPfxdiKS06x9pSAvlLgUELea9ADR976iqtQvRK9nZOOrRrWrph0g4SX5kVYbJbmKcWTYSfBWx3o581NdbWUbt670Dmn2PtiOpQ6XPXLACBAuSzzSWWO4MpAmJcNE4C-I~aOX8KI6F7E0OmMpsYYqWpWshe6W-UE6kxq4K3ifwL~zM4T9b5OEzZelm1QlsysdO8qWSWkXB7zpaGsfxXbY0-b8ThkD21FOoESf8ILJiCfy3CF1Zzrocl7b6SvXgn2Wtkmvpg__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)