Adhesive interactions between multiple myeloma (MM) cells and marrow stromal cells activate multiple signaling pathways including nuclear factor κB (NF-κB), p38 mitogen-activated protein kinase (MAPK), and Jun N-terminal kinase (JNK) in stromal cells, which promote tumor growth and bone destruction. Sequestosome-1 (p62), an adapter protein that has no intrinsic enzymatic activity, serves as a platform to facilitate formation of signaling complexes for these pathways. Therefore, we determined if targeting only p62 would inhibit multiple signaling pathways activated in the MM microenvironment and thereby decrease MM cell growth and osteoclast formation. Signaling through NF-κB and p38 MAPK was increased in primary stromal cells from MM patients. Increased interleukin-6 (IL-6) production by MM stromal cells was p38 MAPK-dependent while increased vascular cell adhesion molecule-1 (VCAM-1) expression was NF-κB–dependent. Knocking-down p62 in patient-derived stromal cells significantly decreased protein kinase Cζ (PKCζ), VCAM-1, and IL-6 levels as well as decreased stromal cell support of MM cell growth. Similarly, marrow stromal cells from p62−/− mice produced much lower levels of IL-6, tumor necrosis factor-α (TNF-α), and receptor activator of NF-κB ligand (RANKL) and supported MM cell growth and osteoclast formation to a much lower extent than normal cells. Thus, p62 is an attractive therapeutic target for MM.
Introduction
Marrow stromal cells in the bone microenvironment of multiple myeloma (MM) patients play a critical role in promoting both tumor growth and bone destruction.1,–3 Binding of MM cells to marrow stromal cells, through vascular cell adhesion molecule-1 (VCAM-1) on stromal cells and α4β1 integrin on MM cells,4,–6 results in increased production of tumor necrosis factor-α (TNF-α),7 receptor activator of nuclear factor κB (NF-κB) ligand (RANKL), and interleukin-6 (IL-6) by marrow stromal cells.7,8 These factors in turn increase both osteoclast (OCL) formation9 and the growth of MM cells. Adhesive interactions between MM cells and marrow stromal cells also decrease the sensitivity of MM cells to chemotherapeutic agents.10,,–13 Many of the downstream effects of these adhesive interactions are mediated through the NF-κB, p38 mitogen-activated protein kinase (MAPK), and Jun N-terminal kinase (JNK) signaling pathways. Sequestosome-1 (p62) is a common component of these signaling pathways and is as an adapter protein that has no intrinsic enzyme activity but serves as a platform to facilitate formation of signaling complexes that activate NF-κB, p38 MAPK, and JNK. It is our hypothesis that targeting p62 in marrow stromal cells should affect multiple signaling pathways simultaneously and impair their capacity to promote the growth of MM cells and OCL formation. Thus, p62 may be an attractive therapeutic target for MM.
In this report, we demonstrate that p38 MAPK and NF-κB signaling are increased in primary marrow stromal cells from MM patients and that knocking-down p62 results in a marked reduction in the capacity of stromal cells to support the growth of MM cells and OCL formation due to the much lower levels of VCAM-1, TNF-α, IL-6, and RANKL expressed by stromal cells.
Methods
Reagents
Fetal bovine serum (FBS) was purchased from GIBCO-BRL (Grand Island, NY). Recombinant human TNF-α, soluble RANKL, and macrophage colony-stimulating factor (M-CSF); mouse TNF-α, mIL-6, and hIL-6 enzyme-linked immunosorbent assay (ELISA) kits were obtained from R&D Systems (Minneapolis, MN). A p38 MAPK inhibitor, SB203580, and the NF-κB inhibitor, NEMO (NF-κB essential modulator; IKKα) binding domain binding peptide, were purchased from Calbiochem (San Diego, CA).
Primary marrow stromal cell cultures
After informed consent was obtained in accordance with the Declaration of Helsinki, bone marrow aspirates were collected in heparin from 11 healthy and 13 patients with MM. These studies were approved by the University of Pittsburgh Institutional Review Board. Marrow mononuclear cells (MNCs) were separated by Ficoll-Hypaque density sedimentation, and were cultured in long-term Dexter-type marrow cultures to obtain marrow stromal cells.14 Briefly, 107 bone marrow cells were incubated in Iscove modified Dulbecco medium (IMDM) with 10% fetal calf serum (FCS) in 10-cm tissue culture dishes, and after 1 day, the nonadherent cells were removed. The cultures were then continued for 21 days. Media were replaced with fresh media every 4 days. At subconfluence, cells were detached with trypsin and plated at a density of 105 cells/10-cm dish and were used at passages 2 to 3.
Myeloma cell lines
p62 knockdown in primary stromal cells
Primary human bone marrow stromal cells and the KM101 human stromal cell line were transfected with 10 μg p62 small interfering RNA (siRNA, sc-29 679; Santa Cruz Biotechnology, Santa Cruz, CA) or scrambled siRNA (sc-37 007; Santa Cruz Biotechnology) using the siRNA Transfection Reagent (sc-29 528; Santa Cruz Biotechnology). Forty-eight hours later, Western blot analysis and reverse transcription polymerase chain reaction (RT-PCR) analysis for p62 protein and mRNA were performed using anti-p62 (BD Biosciences, Franklin Lakes, NJ) and p62-specific primers. The gene-specific primers for p62 were 5′-AAGCCGGGTGGGAATGTTG-3′ (sense) and 5′-GCTTGGCCCTTCGGATTCT-3′ (antisense).
Coculture of primary human bone marrow stromal cells with myeloma cell lines
p62 siRNA or control siRNA transfected primary human bone marrow stromal cells (104/well in 12-well plates or 2 × 103/well in 96-well plates) and MM1.S or ANBL-6 cells (3 × 104/well in 12-well plates or 6 × 103/well in 96-well plates) were cocultured in RPMI plus 10% FBS for 3 days. MM1.S and ANBL-6 cells from 12-well plates were harvested by pipeting and counted using a hemocytometer. Supernatants from 96-well plates were collected and assayed for IL-6 by ELISA.
p62−/− mice
Mice genetically deficient for p62 (p62−/−) were produced as described by Shin17 and maintained on a C57BL/6 background using standard procedures. Animal handling protocols were approved by the Institutional Animal Care and Use Committee (IACUC) at Virginia Commonwealth University.
For all studies, experimental animals were produced from matings that yielded both homozygous knockout and heterozygous offspring. The heterozygous littermates were used as the control animals. Marrow and spleen were isolated from p62−/− mice and p62+/− littermate mice as described in the next section.18
Isolation of p62+/− and p62−/− stromal cells and coculture with CFU-blast derived OCL precursors
Marrow cells from p62−/− or p62+/− littermates were harvested and used to establish long-term Dexter-type marrow cultures. Briefly, 107 marrow cells were incubated in IMDM with 10% FCS in T-25 tissue culture flasks. At the end of 3 weeks of culture, the nonadherent cells were removed, and the adherent cells used as a source of marrow stromal cells. p62+/− spleen cell–derived OCL precursors prepared as described above19,20 were then cocultured with marrow stromal cells from the p62−/− or p62+/− littermates. Cultures were treated with TNF-α, and OCL formation assessed by counting the number of tartrate-resistant acid phosphatase (TRAP)–positive multinucleated cells formed after 9 days of culture. As part of these experiments, RANKL production was determined in stromal cell cultures treated with TNF-α using an ELISA kit for murine RANKL (R&D Systems).
Coculture of murine marrow stromal cells with human myeloma cells
Stromal cells (3 × 103 cells/well in 96-well plates) from p62−/− or p62+/− littermates derived as described in “Coculture of primary human bone marrow stromal cells with myeloma cell lines”21 were cocultured with green fluorescent protein (GFP)-labeled human myeloma MM1.S cells (6 × 104 cells/well) for 3 days. MM cells were counted by fluorescence microscopy. At the end of culture, murine IL-6 and TNF-α production were determined in the conditioned media using ELISA kits (R&D Systems).
Fluorescence-activated cell sorting analysis
Primary human bone marrow stromal cells were trypsinized and incubated with fluorescein isothiocyanate (FITC)–conjugated anti-CD14 (monocyte marker), FITC or phycoerythrin (PE) anti-CD51 (endothelial cell marker), FITC anti-CD63 (lymphocyte marker), PE anti-CD45, and FITC-CD138 (all from BD Biosciences, San Jose, CA) as previously described.22 Cells were analyzed on a FACSCalibur flow cytometer (BD Biosciences) using WinMDI software (Joseph Trotter, Scripps Research Institute, La Jolla, CA).
Western blot analysis and ELISA
Equal amounts of cell lysate from marrow stromal cells (15 μg) were subjected to 7.5 or 10% sodium dodecyl sulfate polyacrylamide gel electrophoresis (SDS-PAGE) under reducing conditions on precast gels (Bio-Rad Laboratories, Hercules, CA). Separated proteins were transferred to nitrocellulose membranes, and the nonspecific sites blocked with 5% bovine serum albumin (BSA) in 50 mM Tris-buffered saline (TBS; pH 7.6) containing 0.05% Tween 20 (TBST). Blots were incubated overnight at 4°C with optimally diluted primary antibodies followed by washing and incubation with horseradish peroxidase (HRP)–conjugated secondary antibodies (Cell Signaling, Danvers, MA) for 1 hour at room temperature. The antibodies used for immunoblotting included the following: anti-p62, anti–VCAM-1 (Santa Cruz Biotechnology), antiphosphorylated PKCζ, anti-PKCζ, antiphosphorylated IκBα, anti-IκBα, antiphosphorylated p38 MAPK (Thr180/Tyr182), anti-p38 MAPK, anti phosphorylated NF-κB, anti–NF-κB, antiphosphorylated IKKγ, anti-IKKγ (all from Cell Signaling), as well as anti–β-actin (Sigma-Aldrich, St Louis, MO). The blots were washed and visualized by an Immobilon Western chemiluminescent detection system (Millipore, Billerica, MA). The membranes were stripped and reprobed for β-actin to ensure equal loading.
Statistical analysis
Significance was evaluated using a 2-sided, unpaired Student t test, with P less than .05 considered significant.
Results
Characterization of marrow stromal cells from healthy patients and those with MM
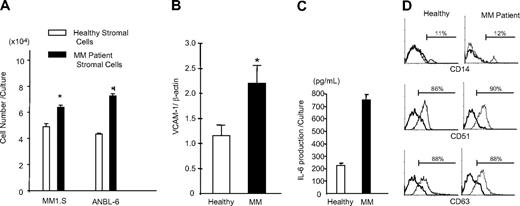
Marrow stromal cells play an important role in supporting MM cell growth, OCL formation, and also increase the resistance of MM cells to chemotherapeutic agents.2 However, it is unclear if marrow stromal cells from MM patients differ from healthy patients, and if so, whether these differences persist once marrow stromal cells are no longer in contact with MM cells. To test for differences in stromal cells from myeloma patients and healthy subjects, we used Dexter marrow cultures to enrich stromal cells from marrow adherent cells. Table 1 lists the characteristics of the 13 MM patients used in these studies. CD138+ cells and CD138+ mRNA were not detectable by FACS analysis or PCR after 3 weeks in the Dexter marrow cultures used to generate stromal cells, even though MM cells from these patients are CD138+ (data not shown). Further, when MM1.S or ANBL6 cells were cocultured for 72 hours with MM or normal stromal cells, the growth of both MM cell lines was significantly increased in cultures containing MM stromal cells compared with cocultures containing normal stromal cells (Figure 1A). MM1.S cells are IL-6–independent, and ANBL6 are IL-6–dependent MM cells. Primary marrow stromal cells from MM patients and healthy patients differed in several aspects. Primary marrow stromal cells from MM patients expressed significantly higher levels of VCAM-1 (2-fold) and IL-6 (3-fold) than normal stromal cells (Figure 1B,C).
Characterization of myeloma (MM) stromal cells. (A) Stromal cells from patients with MM or healthy subjects were cocultured with the MM1.S or ANBL-6 MM cell line for 3 days. MM cell growth was determined by counting MM cells after removing the MM cells by vigorously pipeting. *P < .05 compared with normal. (B) The levels of VCAM-1 expression in primary normal and myeloma-derived stromal cells from 13 MM patients and 11 healthy controls were determined by Western blot analysis as described in “Methods.” The ratio of VCAM-1 to β-actin was compared by densitometry. Results are presented as mean (± SEM). *P < .05 compared with normals. (C) IL-6 production in the same samples was determined by ELISA. (D) FACS analysis of MM and normal stromal cells. Bone marrow mononuclear cells from patients and healthy subjects were cultured at 106/mL in IMDM plus 10% FCS. After 3 days in culture, nonadherent cells were removed, and the media was replaced. The cultures were fed 2 times a week until confluence or 21 days. Stromal cells were detached using trypsin and counted using trypan blue exclusion, and the presence of residual MM cells determined by CD138 staining. The stromal cells were then cultured at 103 cells/cm2 under the same conditions for 3 days and used for each experiment. Cells (104) were incubated with the specific antibody for 15 minutes, and the percentage of positive cells were determined by FACS. Similar FACS results were seen in experiments using stromal cells from 3 different patients and healthy subjects.
Characterization of myeloma (MM) stromal cells. (A) Stromal cells from patients with MM or healthy subjects were cocultured with the MM1.S or ANBL-6 MM cell line for 3 days. MM cell growth was determined by counting MM cells after removing the MM cells by vigorously pipeting. *P < .05 compared with normal. (B) The levels of VCAM-1 expression in primary normal and myeloma-derived stromal cells from 13 MM patients and 11 healthy controls were determined by Western blot analysis as described in “Methods.” The ratio of VCAM-1 to β-actin was compared by densitometry. Results are presented as mean (± SEM). *P < .05 compared with normals. (C) IL-6 production in the same samples was determined by ELISA. (D) FACS analysis of MM and normal stromal cells. Bone marrow mononuclear cells from patients and healthy subjects were cultured at 106/mL in IMDM plus 10% FCS. After 3 days in culture, nonadherent cells were removed, and the media was replaced. The cultures were fed 2 times a week until confluence or 21 days. Stromal cells were detached using trypsin and counted using trypan blue exclusion, and the presence of residual MM cells determined by CD138 staining. The stromal cells were then cultured at 103 cells/cm2 under the same conditions for 3 days and used for each experiment. Cells (104) were incubated with the specific antibody for 15 minutes, and the percentage of positive cells were determined by FACS. Similar FACS results were seen in experiments using stromal cells from 3 different patients and healthy subjects.
Because marrow stromal cells are a heterogenous cell population and comprise fibroblast-like cells, macrophages, and endothelial cells, we next determined if the differences between MM patient-derived and normal stromal cells were due to a change in the distribution of cell types present in the stromal cell preparations, such as enrichment or loss of a particular cell type that affected the capacity of the stromal cell preparations to stimulate the growth of MM cells. Both MM and normal stromal cells contained similar percentages of cells that expressed CD63 (88.5 ± 1.4 vs 88.4 ± 1.8, mean ± standard deviation [SD] for healthy vs MM patients, n = 5) and CD51 (86 ± 0.5 vs 90 ± 3, mean ± SD for healthy vs MM patients, n = 5)23,24 and that had low expression of CD14 (11 ± 1 vs 12 ± 0.3, mean ± SD for healthy vs MM patients, n = 5; Figure 1D). The hematopoietic cell marker for the monocyte lineage (CD11b) was not detected in either stromal cell preparation (data not shown).
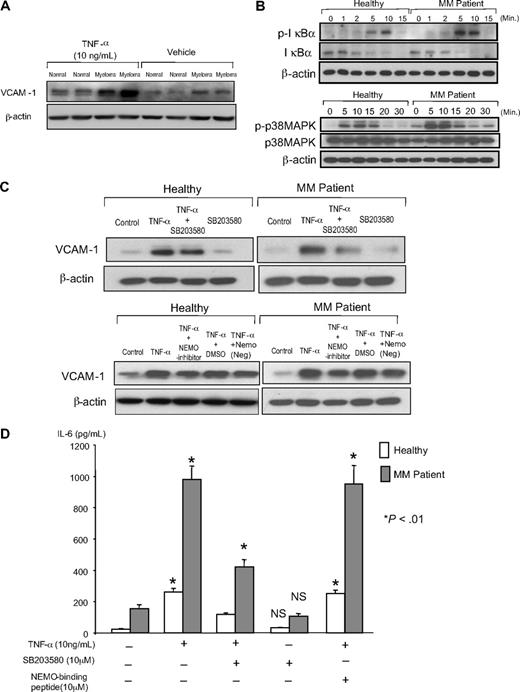
We then determined if MM stromal cells were more responsive to stimuli such as TNF-α, which is increased in the bone marrow microenvironment of MM patients. As shown in Figure 2, marrow stromal cells from MM patients had increased VCAM-1 and IL-6 expression levels compared with normal stromal cells both at baseline and when treated with TNF-α (Figures 2A,D). As shown in Figure 2C, when MM marrow stromal cells were treated with TNF-α, VCAM-1 expression was increased approximately 6-fold. In contrast, TNF-α increased VCAM-1 expression approximately 4-fold in normal marrow stromal cells. When results from 7 patients and 7 healthy subjects were compared, TNF-α increased VCAM-1 levels in MM vs normal stromal cells 1.55 ± 0.18-fold (mean ± SD P < .05). We then determined the contribution of the NF-κB and p38 MAPK signaling pathways to the increased VCAM-1 and IL-6 expression by TNF-α treated stromal cells. For these experiments, the cells were serum-starved and then treated with TNF-α. Both NF-κB and p38 MAPK signaling were increased in normal and MM stromal cells in response to TNF-α, but signaling was increased to a greater extent in MM stromal cells compared with normal cells (Figure 2B). Inhibiting NF-κB activation with a NEMO binding inhibitor decreased VCAM-1 expression by 50% in normal and MM stromal cells, but had no effect on IL-6 expression induced by TNF-α (Figure 2C,D). In contrast, inhibiting p38 MAPK signaling significantly decreased IL-6 production and slightly decreased VCAM-1 expression in both normal and MM stromal cells.
VCAM-1 expression, IL-6 production, and downstream signaling of NF-κB and p38 MAPK by stromal cells from MM patients and healthy subjects. (A) Stromal cells from healthy and MM patients were cultured with 10 ng/mL TNF-α for 4 days, the cell lysates were collected, and the levels of VCAM-1 were determined by Western blot analysis using anti–VCAM-1 antibody. Densitometry readings were all compared with healthy patient 1 untreated stromal cells. (B) Activation of downstream signaling pathways in normal or MM stromal cells induced by TNF-α. Stromal cells (5 × 104 cells/well) from healthy subjects and MM patients were cultured with 10% FCS in IMDM for 14 days. Cells were then cultured with 2% FCS in IMDM for 24 hours as a means of starvation. After starvation, cells were exposed to TNF-α (10 ng/mL) for the indicated times. Cells were lysed, fractionated by SDS-PAGE, and analyzed by immunoblot using antibodies recognizing phosphorylated and total signaling molecules of IκBα and p38 MAPK. β-Actin served as the loading control. (C) NEMO inhibitor but not p38 inhibitor decreases TNF-α–induced VCAM-1 expression in MM stromal cells. Stromal cells from MM patients were cultured for 4 days with TNF-α in the presence or absence of 10 μM NEMO inhibitor or 10 μM of a p38 MAPK inhibitor (SB203580). The cell lysates were collected and analyzed by Western blot analysis using anti–mouse VCAM-1. Densitometry reading for healthy subjects and MM patients were compared independently to their relevant MM or normal controls. (D) IL-6 production from MM stromal cells was blocked by the p38 MAPK inhibitor. Stromal cells from MM patients were cultured for 4 days with TNF-α and/or NEMO and p38 MAPK inhibitors. The culture media were collected, and IL-6 was measured with an IL-6 ELISA kit. *P < .01 compared from TNF-α alone. NS indicates not significantly different from vehicle treated cells. Similar results were seen in 6 independent experiments using MM and normal derived primary stromal cell samples.
VCAM-1 expression, IL-6 production, and downstream signaling of NF-κB and p38 MAPK by stromal cells from MM patients and healthy subjects. (A) Stromal cells from healthy and MM patients were cultured with 10 ng/mL TNF-α for 4 days, the cell lysates were collected, and the levels of VCAM-1 were determined by Western blot analysis using anti–VCAM-1 antibody. Densitometry readings were all compared with healthy patient 1 untreated stromal cells. (B) Activation of downstream signaling pathways in normal or MM stromal cells induced by TNF-α. Stromal cells (5 × 104 cells/well) from healthy subjects and MM patients were cultured with 10% FCS in IMDM for 14 days. Cells were then cultured with 2% FCS in IMDM for 24 hours as a means of starvation. After starvation, cells were exposed to TNF-α (10 ng/mL) for the indicated times. Cells were lysed, fractionated by SDS-PAGE, and analyzed by immunoblot using antibodies recognizing phosphorylated and total signaling molecules of IκBα and p38 MAPK. β-Actin served as the loading control. (C) NEMO inhibitor but not p38 inhibitor decreases TNF-α–induced VCAM-1 expression in MM stromal cells. Stromal cells from MM patients were cultured for 4 days with TNF-α in the presence or absence of 10 μM NEMO inhibitor or 10 μM of a p38 MAPK inhibitor (SB203580). The cell lysates were collected and analyzed by Western blot analysis using anti–mouse VCAM-1. Densitometry reading for healthy subjects and MM patients were compared independently to their relevant MM or normal controls. (D) IL-6 production from MM stromal cells was blocked by the p38 MAPK inhibitor. Stromal cells from MM patients were cultured for 4 days with TNF-α and/or NEMO and p38 MAPK inhibitors. The culture media were collected, and IL-6 was measured with an IL-6 ELISA kit. *P < .01 compared from TNF-α alone. NS indicates not significantly different from vehicle treated cells. Similar results were seen in 6 independent experiments using MM and normal derived primary stromal cell samples.
Role of p62 in the activated signaling in marrow stromal cells from MM patients
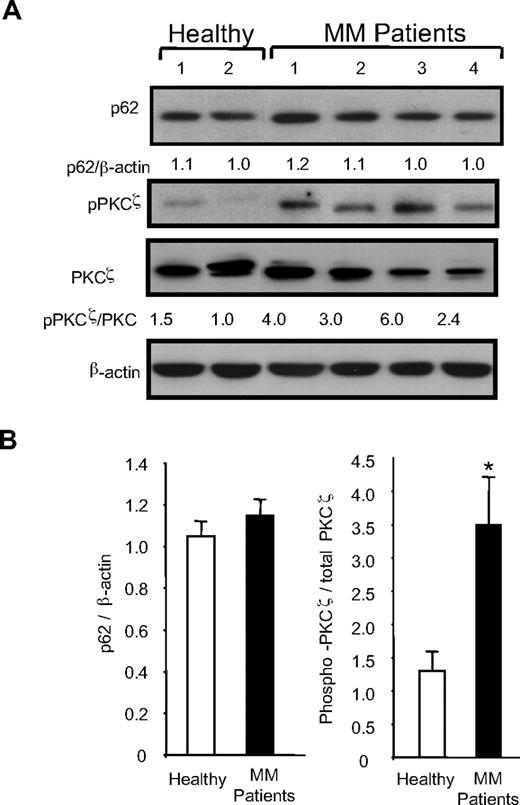
Stromal cells from MM patients have increased NF-κB and p38 MAPK signaling, and p62 is a common component that serves as a platform for formation of these signaling complexes. However, the effects of targeting p62 on these signaling pathways in MM are unknown. Therefore, we measured p62 and PKCζ levels in stromal cells from 13 MM patients and 11 healthy controls by Western blot analysis and determined the effects of siRNA knockdown of p62 in stromal cells on p38 MAPK and NF-κB signaling. We measured PKCζ and phospho-PKCζ levels, because p62 specifically binds PKCζ, which is then activated by phosphorylation. For these experiments, stromal cells were exposed to 10% (vol/vol) FBS for 10 minutes after 12 hours of serum starvation, and then p62 levels, phosphorylation of PKCζ, and total PKC levels were measured by Western blot analysis. As shown in Figure 3A and B, significantly elevated ratios of phosho-PKCζ to total PKCζ (2- to 6-fold) were detected in stromal cells from MM patients compared with healthy cells although the levels varied greatly among the individual patients. In contrast, p62 protein levels in stromal cells from MM patients and healthy patients were similar (Figure 3B).
p62, phospho-PKCζ/PKCζ, and VCAM-1 expression in MM stromal cells. Stromal cells (1°) from 13 patients and 11 healthy controls were cultured in 12-well plates for 3 days, and an aliquot of each sample was serum-starved for 12 hours and then exposed to serum for 10 minutes at the end of culture period. Levels of pPKC-ζ were determined in serum-starved samples, while PKCζ, actin, and p62 were determined in the matched unstarved samples by Western blot analysis as described in “Methods.” Equal amounts of protein were loaded in all lanes. (A) Typical results for PKCζ phosphorylation and p62 for 4 MM patients and 2 healthy subjects are shown. The relative levels were compared with healthy patient 2, who expressed the lowest level of p62 and pPKCζ. The black marks reflect splicing of the results to group normal and myeloma subjects together, specifically normal 2 was moved next to normal 1 for the pPKCζ blot. (B) The ratio of p62 and phospho-PKCζ/PKCζ in MM compared with normal stromal cells for 13 MM patients and 11 healthy subjects. Results represent the mean (± SEM). *P < .01.
p62, phospho-PKCζ/PKCζ, and VCAM-1 expression in MM stromal cells. Stromal cells (1°) from 13 patients and 11 healthy controls were cultured in 12-well plates for 3 days, and an aliquot of each sample was serum-starved for 12 hours and then exposed to serum for 10 minutes at the end of culture period. Levels of pPKC-ζ were determined in serum-starved samples, while PKCζ, actin, and p62 were determined in the matched unstarved samples by Western blot analysis as described in “Methods.” Equal amounts of protein were loaded in all lanes. (A) Typical results for PKCζ phosphorylation and p62 for 4 MM patients and 2 healthy subjects are shown. The relative levels were compared with healthy patient 2, who expressed the lowest level of p62 and pPKCζ. The black marks reflect splicing of the results to group normal and myeloma subjects together, specifically normal 2 was moved next to normal 1 for the pPKCζ blot. (B) The ratio of p62 and phospho-PKCζ/PKCζ in MM compared with normal stromal cells for 13 MM patients and 11 healthy subjects. Results represent the mean (± SEM). *P < .01.
We then assessed the effects of knock-down of p62 in human marrow stromal cells. p62 siRNA (1-10 μg) was transfected into primary human myeloma-derived stromal cells and the KM101 human stromal cell line using a commercial transfection reagent. We confirmed that p62 expression was decreased by 60% and 90% at the mRNA and protein level, respectively, in these stromal cells by real-time PCR and Western blot analysis using an anti-p62 antibody (Figure S1, available on the Blood website; see the Supplemental Materials link at the top of the online article.).
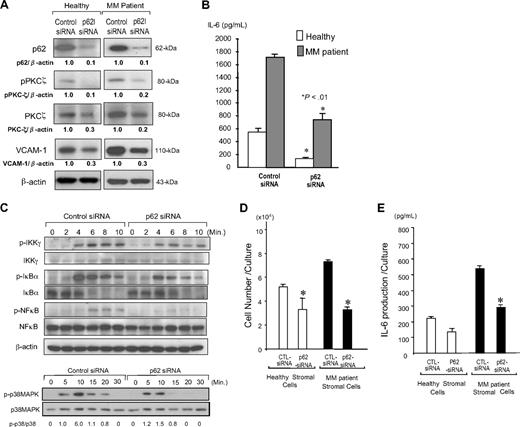
PKCζ and VCAM-1 expression were decreased by at least 70% in p62 siRNA transduced MM and normal stromal cells compared with control siRNA transduced cells (Figure 4A). IL-6 production by p62 siRNA transfected normal and MM-derived stromal cells was also significantly decreased compared with scrambled siRNA or untreated cells (Figure 4B). Further, knocking-down p62 in primary MM stromal cells treated with TNF-α markedly decreased NF-κB and p38 MAPK signaling compared with control siRNA treated cells (Figure 4C).
Effects of knockdown of p62 in marrow stromal cells. (A) p62 siRNA or control RNA transduced normal or MM stromal cells were cultured for 3 days, serum-starved for 24 hours and then exposed to serum for 10 minutes, and the cell lysates from the stromal cells were collected. Western blot analysis was performed using anti-p62 (BD Biosciences), anti–phosho-PKCζ, anti-PKCζ, and anti-VCAM-1, and the relative levels compared with the appropriate control were determined by densitometry. (B) IL-6 concentrations in culture media were measured after 3 days of culture by IL-6 ELISA assay kit. (C) Activation of downstream signaling pathways in p62 siRNA transduced MM stromal cells induced by TNF-α. p62 siRNA or control RNA transduced MM stromal cells (5 × 104 cells/well) were cultured with 10% FCS in IMDM for 2 days. Cells were then cultured with 2% FCS in IMDM for 24 hours as a means of starvation. After starvation, cells were exposed to TNF-α (10 ng/mL) for the indicated times. Cells were lysed, fractionated by SDS-PAGE, and analyzed by immunoblot using antibodies recognizing phosphorylated and total signaling molecules of IκBα, NF-κB, and p38 MAPK. β-Actin served as the loading control. All antibodies were purchased from Cell Signaling. (D) p62 siRNA (0-10 mg) or control siRNA transduced normal or myeloma-derived stromal cells were cocultured with the ANBL-6 MM cell line for 3 days. MM cell growth was determined by counting CD138+ MM cells after removing the MM cells by vigorously pipeting. (E) Stromal cells were cocultured with ANBL-6 as described in “Methods.” The conditioned media were collected after 3 days, and the IL-6 concentrations were measured by ELISA kit. Similar results were seen in 3 independent experiments.
Effects of knockdown of p62 in marrow stromal cells. (A) p62 siRNA or control RNA transduced normal or MM stromal cells were cultured for 3 days, serum-starved for 24 hours and then exposed to serum for 10 minutes, and the cell lysates from the stromal cells were collected. Western blot analysis was performed using anti-p62 (BD Biosciences), anti–phosho-PKCζ, anti-PKCζ, and anti-VCAM-1, and the relative levels compared with the appropriate control were determined by densitometry. (B) IL-6 concentrations in culture media were measured after 3 days of culture by IL-6 ELISA assay kit. (C) Activation of downstream signaling pathways in p62 siRNA transduced MM stromal cells induced by TNF-α. p62 siRNA or control RNA transduced MM stromal cells (5 × 104 cells/well) were cultured with 10% FCS in IMDM for 2 days. Cells were then cultured with 2% FCS in IMDM for 24 hours as a means of starvation. After starvation, cells were exposed to TNF-α (10 ng/mL) for the indicated times. Cells were lysed, fractionated by SDS-PAGE, and analyzed by immunoblot using antibodies recognizing phosphorylated and total signaling molecules of IκBα, NF-κB, and p38 MAPK. β-Actin served as the loading control. All antibodies were purchased from Cell Signaling. (D) p62 siRNA (0-10 mg) or control siRNA transduced normal or myeloma-derived stromal cells were cocultured with the ANBL-6 MM cell line for 3 days. MM cell growth was determined by counting CD138+ MM cells after removing the MM cells by vigorously pipeting. (E) Stromal cells were cocultured with ANBL-6 as described in “Methods.” The conditioned media were collected after 3 days, and the IL-6 concentrations were measured by ELISA kit. Similar results were seen in 3 independent experiments.
We then examined the effects of knock-down of p62 in MM patient-derived and normal stromal cells on the growth of ANBL6 MM cells. As shown in Figure 4D, loss of signaling through p62 significantly decreased stromal cell support of MM cell growth and reduced MM-derived stromal cell support of MM cell growth to normal levels. Similarly, knockdown of p62 significantly blunted the increased IL-6 production in cocultures of MM-derived stromal cells with MM cells compared with MM cells cocultured with normal stromal cells (Figure 4E).
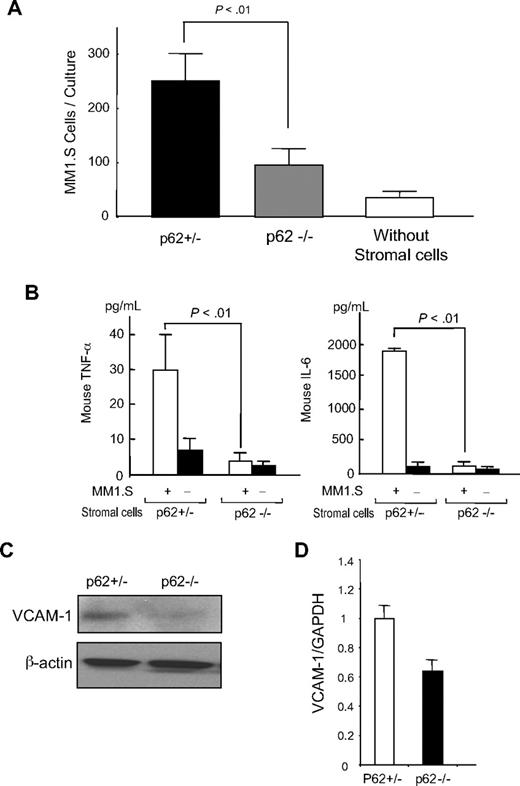
To further characterize the contribution p62 makes to the capacity of marrow stromal cells to increase MM cell growth and OCL formation, we tested marrow stromal cells from p62−/− mice for their capacity to support MM cell growth and produce IL-6 and TNF-α in response to the MM1.S human MM cell line. We used GFP-labeled MM1.S cells to allow identification of MM cells by fluorescence microscopy and murine stromal cells to distinguish cytokines produced by the stromal cells from those produced by the MM cells. We have previously reported that murine stromal cells can enhance the growth of human MM cells such as MM1.S.25 As shown in Figure 5A, the growth of human MM cells was significantly lower when MM cells were cocultured with p62−/− stromal cells compared with p62+/− stromal cells. Further, in contrast to p62+/− stromal cells, which produced high levels of IL-6 and TNF-α when cocultured with human MM cells, IL-6 and TNF-α production by p62−/− stromal cells were not significantly increased in response to MM cells (Figure 5B). Similarly, basal VCAM-1 expression was significantly reduced in p62−/− stromal cells compared with p62+/− stromal cells (Figure 5C). When p62−/− bone marrow stromal cells were then cocultured with MM1.S cells, VCAM-1 mRNA levels were significantly reduced compared with cocultures with p62+/− stromal cells (Figure 5D).
Human MM cell growth by p62−/− stromal cells. (A) Marrow stromal cells from p62−/− or p62+/− mice were cocultured with GFP-labeled MM1.S cells for 3 days. Identification of MM cells was performed by fluorescence microscopy. Results represent the mean (± SEM) for 4 determinations. *P < .01 compared with cultures containing stromal cells from p62+/− mice. (B) IL-6 and TNF-α production in cocultures of human MM cells with p62−/− or p62+/− mouse marrow stromal cells. Stromal cells from p62−/− or p62+/− littermates were cocultured with MM1.S cells for 3 days. The conditioned media were harvested and assayed using commercially available ELISAs. Results represent the mean (± SEM) for 4 determinations. *P < .01 compared with cultures containing p62+/− stromal cells. (C) VCAM-1 expression on stromal cells. Stromal cells from the p62−/− or p62+/− littermates were cultured for 3 days, the cell lysates were collected, and analyzed by Western blot using anti–mouse VCAM-1. (D) VCAM-1 mRNA levels in p62+/− or p62−/− bone marrow stromal cells cocultured with MM1.S. Marrow stromal cells from p62+/− or p62−/− mice were cocultured with MM1.S cells for 3 days, the myeloma cells removed by vigorous washing as described in “Discussion,” and murine VCAM-1 mRNA was quantitated by quantitative PCR. Similar results were seen in 3 independent experiments.
Human MM cell growth by p62−/− stromal cells. (A) Marrow stromal cells from p62−/− or p62+/− mice were cocultured with GFP-labeled MM1.S cells for 3 days. Identification of MM cells was performed by fluorescence microscopy. Results represent the mean (± SEM) for 4 determinations. *P < .01 compared with cultures containing stromal cells from p62+/− mice. (B) IL-6 and TNF-α production in cocultures of human MM cells with p62−/− or p62+/− mouse marrow stromal cells. Stromal cells from p62−/− or p62+/− littermates were cocultured with MM1.S cells for 3 days. The conditioned media were harvested and assayed using commercially available ELISAs. Results represent the mean (± SEM) for 4 determinations. *P < .01 compared with cultures containing p62+/− stromal cells. (C) VCAM-1 expression on stromal cells. Stromal cells from the p62−/− or p62+/− littermates were cultured for 3 days, the cell lysates were collected, and analyzed by Western blot using anti–mouse VCAM-1. (D) VCAM-1 mRNA levels in p62+/− or p62−/− bone marrow stromal cells cocultured with MM1.S. Marrow stromal cells from p62+/− or p62−/− mice were cocultured with MM1.S cells for 3 days, the myeloma cells removed by vigorous washing as described in “Discussion,” and murine VCAM-1 mRNA was quantitated by quantitative PCR. Similar results were seen in 3 independent experiments.
Effects of loss of p62 on OCL formation induced by stromal cells
To further determine the effects of loss of p62 on OCL formation, we characterized bone marrow stromal cells from p62−/− mice and p62+/− mice for their capacity to support osteoclastogenesis. Normal spleen cells, as a source of OCL precursors, were cocultured with marrow stromal cells from p62−/− or p62+/− mice. Both types of stromal cells supported low levels of OCL formation in the absence of TNF-α. However, p62−/− stromal cells displayed a markedly reduced capacity to support osteoclastogenesis when treated with TNF-α compared with p62+/− stromal cells (Figure 6A). We then examined the levels of RANKL expression by p62+/− and p62−/− marrow stromal cells to determine whether the decrease in OCL formation seen in cocultures of OCL precursors with p62−/− stromal cells was due to defective RANKL production. p62−/− stromal cells treated with TNF-α released lower RANKL levels in their conditioned media compared with p62+/− marrow stromal cells (Figure 6B).
OCL formation in cocultures of normal OCL precursors with p62−/− stromal cells treated with TNF-α. (A) CFU-GM cells (104 cells/well) from spleens of p62+/− mice were cultured with stromal cells from p62+/− and p62−/− mice for 7 days in the presence of TNF-α. The cells were then stained for TRAP, a marker enzyme of OCLs, and the number of TRAP+ multinucleated cells determined. Results represent the mean (± SEM) for 4 determinations. *P < .01 compared with cells cocultured with p62+/− cultures. (B) RANKL production by p62+/− and p62−/− mouse stromal cells. Stromal cells from long-term mouse marrow cultures were treated with media alone or TNF-α. Conditioned media were harvested 4 days after the start of the cultures. The concentration of soluble RANKL present was determined using an ELISA kit for mouse RANKL. Results are reported as RANKL concentration (pg/mL) and are the mean (± SEM) of 4 samples. *P < .01, compared with p62+/− stromal cell cultures. Similar results were seen in 3 independent experiments.
OCL formation in cocultures of normal OCL precursors with p62−/− stromal cells treated with TNF-α. (A) CFU-GM cells (104 cells/well) from spleens of p62+/− mice were cultured with stromal cells from p62+/− and p62−/− mice for 7 days in the presence of TNF-α. The cells were then stained for TRAP, a marker enzyme of OCLs, and the number of TRAP+ multinucleated cells determined. Results represent the mean (± SEM) for 4 determinations. *P < .01 compared with cells cocultured with p62+/− cultures. (B) RANKL production by p62+/− and p62−/− mouse stromal cells. Stromal cells from long-term mouse marrow cultures were treated with media alone or TNF-α. Conditioned media were harvested 4 days after the start of the cultures. The concentration of soluble RANKL present was determined using an ELISA kit for mouse RANKL. Results are reported as RANKL concentration (pg/mL) and are the mean (± SEM) of 4 samples. *P < .01, compared with p62+/− stromal cell cultures. Similar results were seen in 3 independent experiments.
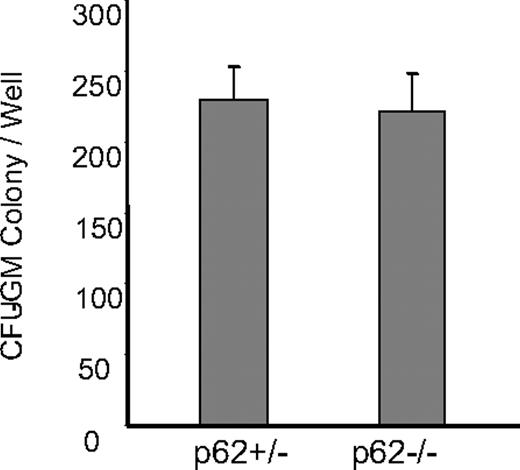
If p62 is to be a potential therapeutic target for MM, it is important to know the effects of loss of p62 on normal hematopoiesis. As shown in Figure 7, loss of p62 did not affect colony-forming units of granulocyte/macrophage (CFU-GM) colony formation in marrow cultures of these mice.
CFU-GM colony formation in cultures of p62+/− and p62−/− bone marrow cells. Marrow cells were cultured at 5 × 103 cells/well in α-MEM containing 1.2% methylcellulose, 30% FBS, 1% deionized BSA, and 100 pg/mL recombinant mouse GM-CSF (R&D Systems). Cells were plated in a volume of 1.0 mL in a 35-mm Petri dish and were incubated at 37°C in a humidified atmosphere of 5% CO2 for 7 days. CFU-GM colonies were scored after 7 days of culture using an inverted microscope.
CFU-GM colony formation in cultures of p62+/− and p62−/− bone marrow cells. Marrow cells were cultured at 5 × 103 cells/well in α-MEM containing 1.2% methylcellulose, 30% FBS, 1% deionized BSA, and 100 pg/mL recombinant mouse GM-CSF (R&D Systems). Cells were plated in a volume of 1.0 mL in a 35-mm Petri dish and were incubated at 37°C in a humidified atmosphere of 5% CO2 for 7 days. CFU-GM colonies were scored after 7 days of culture using an inverted microscope.
Discussion
Adhesive interactions between MM cells and stromal cells result in increased production of cytokines such as TNF-α, IL-6, and RANKL by the stromal cells, which induce MM cell growth and OCL formation.2 These adhesive interactions activate multiple signaling pathways in stromal cells that play important roles in their enhancement of tumor growth and bone destruction. Ishitsuka and coworkers have shown that p38 MAPK is involved in the increased osteoclastogenesis in MM and that blocking p38 MAPK inhibited IL-6 secretion from long term cultures of bone marrow stromal cells derived from MM patients.26 Further, inhibition of p38 MAPK decreased osteoclastogenesis in a murine model of human MM. Mitsiades et al have shown that NF-κB is also activated in bone marrow stromal cells when MM cells bind to marrow stromal cells and that TNF-α increased adhesion of bone marrow stromal cells to MM cells and increased production of IL-6.27 These results suggest that inhibition of multiple signaling pathways will be required to block the stimulatory effects of marrow stromal cells in MM. Therefore, we determined if targeting p62 could affect multiple signaling pathways in MM stromal cells. p62 is an adaptor protein that has no intrinsic enzymatic activity but is a critical component of multiple signaling pathways activated in MM stromal cells. p62 forms multiprotein complexes that result in activation of ERK, p38, and NF-κB.28,29 We previously reported that increased signaling through p62 in OCL precursors also increases OCL formation in vitro and in vivo.18,21 Therefore, we determined if some of these signaling pathways are activated in primary marrow stromal cells from MM patients, their respective roles on MM cell growth and osteoclast formation, and the effects of knockdown or loss of p62 on tumor growth and OCL formation.
When primary marrow stromal cells from patients with MM were isolated and cultured for 3 weeks in Dexter-marrow cultures, the stromal cells from MM patients produced increased levels of IL-6 and VCAM-1 and demonstrated an increased capacity to support the growth of both IL-6–independent and IL-6–dependent human MM cell lines compared with primary normal marrow stromal cells. Nguyen and coworkers have also shown that bone marrow stromal cells from patients with MM have increased VCAM-1 expression and IL-6 and VEGF production compared with normal stromal cells, and this was, in part, p38 MAPK-dependent.30 These differences in VCAM-1 and IL-6 production by marrow stromal cells from patients with MM and healthy subjects did not appear to result from loss or enrichment of endothelial cells or monocytic within the mixed-cell population of stromal cells present in these preparations, because FACS analysis demonstrated similar distributions of endothelial cells and monocytic cells in these preparations. These differences appear to be intrinsic to the MM-derived marrow stromal cells, because after passage for 3 weeks in the absence of any detectable CD138 expression in the stromal cell preparation, the stromal cells still expressed high levels of IL-6, VCAM-1, and TNF-α. While it is possible these observed differences may result from the manner by which the stromal cells were derived, it more likely reflects that intrinsic changes have occurred in the marrow microenvironment of patients with MM that persists even after culture for more than 3 weeks. In support of this hypothesis, Golay and coworkers have also shown marrow stromal cells from patients with MM and leukemia continued to produce high levels of IL-6 and VEGF after 3 to 4 weeks of culture.31 The basis for this change in the intrinsic properties of the stromal cells is currently unknown, but may reflect changes that occur with chronic exposure of stromal cells to MM cells or cytokines that are up-regulated in the marrow microenvironment in response to MM cells. Similarly, persistent changes in the marrow stromal cells have also been detected in marrow samples from patients with Paget disease.32,33 In these experiments, marrow stromal cells from Paget patients continued to express high levels of RANKL after many passages in the absence of other cell types.
Marrow stromal cells from patients with MM showed greater responses to TNF-α, a cytokine that is increased in the marrow microenvironment of patients with MM,34 and treatment of primary stromal cells from MM patients significantly increased VCAM-1 expression compared with normal stromal cells. This increase responsivity to TNF-α was reflected by the increased NF-κB and p38 MAPK signaling. The increased expression of VCAM-1 induced by TNF-α was mediated by NF-κB, while the increased IL-6 production by stromal cells was mediated by p38 MAPK in both normal and MM cells. However, the mechanisms responsible are still a subject of active investigation.
Studies with knockdown of p62 demonstrated that p62 in marrow stromal cells play an important role in the activation of PKCζ, NF-κB, and p38 MAPK, which were necessary for increased expression of VCAM-1 and IL-6, and is an important contributor to the capacity of marrow stromal cells from both healthy and MM patients to support the growth of MM cells. Taken together, these results suggest that p62 is critical to the increased downstream signaling through NF-κB and p38 MAPK in the marrow microenvironment of patients with MM.
Importantly, loss of p62 in marrow stromal cells significantly decreased their capacity to produce RANKL when cocultured with human MM cells. The decreased RANKL production most likely resulted from the decreased p38 MAPK signaling with knockdown of p62 in these stromal cells. Xing and coworkers have previously reported that RANKL production was unaffected in stromal cells from p50 and p52 double knockout mice.35 Consistent with these findings, marrow stromal cells lacking p62 produced very low basal levels of RANKL, and this was minimally increased when the cells were treated with TNF-α (Figure 2).
In summary, our results demonstrate that p62 plays an important role in the increased NF-κB and p38 MAPK signaling in marrow stromal cells from patients with MM that results in increased VCAM-1, IL-6, TNF-α, and RANKL production. These data suggest that p62 is an attractive therapeutic target for treating MM and MM bone disease. However, any therapeutic target must be evaluated in terms of its hematologic toxicity. We found that CFU-GM, the granulocyte macrophage progenitors, are present in similar numbers in marrow and spleens from p62 knockout and p62 heterozygous mice. Similarly, p62 knockout mice have normal blood counts and do not display any hematologic abnormalities.36 These findings suggest that loss of p62 may only impact conditions in which NF-κB and p38 MAPK signaling is up-regulated, as in inflammatory arthritis and cancers, such as MM. In support of this hypothesis, p62−/− mice have decreased OCL formation compared with normal mice in response to high levels of parathyroid hormone-related peptide (PTHrP) but otherwise have normal basal OCL numbers.37 These results support further studies to examine the therapeutic utility of targeting p62 in MM.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
We thank Dr Deborah Galson for reading the manuscript and her constructive suggestions.
This work was supported by a Multiple Myeloma Research Foundation grant, a VA Merit Review grant, and by research funds from the National Institutes of Health (NIH; grant no. R01 AR053537-02). The materials are the result of work supported with resources and the use of facilities at the VA Pittsburgh Healthcare System, Research and Development.
National Institutes of Health
Authorship
Contribution: Y.H. performed the signaling and some of the biologic experiments; T.H. performed the initial signaling and biologic experiments; D.F.J. provided the ALB6 cell line and contributed to the design of coculture experiments; J.J.W. produced the knockout mice used in these studies and provided expertise on the mouse studies; J.S. generated the p62 knockout mouse line; G.D.R. helped design experiments and writing the manuscript; and N.K. performed the coculture experiments, supervised overall experiments, and wrote the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Noriyoshi Kurihara, VA Pittsburgh Healthcare System, Research and Development 151U, University Dr C, Rm 2E-115, Pittsburgh, PA 15240; e-mail: Kuriharan@upmc.edu.