Two related recent studies on erythropoiesis by Robach and colleagues describe surprising differential responses to erythropoietin with respect to skeletal muscle iron mobilization, apparently depending on normoxic versus hypoxic conditions.
Like other heavy metals, iron is toxic, albeit in bound form, essential for life. Thus elaborate mechanisms involving dozens of molecules balance systemic and cellular iron usage, detoxification, storage, and homeostasis, with the regulatory peptide hormone hepcidin a prominent recent addition to this repertoire.1 As the main consumer (80%) of mobilizable iron, the erythroid compartment in response to its homeostatic regulator erythropoietin (Epo) is an indirect but significant player in this balance. First, erythroid iron intake and incorporation into heme represent a sort of temporary iron store. Second, the “outflow” when aged erythrocytes are eaten up by macrophages also has to be taken into account. Finally, lowered hepcidin levels, due to, for example, elevated Epo, enable increased transfer of iron between macrophages and liver as the major storage organ via up-regulated activity of the iron exporter ferroportin.2 Although skeletal muscle cells contain up to 15% of total body iron in myoglobin and do express ferroportin, knowledge about the contribution of this potential iron storage depot to erythropoiesis has remained scarce so far.
In this issue of Blood, Robach et al describe hematologic and molecular responses in muscle samples upon Epo injections.3 Eight healthy volunteers received “clinical” doses of recombinant human Epo (65 IU per kg body weight), for the first 2 weeks every other day and then once per week. Besides measuring classical blood parameters as well as urinary hepcidin levels, the authors performed small muscle biopsies, a commendable effort by both patients and investigators. As expected, erythropoiesis was enhanced while hepcidin levels decreased. In muscle, there was a concomitant increase in ferroportin expression by about 70%, which, however, was accompanied by only a very minor reduction in myoglobin levels and thus more or less futile in terms of iron mobilization. To make the results even baffling, expression of the iron uptake protein transferrin receptor (TfR) went up in muscle, together with an elevated abundance of the iron storage protein ferritin (see figure). This indicated that there was an increased iron influx into muscle cells upon Epo administration, but this iron was not ending up in myoglobin. Measuring total cellular iron levels further corroborated this interpretation. At this stage, the overall picture might have been interpreted as expected hematologic results and a “complicated” situation in muscle.
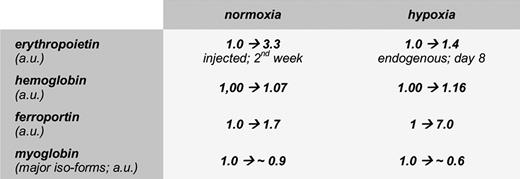
Changes in selected molecular components directly or indirectly involved in iron metabolism upon exposure of human subjects to either normoxic or hypoxic conditions. Data are shown in arbitrary units to facilitate comparison between factors of response and are average values deduced from the authors' original figures and tables.
Changes in selected molecular components directly or indirectly involved in iron metabolism upon exposure of human subjects to either normoxic or hypoxic conditions. Data are shown in arbitrary units to facilitate comparison between factors of response and are average values deduced from the authors' original figures and tables.
The story, however, becomes really interesting when seen in conjunction with an earlier paper from the same group.4 There, similar parameters were quantitated, again with human volunteers but at high altitude, to be precise in the Monte Rosa region at 4559m. In this really hypoxic environment (101 kPa → 59 kPa), the ensuing rise in hematocrit was accompanied by a significant loss of muscle-iron and myoglobin (see figure), lowered TfR and ferritin levels, and a massively elevated level of ferroportin. In this case, muscle cells indeed appeared to become a source of mobilizable iron.
How can these seemingly disparate data be reconciled? One could always argue that experimental protocols were not identical. While probands tested under normoxic conditions received Epo injections boosting their total levels by 350% throughout the second week, the mountain volunteers had to rely on an observed 40% increase of endogenous Epo (day 8). This does not offer an adequate explanation since the lower Epo concentrations had a much larger impact on ferroportin levels. The equation, more Epo/less hepcidin/more ferroportin activity/more iron release that beautifully explains the role of macrophages in iron homeostasis, appears to fail for muscle.
In their present paper, Robach et al discuss a variety of possible scenarios these differential responses could take on. One physiologically meaningful hypothesis sticks out, despite involving a notorious “factor X.” Such a factor might sense an emergency need for enhanced erythropoiesis, especially under hypoxia or eventually also upon blood loss. Thereby it would open a route to utilize the otherwise protected source of iron in muscle. In contrast, elevated Epo under normoxia might be sensed as a more “normal” situation, leading to the conventional route of increasing red blood cell production by involving the reticulo-endothelial system. It will be interesting to see whether and under which specific conditions myoglobin iron might also become mobilized under normal oxygen supply.
Biologic systems persist to be more complex than any possible preconception. Despite the decades that have passed since the first applications of Epo5 for example, to treat anemia in kidney diseases, cancer or—less beneficially—for blood doping, it looks as if there are still facets of this molecule and its role in iron homeostasis that need further study.
Conflict-of-interest disclosure: The authors declare no competing financial interests. ■