Abstract
Postthrombotic syndrome (PTS) is a chronic complication of deep venous thrombosis (DVT) that reduces quality of life and has important socioeconomic consequences. More than one-third of patients with DVT will develop PTS, and 5% to 10% of patients will develop severe PTS, which may manifest as venous ulceration. The principal risk factors for PTS are persistent leg symptoms 1 month after the acute episode of DVT, extensive DVT, recurrent ipsilateral DVT, obesity, and older age. Daily use of elastic compression stockings (ECSs) for 2 years after proximal DVT appears to reduce the risk of PTS; however, there is uncertainty about optimal duration of use and compression strength of ECSs and the magnitude of their effect. The cornerstone of managing PTS is compression therapy, primarily using ECSs. Venoactive medications such as aescin and rutoside may provide short-term relief of PTS symptoms. The likelihood of developing PTS after DVT should be discussed with patients, and symptoms and signs of PTS should be monitored during clinical follow-up. Further studies to elucidate the pathophysiology of PTS, to identify clinical and biologic risk factors, and to test new preventive and therapeutic approaches to PTS are needed to ultimately improve the long-term prognosis of patients with DVT.
Introduction
Deep vein thrombosis (DVT) is a common vascular condition that is associated with significant rates of morbidity and mortality. Although pulmonary embolism and recurrent venous thrombosis are well-known consequences of DVT, an important, underappreciated, chronic consequence of DVT is postthrombotic syndrome (PTS). PTS develops in 20% to 50% of patients with DVT,1,2 even when appropriate anticoagulant therapy is prescribed to treat the DVT. On the basis of its high incidence and prevalence, PTS is the single most frequent complication of DVT.
Some practitioners may believe that PTS is primarily a cosmetic or “nuisance” problem. To the contrary, PTS is burdensome and potentially debilitating to patients, and it is a condition for which patients frequently seek medical advice. Manifestations of PTS vary from mild clinical symptoms or signs to more severe manifestations such as chronic leg pain that limits activity and ability to work, intractable edema, and leg ulcers.3 PTS has been shown to have significant, adverse effects on quality of life and productivity,4-6 and is costly as measured by health resource utilization, direct costs, and indirect costs.7-9
In this review, I address the following questions: (1) How is PTS diagnosed? (2) Can we identify patients with DVT who are at risk of developing PTS? (3) How can PTS be prevented? (4) How do I treat PTS? and (5) What are the gaps in our understanding of PTS that should be addressed by future research? I also address upper-extremity PTS and the responsibility to discuss long-term prognosis with patients with DVT.
This paper focuses on PTS in adults. Readers with an interest in PTS in children are referred to a recent review of this topic.10
How I diagnose PTS
Clinical presentation of PTS
PTS is termed a “syndrome” because it is associated with groupings of symptoms and clinical signs that typically vary from patient to patient (Table 1). Patients with PTS experience aching pain, heaviness, swelling, cramps, itching, or tingling in the affected limb. Symptoms may be present in various combinations and may be persistent or intermittent. Typically, symptoms are aggravated by standing or walking and improve with resting, leg elevation, and lying down. Signs that may be noted on physical examination of the limb include edema, perimalleolar or more extensive telangiectasia, brownish pigmentation, and venous eczema (Figure 1). Secondary varicose veins may occur, and brawny, tender thickening of the subcutaneous tissues of the medial lower limb known as lipodermatosclerosis may develop. A feared complication is the development of one or more venous leg ulcers, which require close medical attention and often recur. Leg ulcers can be precipitated by minor trauma and are characteristically chronic, painful, and slow to heal.3,11
How is PTS diagnosed?
PTS is a clinical diagnosis.
PTS is diagnosed on clinical grounds based on the development of characteristic symptoms and signs in a patient with prior DVT. The clinical picture of PTS can be nonspecific, because conditions other than DVT (eg, primary venous insufficiency, chronic congestive heart failure, trauma) may result in similar symptoms or signs in the lower extremities. However, in a patient with objectively confirmed prior DVT who has typical PTS symptoms and signs in that limb, PTS is usually the correct diagnosis. In some patients, it may take up to 3 to 6 months for the initial pain and swelling associated with acute DVT to resolve; hence, a diagnosis of PTS should be deferred until after the acute phase has passed.3
In the absence of characteristic clinical features of PTS, the demonstration of venous abnormalities (eg, venous reflux, persistent venous obstruction, venous hypertension) on invasive (eg, contrast venography) or noninvasive (eg, ultrasonography, plethysmography) imaging or testing should not, in itself, lead to a diagnosis of PTS in a patient with previous DVT. This is because, although many patients with symptomatic PTS have detectable venous abnormalities, many patients with DVT who do not have symptoms of PTS can also be shown to have such abnormalities.12-14 I do not routinely perform invasive or noninvasive venous testing in patients with a clear clinical diagnosis of PTS.
Clinical tools are available to help diagnose and measure the severity of PTS.
Two clinical tools that are frequently used in clinical investigations to measure PTS are the Villalta PTS scale15 and the CEAP (clinical, etiologic, anatomic, and pathophysiologic) classification for chronic venous disease.16 The Villalta scale, discussed further in the next paragraph, is a clinical scoring system that is based on severity ratings of PTS symptoms and signs. The CEAP classification tool combines clinical and objective findings into 7 classes of chronic venous disease with subcategories to denote causative, anatomic, and pathophysiologic attributes. Other, less frequently used scales have been proposed as well.17
It would clearly be an advantage to achieve agreement on a uniform definition of PTS. Because a wide variety of definitions have been used in the published literature, clinicians may lack confidence in their ability to diagnose PTS, and it has been difficult to compare research data across studies or to formally combine data in meta-analyses. Recently, in a step toward standardizing the measurement of PTS in clinical studies, the Subcommittee on Control of Anticoagulation of the Scientific and Standardization Committee of the International Society on Thrombosis and Hemostasis recommended that the Villalta scale be adopted to diagnose and grade the severity of PTS.18 The scale can be used as a binary (ie, yes or no), categorical (none, mild, moderate, severe), or continuous (score range, 0-33) measure. The components of the Villalta scale and its scoring algorithm are shown in Table 2. A recent review of the scale's measurement (ie, psychometric) properties indicates that it is a reliable and valid measure of PTS, is acceptable to research subjects and research personnel, and shows responsiveness to clinical change in PTS.19 Although to date, the Villalta scale has primarily been used as a research tool and is not yet in common use in the clinical setting, I use it in my own practice to diagnose PTS and to monitor its severity over time.
Objective diagnostic testing can be helpful in some circumstances.
If a patient with a history of a previously documented DVT develops clinical manifestations compatible with PTS, there is generally no need for further diagnostic investigation. However, objective confirmation can be useful in patients who have a characteristic presentation of PTS but who do not have a history of previous DVT. Compression ultrasonography can be performed to assess for lack of compressibility of the popliteal or common femoral veins, along with the use of continuous-wave Doppler scan to assess for reflux of their venous valves. In one study, the combination of a standardized clinical evaluation, compression ultrasonography, and continuous-wave Doppler analysis was able to reliably diagnose or exclude previous proximal vein thrombosis in almost 90% of patients.20
Ascending contrast venography may show findings that suggest previous DVT such as narrowing or occlusion of the deep veins, opacification of fewer deep veins than normal or opacification of superficial or deep collateral veins, reduced vein diameter because of fibrotic thickening of the recanalized vein's wall, and an irregular-appearing or multichanneled lumen.21 However, because contrast venography is an invasive test that is technically demanding, is costly, and has risks associated with the requirement for contrast media, I do not advocate its use for this purpose.
When patients with PTS experience new leg symptoms or a change in previous symptoms, they may fear that they have a new episode of acute venous thrombosis. It should be explained to patients that it is not uncommon for PTS symptoms to wax and wane over time. If new symptoms in the affected leg develop or if chronic symptoms in the affected leg become worse and there are no associated symptoms that could suggest acute pulmonary embolism, I generally advise my patients to rest their leg and wait a day because in most cases, the symptoms are probably due to PTS and will settle down. However, because patients with PTS are at increased risk of recurrent venous thromboembolism (VTE), if such leg symptoms persist or progress, particularly in the setting of new clinical risk factors for DVT, investigation to rule out recurrent DVT is warranted. The approach to the diagnosis of recurrent DVT in patients with PTS is the same as in patients without PTS. Establishing the diagnosis of recurrent ipsilateral DVT can be challenging, because the finding of a noncompressible venous segment in the same area as the first DVT can represent new or residual thrombus. An unequivocal change in the extent of thrombosis or an increase in clot diameter of 4 mm or more on the current ultrasound scan compared with the previous ultrasound scan is considered to be indicative of new ipsilateral DVT.22-24 Recent studies suggest that strategies that use D-dimer testing alone25,26 or in combination with clinical probability testing27 can reduce the need to perform ultrasonography in patients with suspected recurrent DVT.
Can we identify patients who are at risk of developing PTS?
What causes PTS to develop after DVT?
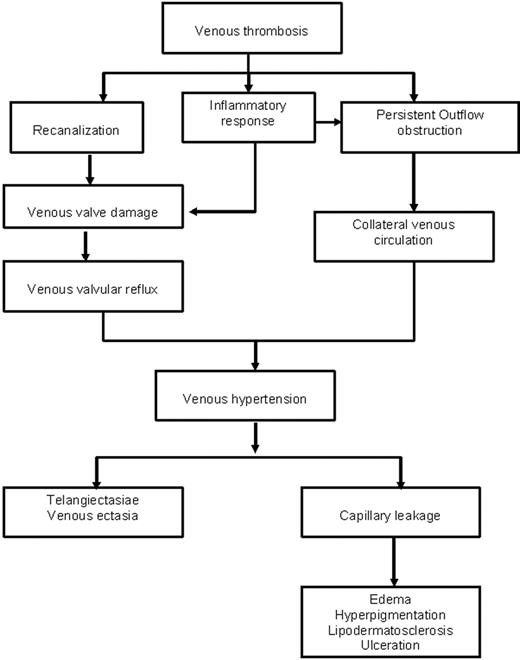
It is thought that PTS occurs primarily as a consequence of venous hypertension. Venous hypertension leads to impaired venous return, reduced calf muscle perfusion, abnormal function of the microvasculature with increased tissue permeability, and, consequently, the characteristic clinical manifestations of PTS.11,28
DVT can lead to chronic venous hypertension via 2 principal mechanisms: persistent (residual) venous obstruction and valvular reflux. Standard anticoagulant treatment of DVT prevents thrombus extension and embolization to the pulmonary arteries, but it does not directly lyse the acute thrombus. Follow-up studies of patients with DVT who were treated with anticoagulants have shown that in many cases only partial clearance of the thrombus occurs.29-32 Damage to venous valves leading to valvular reflux occurs frequently after DVT, probably by thrombus-induced activation of inflammation, fibrous scarring associated with acute and resolving thrombosis, or venous dilation distal to the obstructed venous segment33-36 (Figure 2). Of the 2 mechanisms, persistent venous obstruction appears to be the more important; on the basis of 2 recent reports, the presence of residual venous obstruction 6 months after DVT alone or in combination with venous reflux predicted the development of PTS, whereas the presence of venous reflux alone did not.31,37
Incidence of PTS after an episode of DVT
On the basis of data from contemporary prospective studies with long-term (ie, 12 months or longer) follow-up, 20% to 50% of patients with DVT can expect to develop PTS and 5% to 10% of patients will develop severe PTS (severe symptoms and/or severe signs, which may include venous ulcers).1,2,38-42 In most cases, PTS develops within the first year or two after DVT.
Individual risk factors for PTS
Because risk factors for PTS are incompletely understood, it is difficult to predict which patients with DVT will develop PTS. However, new information has been gained in the past few years about clinical and biologic factors that influence the risk of developing PTS. In a recent prospective cohort study of 387 patients with acute symptomatic DVT,2 we found that incomplete resolution of leg symptoms and signs by 1 month after DVT strongly predicted the development of PTS during the subsequent 2 years. We and others have also identified that venous thrombosis of the common femoral or iliac vein (compared with distal or popliteal vein DVT),2,40,42,43 previous ipsilateral venous thrombosis,1,2,39,40,44-46 higher body mass index,2,41,42,47,48 and older age2,39,41 are associated with a higher likelihood of developing PTS. Female sex has been inconsistently associated with PTS.2,40,42 The risk of PTS does not appear to be influenced by carriage of the factor V Leiden or the prothrombin mutation2,42 or by the circumstances of the initial DVT (ie, unprovoked, result of reversible risk factors, or cancer related).2,39-41
A relationship does not appear to exist between long-term duration or long-term intensity of oral anticoagulation and the subsequent development of PTS.4,40 However, one study reported that patients with DVT who had subtherapeutic International Normalized Ratios more than half of the time during the initial 3 months of treatment with vitamin K antagonists had a 3-fold higher risk of developing PTS,41 which reinforces the importance of close monitoring after the initial thrombotic episode to ensure an adequate intensity of oral anticoagulant therapy.
With regard to biomarkers that could help to predict PTS, recent studies have reported that elevated levels of markers of inflammation (eg, ICAM-1, interleukin-6, and C-reactive protein)49,50 and D-dimer40,51 early after diagnosis or within a few months of DVT were associated with the development of PTS. A large, prospective multicenter study that is examining the predictive role of various markers of inflammation, D-dimer, and thrombophilia in the development of PTS is currently under way.52
In summary, proximally extensive DVT, prior ipsilateral DVT, persistent venous symptoms 1 month after DVT, obesity, and older age appear to be robust clinical predictors of PTS. Clinicians who manage patients with DVT should be aware of these risk factors and should routinely assess if they are present in their patients. At the same time, it should be kept in mind that patients with DVT without these features can also develop PTS.
How can PTS be prevented?
Primary and secondary thromboprophylaxis
The systematic use of thromboprophylaxis to prevent DVT in high-risk hospitalized patients as recommended in evidence-based consensus guidelines53 will prevent cases of PTS. Unfortunately, there remains much room for improvement in our practices, because audits conducted in a number of countries consistently show that thromboprophylaxis continues to be underused.53-55
However, even when appropriate thromboprophylaxis is used, the risk of VTE is not eliminated. Moreover, approximately one-half of VTE events occur unpredictably; hence, they are not preventable with thromboprophylaxis. Because recurrent ipsilateral DVT is an important risk factor for PTS, clinicians should be diligent about reducing the risk of recurrent DVT in their patients by providing anticoagulation of appropriate intensity and duration to treat the initial DVT.56,57
Elastic compression stockings
Graduated elastic compression stockings (ECSs) reduce venous hypertension, decrease edema, and improve tissue microcirculation.58 Three trials have evaluated the effectiveness of long-term use of ECSs for the prevention of PTS after symptomatic proximal DVT. In a Dutch study of 194 patients who were randomly allocated to daily use of a made-to-measure knee-length ECS with 30 to 40 mm Hg of compression strength for at least 2 years or no stocking, ECSs resulted in a decrease from 47% to 20% of mild PTS and from 23% to 11% of severe PTS.59 Prandoni et al39 evaluated the effectiveness of “off-the-rack” knee-length ECSs with 30 to 40 mm Hg of compression strength, worn for 2 years, versus no stockings in 180 patients with proximal DVT. Use of ECSs reduced the risk of PTS from 49% to 26% (adjusted HR, 0.5; 95% CI, 0.3-0.8) in favor of ECSs.39 However, in a Canadian randomized trial conducted by Ginsberg et al14 of patients with proximal DVT who had not developed PTS by 1 year after the initial DVT, no benefit was observed of daily use of ECSs with 20 to 30 mm Hg of compression strength for up to 4 years, compared with use of sham stockings (1 or 2 sizes too large). PTS developed in 0 of 24 patients in the ECS group versus 1 of 23 patients in the sham-stockings group (P = .49).14
A meta-analysis that pooled the 3 studies concluded that use of ECSs after DVT substantially reduces the risk of any PTS (OR, 0.3; 95% CI, 0.20-0.48) and of severe PTS (OR, 0.39; 95% CI, 0.20-0.76).60 In light of these data, the guidelines from American College of Chest Physicians recommend that patients with acute symptomatic proximal DVT wear ECSs with an ankle pressure gradient of 30 to 40 mm Hg for a minimum of 2 years, or even longer if patients have symptoms of PTS, if this is feasible (ie, if patients or their caregivers are able to apply and remove stockings).56
Notwithstanding this recommendation, I believe that important questions remain as to the true magnitude of effectiveness and general feasibility of using ECSs to prevent PTS in patients with DVT. First, the 3 previous trials had various limitations that could affect their validity and generalizability, including modest sample size, recruitment at a single center, lack of placebo control, and lack of blinding of assessors. The lack of blinding in the 2 positive studies reduces confidence in the results because scales used to diagnose PTS have subjective elements that are susceptible to reporting bias. Although ECSs are unlikely to cause harm, they are difficult to apply, uncomfortable, and expensive, and require replacement every few months. The SOX Trial, an ongoing large multicenter blinded trial that is comparing active versus placebo stockings to prevent PTS after proximal DVT is anticipated to provide important additional information on the effectiveness of ECS.52 Second, it is not known whether ECSs should be used in patients with symptomatic distal DVT, because the above-mentioned trials enrolled only patients with proximal DVT. Third, it is unclear whether ECSs prevent PTS or merely palliate it, in which case it may be equally effective and more convenient for patients to initiate the use of ECSs at the time of onset of PTS. Fourth, it would be worth evaluating the effectiveness of ECSs with lighter (20-30 mm Hg) compression strength to prevent PTS, because they are easier to apply than are ECSs with 30 to 40 mm Hg of compression strength, especially for older patients, and they appear to have similar effectiveness in preventing recurrent venous ulcer.61 Finally, it is not known for how long ECSs need to be worn. Although the trials to date evaluated the use of ECSs for 2 years or longer, a recent trial reported that beyond an initial 6-month period of use, there was no incremental benefit in prolonging compression therapy for an additional 18 months,62 suggesting that the use of ECSs for 6 months might be adequate and would be easier for patients to tolerate than the currently recommended 2 years.
Based on the current state of published evidence regarding the use of ECSs to prevent PTS and pending the results of ongoing trials in this area, I believe that a reasonable clinical approach is to prescribe below-knee ECSs with 30 to 40 mm Hg compression strength to patients who have residual leg pain or swelling after proximal or distal DVT and to continue the ECSs for as long as the patient derives symptomatic benefit or is able to tolerate them.
Thrombolysis of acute DVT to prevent PTS
Some studies of systematic thrombolytic therapy and, more recently, catheter-directed thrombolysis techniques support the hypothesis that early thrombolysis of acute DVT reduces the subsequent occurrence of PTS, presumably by rapidly reestablishing venous patency and preserving venous valves.63,64 However, because studies to date have been small in size and have had various methodologic limitations, uncertainty remains as to the long-term effects of thrombolysis on PTS as well as the risks associated with these procedures. The safety, effectiveness, and cost-effectiveness of newer endovascular strategies such as catheter-directed thrombolysis, including pharmacomechanical catheter-directed thrombolysis (ie, with inclusion of thrombus fragmentation and/or aspiration), are currently undergoing evaluation in rigorously designed, randomized controlled trials in which PTS is the primary study outcome.28,65
Based on the current state of evidence, I recommend against the routine use of early thrombolytic therapy for the prevention of long-term sequelae of DVT. In selected cases, however, thrombolytic therapy may be considered. In the current guidelines from the American College of Chest Physicians, it is suggested that in selected patients with extensive acute proximal DVT (eg, those with iliofemoral DVT, symptoms fewer than 14 days, good functional status, life expectancy of more than a year) in whom the risk of bleeding is low, catheter-directed or pharmacomechanical thrombolysis, or, less ideally, systemic thrombolytic therapy, followed by standard anticoagulant therapy, may be used to reduce acute DVT symptoms and PTS, providing that appropriate expertise and resources are available.56
How I treat PTS
Compression therapy
Compression therapy and frequent leg elevation are the cornerstones of managing established PTS. ECSs are helpful to reduce leg swelling, heaviness, and aching.66 Patients should be advised to apply their stockings in the morning and to remove them at bedtime or earlier in the evening, if they are able to rest and elevate their legs. The principal contraindication to using ECSs is symptomatic peripheral arterial disease, because claudication can worsen when stockings are worn. There are also practical limitations to using ECSs. If a patient lacks hand strength, arm strength, or the finger dexterity required to apply ECSs, assistance can be provided by a caregiver or by using a stocking aid (fabric sleeve, plastic or metal frame) that can be purchased at medical supply stores. The use of talcum powder to reduce skin friction and rubber gloves to improve grip can also be helpful. ECSs are now available in a wide array of styles, textures, and colors.
I emphasize to my patients that compression is a form of active therapy that requires adherence on their part to maximize effectiveness. I start by prescribing a knee-length ECS with 30 to 40 mm Hg compression strength; however, some patients will find these constricting or difficult to apply, in which case an ECS with 20 to 30 mm Hg compression strength can be tried. Other patients will require higher compression strengths (eg, 40-50 mm Hg) to adequately control edema. Knee-length and thigh-length stockings have similar physiologic effects in decreasing venous stasis of the lower limb, but the former are easier to apply and are more comfortable.67
Other compression therapies have been evaluated for the treatment of severe manifestations of PTS. In a randomized crossover trial conducted in 15 patients, the use of an intermittent compression extremity pump twice daily for 2 months (20 minutes per session, 50 mm Hg pressure) reduced edema and improved PTS symptoms.68 Recently, a randomized crossover trial in 32 patients with severe PTS tested the effectiveness of a portable, battery-operated lower-limb venous return assist device (VenoWave; Saringer Life Science Technologies) that is worn below the knee strapped firmly to the calf. The device provides compression of the calf and increases upward volumetric displacement of venous blood. Use of the device alone or in combination with ECSs was associated with improvement in quality of life and reduced the severity of PTS.69 The VenoWave device is now approved by Health Canada and by the US Food and Drug Administration.
Medications
Some evidence suggests that “venoactive” or “phlebotonic” remedies such as aescin (a derivative of the horse chestnut seed) or rutoside reduce symptoms of PTS. In a clinical trial of 120 patients conducted in Italy, the oral administration of hydroxyethylrutoside for 1 year improved symptoms of PTS (improvement defined as reduction in the Villalta PTS score to < 5, or decrease in score by at least 30% in comparison to the baseline score, at any time during the follow-up) to a similar extent as below-knee ECSs, with no added benefit of combining the 2 therapies.70 A 12-week trial of ECSs versus twice-daily horse chestnut seed extract in 240 patients with chronic venous insufficiency showed that both therapies had similar effects in reducing edema (as measured by lower leg volume) and were well tolerated.71 A subsequent Cochrane review of 17 trials that have compared horse chestnut seed extract to placebo, ECSs, or other medications concluded that horse chestnut seed extract is efficacious for the short-term treatment of symptoms of chronic venous insufficiency such as leg pain and edema and that adverse events were mild and infrequent and included gastrointestinal complaints, dizziness, nausea, headache, and pruritus; however, larger, more rigorous trials are required to assess long-term effectiveness and safety.72 In my own practice, I often suggest a short-term (ie, up to 3 weeks) trial of twice-daily horse chestnut seed extract (available at natural product stores) to patients whose PTS symptoms are not adequately controlled by ECSs.
No evidence suggests that short-term or long-term use of diuretics is effective for the treatment of PTS-related edema or that nonsteroidal anti-inflammatory drugs improve symptoms of PTS beyond their analgesic effects.
Venous ulcer management
Postthrombotic venous ulcers are generally treated conservatively with compression bandages or stockings, leg elevation, topical dressings, and various pharmacologic compounds, but they can be refractory to therapy and tend to recur. Patients with ulcers should be managed by a specialist with expertise in managing postthrombotic ulcers. Depending on the center, this may include dermatologists, internists, or vascular or plastic surgeons. Surgery may be advocated in select patients when ulcers do not respond to conservative treatment. Although detailed discussion of the management of venous ulcers is beyond the scope of this article, the interested reader is referred to recent reviews or guidelines that have addressed this topic.11,56,73
Endovascular or surgical treatment of PTS
A few case reports and small case series reported by vascular interventional radiologists or venous vascular surgeons at highly specialized centers suggest that procedures such as endovascular stent recanalization for patients with obstruction of the iliac vein or inferior vena cava, or surgical valvuloplasty for chronic femoropopliteal obstruction and deep venous valvular reflux may be of benefit to selected patients with moderate or severe PTS.28 To date, however, no methodologically rigorous, comparative trials have addressed whether these therapies improve the clinical manifestations of PTS.
Available strategies to prevent and treat PTS are summarized in Table 3.
Upper-extremity PTS
PTS of the upper extremity, although less well studied than lower-extremity PTS, has been reported to occur in 15% to 25% of patients after treated upper-extremity DVT.74,75 Upper-extremity PTS is a potentially disabling condition that adversely affects quality of life, particularly if the dominant arm is involved.76 Symptoms include arm swelling, heaviness, and fatigue with exertion.75,76 On examination, dilation of the superficial veins of the upper arm and chest wall, as well as dependent cyanosis of the arm, may be noted. To date, no controlled studies have evaluated the effectiveness of elastic bandages, compression sleeves (as are used for lymphedema), or venoactive drugs to prevent or treat PTS after upper-extremity DVT. Anecdotal evidence suggests that patients with persistent arm swelling and pain after upper-extremity DVT may derive symptomatic relief from elastic bandages or compression sleeves.56 Because these are unlikely to cause harm, they should be tried.
The responsibility to discuss long-term prognosis with our DVT patients
Patients with acute DVT often assume that the appearance and function of their leg (or arm) will return to normal once anticoagulant treatment is initiated or completed. Although the long-term prognosis of DVT is favorable for many patients, physicians should proactively and candidly discuss with their patients that PTS is a frequent complication of DVT, and should monitor their patients for the emergence of PTS symptoms and signs during follow-up. For those patients who do develop PTS, it is important to explain that it is a chronic condition that can generally be expected to wax and wane over time. Despite the common belief that patients with PTS have a uniformly poor prognosis, a few recent studies have suggested that prognosis might be better than previously reported, with greater than 50% of patients remaining stable or improving during long-term follow-up.2,77-79 However, currently, it is not possible to reliably predict the course of PTS in individual patients.
PTS, particularly if severe, reduces quality of life, impairs physical functioning, may reduce the ability to work or to conduct leisure activities, and can be associated with progressive, unsightly changes to the leg. Therefore, physician or nurse-initiated psychological support is critical. As for other chronic conditions for which treatment options are limited, organizing local support groups for patients with PTS can be a source of comfort and empowerment to patients. Patient-directed information on PTS is also available on websites such as the National Alliance for Thrombosis and Thrombophilia (http://www.stoptheclot.org/), a patient-led advocacy organization,80 and the Venous Disease Coalition (http://www.venousdiseasecoalition.org/), a public and interdisciplinary consortium to promote public and health professional awareness of venous disease.81
Research needs
PTS is a relatively untapped area of venous thrombosis research, and research needs are substantial. Important subjects for future investigation include better elucidation of the pathophysiology of PTS; identification of clinical, anatomic, physiologic, and genetic risk factors for PTS; and development of PTS risk prediction models that integrate clinical and biomarker information. Further work to investigate the association between inflammation and PTS could lead to identification of new therapeutic targets for preventing PTS after DVT. Finally, rigorous evaluation of the long-term effectiveness and safety of catheter-directed thrombolytic techniques to prevent PTS as well as endovascular or surgical procedures to treat moderate-to-severe PTS is required.
Acknowledgment
S.R.K. is a recipient of a National Research Scientist Award from the Fonds de la Recherche en Santé du Québec.
Authorship
Contribution: S.R.K. developed and wrote the paper.
Conflict-of-interest disclosure: The author has received research funding from the Canadian Institutes of Health Research and from Sigvaris Corporation (in-kind support) for an ongoing trial of compression stockings versus placebo stockings to prevent PTS.
Correspondence: Susan R. Kahn, McGill University, Division of Internal Medicine, and Centre for Clinical Epidemiology and Community Studies, Jewish General Hospital, 3755 Cote Ste Catherine, Rm A-114, Montréal, PQ H3T 1E2, QC, Canada; e-mail: susan.kahn@mcgill.ca.