Abstract
Abstract 1328
Poster Board I-350
Heparin-induced thrombocytopenia (HIT) is a clinicopathologic diagnosis based on pretest clinical assessment aided by the 4T score and confirmed by laboratory testing for the presence of anti-heparin-platelet factor 4 antibody (HIT Ab). Prompt and accurate diagnosis of HIT is paramount due to an extraordinarily high risk of thrombosis, and the inherent risk of bleeding and high cost of direct thrombin inhibitors (DTI). The polyspecific enzyme linked immunosorbent assay (poly-ELISA) for the HIT Ab is the most commonly available test that detects IgG, IgM and IgA HIT Ab. The IgG-specific ELISA detects only IgG HIT Ab, the antibody that is known to cause HIT. The use of a second step ELISA with high-dose heparin in the reagent improves the specificity by demonstrating heparin-dependence of the antibody detected. The 4T score was developed to predict the probability of HIT. This score takes into account the severity of thrombocytopenia, timing of platelet fall with relation to heparin use, presence of new thrombosis, and other causes of thrombocytopenia. The high negative predictive value of the 4T score has been validated in multiple studies (Bryant et al, BJH 2008). However, the polyspecific ELISA was used in most of these studies, increasing the possibility of false positive tests.
We have collected a database of patients being tested for HIT at our institution, where the IgG-specific ELISA along with high-dose heparin inhibition is being used to detect the HIT Ab. We performed a retrospective review of the last 165 ELISAs performed and the clinical circumstances of the testing. We hypothesize that the high negative predictive value of the 4T score combined with the more specific IgG-specific ELISA could be used to rule out HIT and avoid the cost of testing and empiric use of DTI.
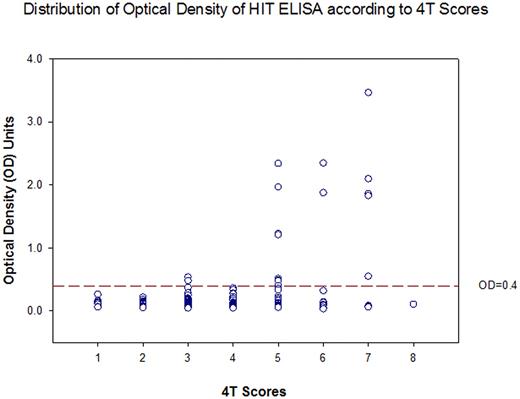
4T scores of 165 patients were analyzed and compared to the results of the HIT Ab. The distribution of optical density units of the ELISA according to 4T score is shown in Figure 1. Of the 165 patients, 107 patients (64%) had a 4T score of 0-3. Of those 107 patients, 2 patients had OD>0.4; both had no significant inhibition with the addition of high-dose heparin (Table 1). Thus none of the 107 patients had a positive IgG-specific ELISA for HIT Ab. Thus having a low 4T score has a sensitivity of 100% for IgG-specific ELISA for HIT Ab, specificity of 71%. This translates to a positive predictive value of 26%, and a negative predictive value of 100% (Table 2).
Based on our data, we conclude that patients with low 4T scores (0-3) are highly unlikely to have HIT. Therefore, we propose that patients with a low 4T score do not need the laboratory workup or empiric treatment for HIT. Since the majority of patients suspected to have HIT have low 4T scores, reserving testing and empiric therapy for patients with intermediate and high 4T scores can lead to significant cost savings, and avoidance of potentially devastating bleeding complications with DTI therapy.
| 4T score . | Low 0-3 . | Intermediate 4-5 . | High 6-8 . |
|---|---|---|---|
| Number of patients (n)=165 | 107 | 46 | 12 |
| Mean OD | 0.133 | 0.381* | 0.862** |
| Percentage of positive HIT Ab | 0 | 21.7* | 41.7* |
| 4T score . | Low 0-3 . | Intermediate 4-5 . | High 6-8 . |
|---|---|---|---|
| Number of patients (n)=165 | 107 | 46 | 12 |
| Mean OD | 0.133 | 0.381* | 0.862** |
| Percentage of positive HIT Ab | 0 | 21.7* | 41.7* |
p<0.05 compared to Low 4T Score category
p=0.05 compared to Low 4T Score category
| 4T Score . | OD>0.4* . | OD<0.4 . | Total . |
|---|---|---|---|
| 4T ≥ 4 | 15 | 43 | 58 |
| 4T ≤ 3 | 0 | 107 | 107 |
| Total | 15 | 150 | 165 |
| Sensitivity =1.0 | Specificity =0.71 | Positive Predictive Value =0.26 | Negative Predictive Value=1.0 |
| 4T Score . | OD>0.4* . | OD<0.4 . | Total . |
|---|---|---|---|
| 4T ≥ 4 | 15 | 43 | 58 |
| 4T ≤ 3 | 0 | 107 | 107 |
| Total | 15 | 150 | 165 |
| Sensitivity =1.0 | Specificity =0.71 | Positive Predictive Value =0.26 | Negative Predictive Value=1.0 |
OD>0.4 and has significant inhibition with high-dose heparin
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.