Abstract
Abstract 1549
Poster Board I-572
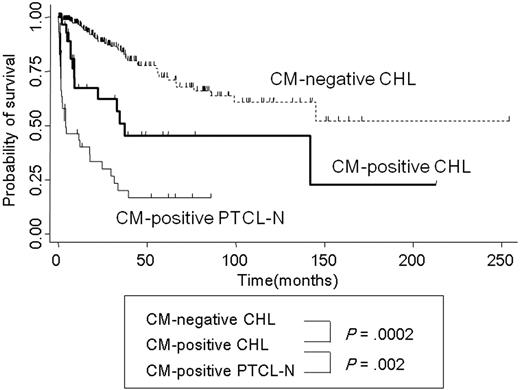
Classical Hodgkin lymphoma (CHL) is characterized by Hodgkin and Reed Sternberg (H-RS) cells, which are B-cell origin in many cases. Recently, we highlighted an adverse prognostic significance of cytotoxic molecule (CM) expression among CHL patients (Asano N, et al. J Clin Oncol. 2006). However, the clinical characteristics of CM-positive CHL still remain controversial. We here document the clinicopathologic profiles of 35 patients with CM-positive CHL, consisting of 23 men and 12 women with a median age of 50 years (range, 16 - 84 years). All patients had lymphoadenopathy, and 14 cases showed mediastinal involvement at presentation. Physical findings included hepatomegaly and splenomegaly in six and five patients, respectively. Four patients had a bulky mass, and nine showed stage IV disease. As for laboratory data, four patients had elevated white blood cell counts (greater than 15.0 × 103/mm3). Anemia (hemoglobin level; less than 10.5 g/dl) was also present in six patients. The pathological diagnoses were nodular sclerosis type (NS) in 22 cases and mixed cellularity (MC) in 12 cases. The H-RS cells of CM-positive CHL had a prototypic immunophenotype of CD15+ CD30+ and Fascin+. All of the cases completely lacked CD20 positivity on H-RS cells, while the expression of CD3e and CD45RO was found in 2 and 1, respectively. The H-RS cells were further positive for EBV RNA transcripts in 14 of 32 (44%) cases studied by in situ hybridization method. All except three cases were negative for Pax5. A clonal TCR-g chain gene arrangement was undetected in any of the cases with successful amplification of control GAPDH DNA by PCR analysis. No cases show B-cell clonality. 27 of 35 patients received systemic multi-agent chemotherapy consisting of first-line treatment regimens as follows: doxorubicin, bleomycin, vinblastine, and dacarbacin (ABVD) (22 patients); cyclophosphamide, doxorubicin, vincristin, and prednisone (CHOP) (2 patients); two with C-MOPP; and one BEACOPP regimens. Three patients died within 6 months, before completing induction treatment because of disease progression. Overall, 22 patients responded to first-line treatment: 13 with complete response and 9 with partial response. 13 of them had relapses, and 8 died with a clinical course ranging from 7 to 142 months. Effective therapeutic approaches should be explored for CM-positive CHL patients, who resist standard treatment for CHL. Comparing CM-positive nodal peripheral T-cell lymphomas of not otherwise specified type (PTCL-N)(n=55) with CM-positive CHL(n=35), no significant differences were detected in clinical parameters except for the frequency of elevated lactate dehydrogenase level in CM-positive PTCL-N. Immunophenotypically, CM-positive CHL cases showed significantly higher rates for CD15, CD30, and Fascin expression, while CM-positive PTCL-N cases showed significantly higher CD3e, CD8, CD45RO, and CXCR3 positivity. The survival curve of CM-positive CHL showed poorer prognosis than that of CM-negative CHL (P = .0002) and better than that of CM-positive PTCL-N (P = .002) (Figure). These findings suggest that CM-positive CHL is characterized by an unfavorable clinical feature, although their histologic and phenotypic features are more suggestive of CHL. Moreover, one case in CM-positive CHL had presented the skin lesion as a CD30-positive lymphoproliferative disorder or an ALK-negative anaplastic large cell lymphoma (ALCL) at the time of recurrence. These findings suggest that CM-positive CHL represent a distinct variant form based on clinicopathologic and phenotypic traits beyond the framework of CHL. Significant overlaps in biologic and morphologic features has been identified in CHL and non-Hodgkin lymphoma. CM-positive CHL cases may be ‘intermediate lymphoma‘ between CHL and PTCL or ALK-negative ALCL. Further studies, including array CGH profiling analysis are needed to clarify the origin of CM-positive CHL.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.