Abstract
Abstract 1666
Poster Board I-692
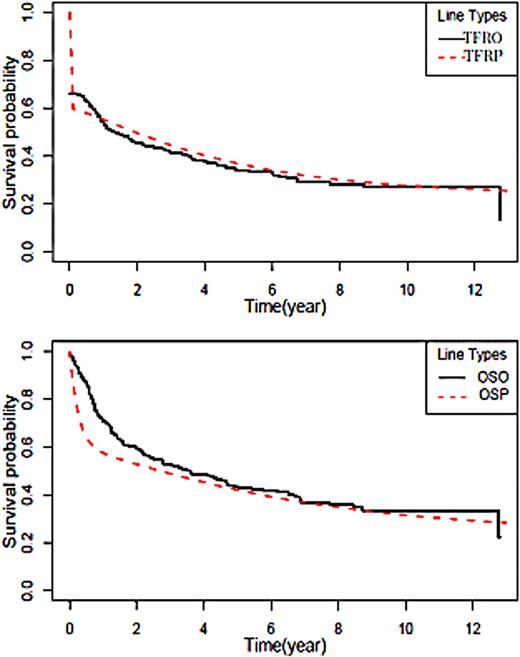
<>Diffuse large B-cell lymphoma (DLBCL) is primarily treated with Rituximab – CHOP immunochemotherapy with varying results. Improved prediction at diagnosis of outcome for an individual patient remains a key goal in DLBCL management. This would allow the selection of patients who could benefit from new therapies. A large amount of data on new immunohistochemical and molecular factors has been collected in the last decade, but the International Prognostic Index (IPI) and Revised IPI are still mostly used for identification of prognostic groups. Both of these indices have important limitations. They rely on a small number of dichotomised predictive variables and patients are assigned to one of a small number of risk groups rather than giving a direct prediction, such as a predictive survival probability or a predictive median lifetime, on a continuous scale for each patient. We have developed a new prognostic index based on Bayesian survival modelling. This has allowed an increase in the number of predictive variables and removal of the need to dichotomise them. Importantly, the new index can give predictions for patients where not all of the predictive variables are observed. It can easily be modified in the future by the addition of new variables, e.g. molecular factors or new treatment regimens. The index was developed using data on a population-based cohort of DLBCL patients prospectively registered with the Scotland and Newcastle Lymphoma Group (SNLG) between 1990 and 2003. The complete data on patients' outcomes were available for 1863 from 2025 registered patients and of this cohort 1391 patients were treated with anthracycline-based chemotherapy and the new index is based on this group. Bayesian statistical inference was used with a three-component Weibull mixture model in which both the hazard multiplier and the component membership probabilities depend on the predictive covariates. The three mixture components correspond to the following three groups: patients who will suffer from primary progressive disease or relapse within one year from diagnosis; patients who will relapse at a later point; those who will have no relapse. A novel method of modelling to deal with cases with missing covariates was used. Both time to first relapse (TFR) and overall survival (OS) were modelled. The following factors were included in the current version of the model: age, sex, performance status by ECOG, clinical stage, B-symptoms, extranodal and bone marrow involvement, Hb, WBC, lactate dehydrogenase, albumin, alkaline phosphatase and urea. The new index is available in the form of a simple computer program and can predict the outcome of patients as: a predicted TFR and OS or a probability of belonging to one of the three groups. In order to check the index, the whole cohort of patients was separated randomly with stratification by IPI into a training-prediction set (2/3 of patients) and a validation-observed set (1/3 of patients). Fig 1 shows the Kaplan-Meyer plots for TRF and OS for both sets. The index was successfully validated. Our new Bayesian prognostic index for DLBCL gives more reliable predictions at diagnosis for individual patients. In future the model can be modified for new treatment regimens or factors. Presently our group is investigating this issue for patients treated with CHOP-R.
Kaplan-Meyer plots for TFR and OS in training-prediction (TFRP and OSP) and validation-observed set (TFRO and OSO).
Kaplan-Meyer plots for TFR and OS in training-prediction (TFRP and OSP) and validation-observed set (TFRO and OSO).
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.