Abstract
Abstract 2581
Poster Board II-558
Tricuspid regurgitant jet velocity (TRJV) measurements are used commonly for estimating pulmonary artery pressures among individuals with sickle cell disease (SCD) undergoing screening for pulmonary hypertension, defined by TRJV ≥ 2.5 m/sec. Measurements, however, may be prone to variability and have not been subjected to reliability testing in this population. The objective of our study was to examine reliability as well as potential sources of variability associated with TRJV measurements in a cohort of children and young adults with SCD.
We evaluated TRJV at steady state in a convenience sample of 30 subjects (53% male) with SCD (SS n=25, SC n=1, S-Beta0 thalassemia n=4) during 2 separate visits 1 week apart. In a blinded fashion, peak TRJV was independently measured by 2 experienced sonographers and officially interpreted by 2 readers who were attending cardiologists at standard time points in the protocol that permitted assessment of reliability and agreement. We calculated within subject variability as well as intra-/inter-sonographer and reader reliability in this analysis using Intraclass Correlation Coefficient (ICC) and Cohen's kappa to assess TRJV as a continuous and categorical variable, respectively. Agreement was also examined graphically using Bland-Altman plots.
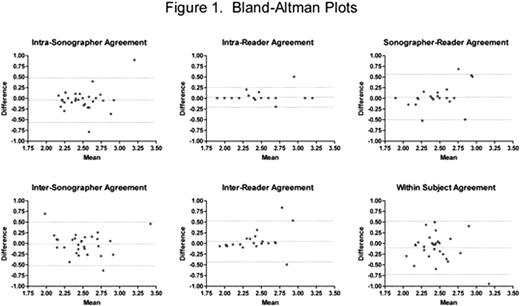
Sonographers were able to measure TRJV in all subjects (mean age, 15.8±3.3 years, range 10 to 22). Readers, however, designated tricuspid regurgitation unquantifiable in 13% of their final interpretations, most commonly due to an inadequate Doppler window. We found that intra-reader reliability was highest (ICC=0.93 [95% CI 0.86, 0.97], p<0.001) and within subject reliability lowest (ICC=0.36 [95% CI 0.02, 0.64], p=0.021) for single TRJV measurements. Inter-reader, intra-/inter-sonographer and between sonographer/reader reliability was in the moderate range, with ICCs that ranged from 0.54 to 0.68. Sonographers and readers also categorized their TRJV measurements and interpretations, respectively, as normal (<2.5 m/s), mild elevation (2.5–2.9 m/s), modest elevation (≥3.0 m/s) or unquantifiable. Using this classification schema, we found that agreement on categories paralleled that on TRJV as a continuous variable. Intra-reader agreement was highest (kappa=0.74 [95% CI 0.53, 0.95], p<0.001) and within subject lowest (kappa=0.14 [95% CI −0.17, 0.46], p=0.38) for TRJV classification, with kappa values ranging from 0.30 to 0.45 for all other combinations of sonographer and reader agreement testing. We plotted absolute differences in sonographer TRJV measurements or reader interpretations against the averages of each pair of values to construct our Bland-Altman graphs (Figure 1). Variability was graphically evident despite finding that only 3.6 to 8.7% of absolute differences fell beyond ±2 standard deviations of the mean difference. For intra- and inter-reader agreement, we observed that absolute differences in readings increased with higher mean TRJV readings.
In summary, quantification of tricuspid regurgitation as well as classification of TRJV values in children and young adults with SCD are affected by several potential sources of variability, including intra-/inter-sonographer and reader differences in measurement and interpretation. Despite using a single sonographer for its determination, within subject reliability in our analysis was especially poor, which may in part reflect sonographer ability to obtain Doppler windows adequate for accurate quantification of tricuspid regurgitation. Our findings underscore the need for methodological improvements that ensure the reliability of measurements used to diagnose TRJV elevation in this population. Multi-institutional reliability testing may also be required to establish the degree of variability that should be considered acceptable in clinical trials involving individuals with SCD and TRJV elevation.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.