Abstract
Abstract 3017
Poster Board II-993
Autoimmune haemolytic anemia (AIHA) of children is a rare and severe condition. Early retrospective series provided the first descriptions, but knowledge is still less than satisfactory. Under a national clinical and biological network, the French Society of Hematology and Immunology (SHIP), in partnership with families (AFSE), conducted from 2004 an observational study of non selected children with AIHA. The aim was to refine epidemiological, clinical and biological data and to identify putative prognostic factors.
Parents gave written informed consent for anonymous data collection. Inclusion criteria were age <18, hemoglobin <11 g/dl, positive Coombs test and haemolysis. Standardized work-up was proposed at initial diagnosis. ES was defined by the synchrone or metachrone association of AIHA and ITP, whatever underlying context was. Dysimmunity was defined by immune deficiency, autoimmune disease, ES or miscellaneousmanifestations. A subclassification heeding familial and personal dysimmunity was proposed. Treatments were prospectively registered. Status of the disease was described as non response (NR), partial response (PR), complete response (CR), and continuous complete response without specific treatment for more than one year (CCR). Kaplan-Meyer method was applied to estimate survival rates in CCR. Potential prognostic variables were assessed using a Cox model. The first 268 patients are described.
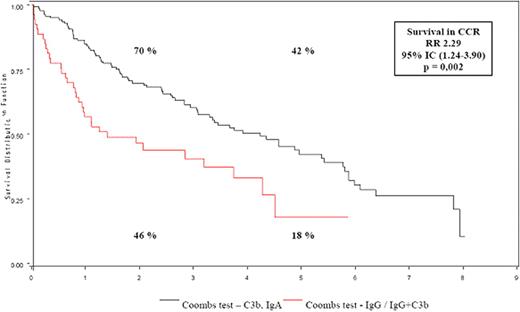
The first 268 children of this cohort, whose AIHA was diagnosed between 1986 and 2007, are described. For the 2003-2007 period, the number of new diagnosis per year ranged from 15 to 35. Median age at diagnosis was 3.8 years. Median hemoglobin level on the first blood count was 6 g/dl. Coombs test was of IgG/IgG+C3b type in 75% of cases. Consanguinity was reported in 8%, first degree familial dysimmunity in 12%, prematurity in 9% of cases. For 53 children, AIHA initial diagnosis was concomitant to a documented infection, mainly EBV (n=11), mycoplasma (n=9), parvovirus (n=6), CMV (n=6). Dysimmunity preceded AIHA in 22% of children, and was diagnosed from the diagnosis of AIHA or in the follow-up in 45% of children. ES was diagnosed in 101 children (37%) : AIHA/ES and isolated AIHA without ITP presentation and outcome significantly differed. In the end of the follow up, all 268 AIHA were subclassified in purely post-infectious in 10%, dysimmune in 52% of cases and primitive in 38%. 92% of children received steroids as first-line therapy.In the end of the first month of disease, CR was obtained for 57% of children. Steroid resistance or high level of steroid dependence led 49% of treated children to receive a median number of 2 (1 to 7) further multimodal therapy, for a median period time of 1.2 years (0 to 21.3). With a 3 year (0.1–21.2) median follow-up, 4% of children died, 30% of alive children were treatment dependant, and AIHA was in PR in 6%, in CR in 50% and in CCR in 40% of cases. In multivariate analysis, Coombs test of IgG/IgG+C3b type was of pejorative value on CCR survival (figure 1).
The present nationwide French cohort is the first large prospective study of non selected children with AIHA reported so far. Heterogeneity of the disease is highlighted, and urge for the need of an etiologic classification dissociating isolated AIHA from AIHA/ES, and the subgroup of AIHA with immune genetic predisposition. Regarding outcome, the only independant prognostic factor is Coombs test type. Chronic course of the disease is not a rare event and warants long term multidisciplinary follow-up. Therapeutic trials should now focus on risk-adjusted sparing steroids and quality of life.
Survival in CCR in 190 children with AIHA diagnosed from January 2000, according to Coombs test type.
Survival in CCR in 190 children with AIHA diagnosed from January 2000, according to Coombs test type.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.