Abstract
Abstract 4626
Red cell exchange (RCE) can be beneficial in the management of patients (pts) with sickling hemoglobinopathies by rapidly reducing hemoglobin (Hb) S levels and raising Hb A levels, thereby decreasing hemolysis and improving organ perfusion. We present 2 pts with sickle beta+ thalassemia (SBT) whose clinical courses were complicated by coexisting warm autoantibody hemolysis and prolonged refractory pain. They had less benefit from RCE than expected due to rapid rebound of Hb S levels and decline in Hb A levels within 48 to 72 hrs after RCE. Each subsequently improved with immunosuppressive therapy.
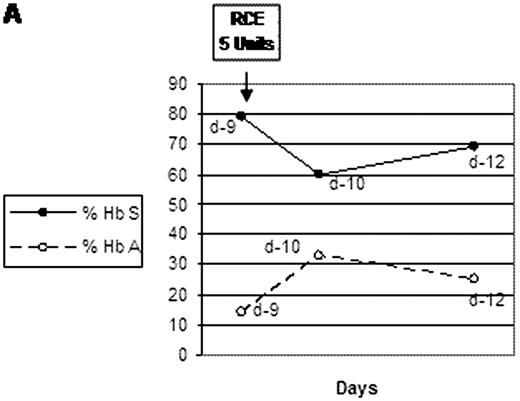
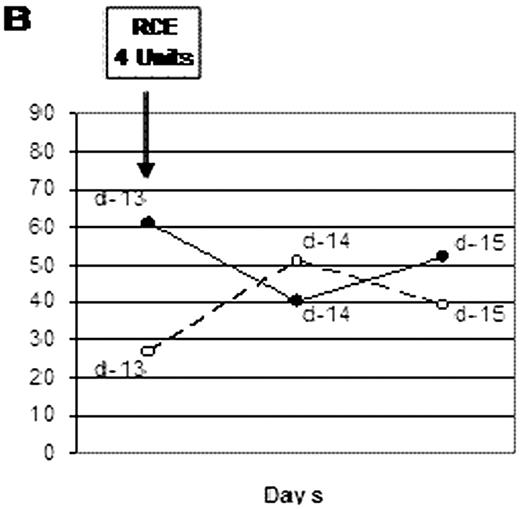
We report 2 African American female pts with SBT who presented with severe anemia, high absolute reticulocyte counts (arc), evident hemolysis, and lack of sustained response of their Hb levels to red cell transfusions. Each had multiple alloantibodies and warm autoantibodies. Patient 1 (see Fig. A), age 34 years, presented with anemia (initial Hb 7.5 g/dL), arc 267 K/μL, and total serum bilirubin (bili) 4.3 mg/dL. Between hospital days 5 and 8, she received 8 units of compatible red cells, but her Hb the next day was only 5.7 g/dL. She then underwent a 5 unit RCE (starting Hb S was 79.3%, Hb A was 14%). Hb S fell to 60.6% the next day; Hb A rose to 33%. Three days post RCE, arc was 854 K/μL, Hb S rose to 68.5%, and Hb A fell to 24.8%. Subsequently intravenous immune globulin (IVIG) was given (48 g per day for 3 days). Her Hb stabilized, began to rise, and she experienced clinical improvement. Patient 2 (see Fig. B), age 36 years, also presented with anemia (Hb 6.8 g/dL), arc 694 K/μL, and bili 2.7 mg/dL. Over the first 10 hospital days she received 3 units of red cells. She was on prednisone (5 mg daily) maintenance for warm autoantibody (IgG) hemolysis. On day 13 a 4 unit RCE was performed. Pre-RCE Hb S was 61.9%, Hb A was 26.9%. Post RCE Hb S was 40.5%, Hb A 50.9%, but 48 hrs post RCE, Hb S level had risen to 52.8% and Hb A fell to 38.8%. Arc was 843 K/μl; Hb was 6.3 g/dL. Prednisone dose was increased to 100 mg per day, and IVIG (2 gm total per kg body weight) was given. Her Hb stabilized and she improved clinically.
Lack of sustained benefit from RCE in these pts likely resulted from 2 factors: (1) high reticulocyte counts, leading to rapid replacement of Hb S cells; and (2) shortened survival of Hb A cells, secondary to their destruction by the warm autoantibodies. Immunosuppressive therapy targeted to the autoimmune component of the anemia provided substantial clinical benefit.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.