Abstract
Naturally occurring CD4+CD25+ regulatory T cells (Tregs) represent a unique T-cell lineage that is endowed with the ability to actively suppress immune responses. Therefore, approaches to modulate Treg function in vivo could provide ways to enhance or reduce immune responses and lead to novel therapies. Here we show that the CD4 binding human immunodeficiency virus-1 envelope glycoprotein gp120 is a useful and potent tool for functional activation of human Tregs in vitro and in vivo. Gp120 activates human Tregs by binding and signaling through CD4. Upon stimulation with gp120, human Tregs accumulate cyclic adenosine monophosphate (cAMP) in their cytosol. Inhibition of endogeneous cAMP synthesis prevents gp120-mediated Treg activation. Employing a xenogeneic graft versus host disease model that has been shown to be applicable for the functional analysis of human Tregs in vivo, we further show that a single dose of gp120 is sufficient to prevent lethal graft versus host disease and that the tolerizing effect of gp120 is strictly dependent on the presence of human Tregs and their up-regulation of cAMP upon gp120-mediated activation. Our findings demonstrate that stimulation via the CD4 receptor represents a T-cell receptor–independent Treg activating pathway with potential to induce immunologic tolerance in vivo.
Introduction
Human naturally occurring regulatory T cells (Tregs) are a thymus-derived subset of T cells representing less than 2% of all peripheral T cells in healthy individuals.1,2 As strikingly illustrated by the development of severe autoimmunity and early death of individuals who lack functional Tregs,3,4 these cells play a critical role in the maintenance of peripheral immunologic tolerance5 by suppressing the activation of other immune cells and conferring regulatory properties upon suppressed T effector cells.6,7 While the suppressive function of Tregs depends on their activation,8 once activated, Tregs suppress other immune cells in a nonspecific manner resulting in a broad and systemic immunoregulatory effect. Consequently, modulation of Treg function could provide ways to enhance or reduce immune responses and thus may lead to novel therapies in humans.9 Efforts to elicit or amplify the regulatory function of Tregs have taken mainly 2 approaches: the isolation and in vitro expansion of Tregs for adoptive transfer10 and the identification of agents that increase the function of Tregs in vivo. The latter approach requires biologicals, such as monoclonal antibodies (mAbs) that either specifically address Tregs or favor Treg activation. Unfortunately, despite improved phenotypical characterization of the human Treg population in recent years,7,11-13 no exclusive surface marker has been defined that allows these cells to be targeted selectively. However, tolerizing methods that have been successfully used in animal models appear to function, at least in part, by increasing Treg activity. One particularly well studied example is the use of anti-CD4 mAbs for tolerance induction in mouse and rat transplantation models.14,15 Initially thought to function solely by depletion or inactivation of CD4+ T cells, anti-CD4-mediated tolerance induction in rodents is now recognized to depend on the activation of Tregs.16,17
Although anti-CD4 mAb-mediated tolerance induction was highly efficient in experimental settings, it has been found to be less successful in clinical trials. This failure has been attributed to many different reasons including pharmacologic problems or an inappropriate selection of outcome criteria. Probably most important, clinical trials using mAbs against CD4 have focused on the inactivation and depletion of inflammatory CD4+ T helper cells18,19 rather than restoration of an immunologic active tolerance through activation of Tregs.
We recently showed that stimulation of human Tregs with certain anti-CD4 mAbs is sufficient to fully activate their suppressive properties,20 suggesting a possible CD4-mediated manipulation of human Tregs for tolerance induction. To further analyze whether CD4 receptor stimulation on Tregs represents a functional Treg activating pathway, we studied the interaction of human Tregs with other CD4-binding molecules. One molecule that binds with particularly high affinity to human CD4 is the human immunodeficiency virus-1 (HIV-1)-1 envelope protein gp120.21 Binding of gp120 to CD4 molecules on CD4+ T cells has been previously shown to result in divergent biologic consequences ranging from partial T-cell activation to induction of apoptosis.22-24 However, these studies were carried out with cell lines and whole CD4 T-cell preparations, and the functional and molecular effects on Tregs have not been addressed so far.
We show here that gp120 upon binding to and signaling through CD4 efficiently activates human Tregs. Exploring the underlying molecular mechanisms, we found that gp120 stimulated Tregs up-regulate cyclic adenosine monophosphate (cAMP), a key event of Treg activation and Treg-mediated suppression.25 Of note, pretreatment of Tregs with an adenylate cyclase inhibitor prevents the induction of suppressive activity by gp120.
using a human equivalent in vivo model of graft-versus-host disease (GVHD) that has been shown to be applicable for the functional analysis of human Tregs in vivo,26 we further show that a single dose of gp120 is sufficient to prevent lethal GVHD and that the tolerizing effect of gp120 is strictly dependent on the presence of human Tregs.
These results disclose CD4 as an attractive target to harness the suppressive potential of Tregs in order to prevent or ameliorate unwanted immune reactions such as in transplantation and autoimmune disorders.
Methods
Mice
NOD-Scid mice were obtained at 1 to 4 days after birth from the central animal facility of the Johannes Gutenberg-University in Mainz. Experiments were performed in accordance with relevant laws (authorization G07-1-016) and institutional guidelines.
Isolation of T cells
Buffy coats and leukapheresis products were obtained from adult healthy volunteers with approval by the local ethical committee (Landesärztekammer Rheinlandpfalz No. 837.029.05 [4687]) at Johannes Gutenberg-University. CD4+CD25+ Tregs, untouched CD4+CD25− T helper cells and CD8+ T cells were isolated as previously described.1,6,27 For some experiments, peripheral blood mononuclear cells (PBMCs) were depleted of Tregs with CD25-Dynabeads (0.5 beads/cell; Invitrogen).
Coculture assay
Resting CD4+CD25+ Tregs were cocultured with syngenic T-cell-depleted PBMC and allogeneic CD8+ T effector cells in the presence or absence of gp120; 105 Tregs were incubated with 3 × 105 irradiated (50 Gy) syngenic T-cell-depleted PBMC in the presence of varying amounts of gp120. Cultures that were stimulated with 0.5 μg/mL anti-CD3 mAbs (clone OKT-3) served as positive control. Either immediately or after 16 hours, 105 allogeneic CD8+ T cells were added to the cultures. Proliferation of alloreactive T effector cells was determined after 3 days of culture by adding 37 kBq/well 3H-TdR for additional 16 hours. Results are expressed as the mean proliferation of triplicates.
Recombinant gp120
The full-length gp120 coding sequence of pSyngp120JR-FL from Dr Eun-Chung Park and Dr Brian Seed28,29 was obtained through the AIDS Research and Reference Reagent Program, Division of AIDS, National Institute of Allergy and Infectious Diseases, National Institutes of Health. Gp120 JR-FL was subcloned into expression plasmid pBI-13, a derivative of pADCMV1,30 and expressed in Chinese hamster ovary (CHO)-DG44 cells.31 Cell-free supernatants of serum-free CHO cell cultures containing soluble gp120 JR-FL were concentrated (240×) using Vivaspin spin columns (Sartorius) with 50-kD MWCO. Supernatants from mock-transfected CHO-DG44 cells treated in a similar manner were used as control (gp120 mock preparation). If not indicated otherwise, gp120 from the CD4- and CCR5-binding HIV-1 strain JR-FL was used for experiments shown. Recombinant gp120 derived from HIV-1 strains that in addition to CD4 bind to CCR5 and CXCR4 (HIV-1 strain MN) or that bind to CD4 and CXCR4 (HIV-1 strain LAV) were obtained from Protein Sciences Corp.
GVHD in NOD-Scid mice
As indicated in the figure legends, different numbers of human PBMC were injected intraperitoneally into newborn NOD-Scid mice alone or together with isolated Tregs or 5 μg gp120. Mice left untreated served as controls. Weight changes were monitored daily. For broncho-alveolar lavage, lungs were lavaged via a tracheal tube with 1-mL phosphate buffered saline. Numbers of human CD45+ cells were assessed by flow cytometry using FITC-conjugated anti-human CD45 mAbs and PE-conjugated anti-human CD3 mAbs. For histology, lungs were fixed and embedded in paraffin. Tissue sections were stained with hematoxylin/eosin (HE) and periodic acid-Schiff (PAS). In addition, human cells were analyzed with anti-human CD45 mAbs. For colitis monitoring, the Coloview high-resolution mouse video endoscopic system was used as described.32 For glutamate pyruvate transaminase (GPT) monitoring, alanine transaminase was quantified in murine sera using the Reflovet Plus system (Scil Animal Care Company). Injection of 107 PBMC resulted in a median time to death of 44 days (range, 35-55) of all treated animals.
Assessment of cAMP production and adenylate cyclase inhibition
To assess cytosolic cAMP concentrations, T cells were washed in ice-cold phosphate buffered saline and lysed in 0.1 N HCl (107/mL), and cAMP was quantified using a cAMP-specific enzyme-linked immunosorbent assay (Correlate EIA Direct cAMP Enzyme Immunoassay Kit, 900-066; Assay Design). MDL-12 (cis-N-(2-Phenylcyclopentyl)azacyclotridec-1-en-2-amine hydrochloride) a cell-permeable inhibitor of adenylate cyclases33 was purchased from Calbiochem (cat. no. 444200) and dissolved in water for injection at a concentration of 6 mM. PP1 (4-amino-5-(4-methylphenyl)-7-(t-butyl) pyrazolo [3,4-d] pyrimidine; Biaffin), a specific inhibitor of src tyrosine kinases, was used at a concentration of 15 μM.
Flow cytometry
Reconstitution and organ infiltration with human cells were determined by analyzing peritoneal exudate cells and splenocytes at indicated time points. Erythrocyte-depleted cells were stained with indicated mAbs. Acquisition was performed on a FACSCalibur, and data were analyzed using CellQuest (BD Biosciences) software.
Statistics
Results represent means plus or minus SE. Statistical significance was determined using the Student t test.
Results
Functional activation of human regulatory T cells by the HIV-1 envelope glycoprotein gp120
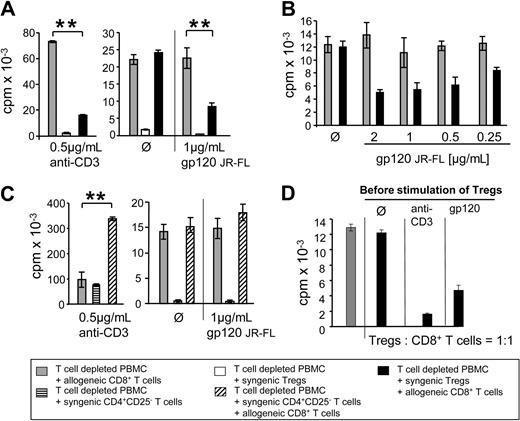
To study the influence of soluble gp120 as a CD4-binding molecule on the function of human Tregs, we cocultured isolated Tregs (supplemental Figure 1, available on the Blood website; see the Supplemental Materials link at the top of the online article) with syngenic T-cell-depleted PBMC in the presence of allogeneic CD8+ T effector cells. In this setting, resting Tregs were not able to suppress the proliferation of alloreactive CD8+ T effector cells without further activation. However, the addition of soluble gp120 dose-dependently resulted in suppressed proliferation in cocultures of Tregs and alloreactive CD8+ T effector cells (Figure 1A-B), suggesting a functional activation of Tregs by gp120. In fact, suppressed proliferation was only observed in the presence of Tregs but not in cultures of alloreactive CD8+ T effector cells without Tregs or in cocultures of alloreactive CD8+ T effector cells and CD4+ T helper cells (Figure 1C). In all experiments, polyclonal stimulation with anti-CD3 mAbs served as a control to verify the functionality of isolated T cells.
gp120-mediated activation of human regulatory T cells. (A) Induction of suppressive activity in human Tregs by recombinant gp120. Tregs were incubated with irradiated syngeneic, T-cell-depleted PBMC and stimulated with 1 μg/mL recombinant gp120 (strain JR-FL). After 16 hours, allogeneic CD8+ T cells were added to the cultures. Cultures without addition (Ø) or stimulated with 0.5 μg/mL anti-CD3 mAbs served as controls. Results represent the mean plus or minus SE (Treg:CD8 ratio 1:1, of 10 experiments; **P < .005). (B) Dose-dependent activation of Tregs by gp120. Experimental setup as under panel A. (C) No induction of suppressive activity in CD4+CD25− T helper cells by gp120, experimental setup as under panel A but with CD4+CD25− T helper cells instead of Tregs. One of 4 experiments (**P < .005). (A-B)  : allogeneic CD8+ T effector cells; □: Tregs, ■: coculture of Tregs and allogeneic CD8+ T effector cells. (C)
: allogeneic CD8+ T effector cells; □: Tregs, ■: coculture of Tregs and allogeneic CD8+ T effector cells. (C)  : allogeneic CD8+ T effector cells; ▤: CD4+CD25− T helper cells; ▨: coculture of CD4+CD25− T helper cells with allogeneic CD8+ T effector cells. (D) Induction of suppressive activity in human Tregs by prestimulation with gp120. Tregs were stimulated with plate-bound gp120 or anti-CD3 mAbs (OKT-3, 1 μg/mL each) or left unstimulated (Ø) for 8 hours. Thereafter, cells were washed and cocultured with T-cell-depleted syngenic PBMC and allogeneic CFSE-labeled CD8+ T cells. Proliferation of alloreactive CD8+ T cells was determined on day 4. Results are representative of 3 experiments.
: allogeneic CD8+ T effector cells; ▤: CD4+CD25− T helper cells; ▨: coculture of CD4+CD25− T helper cells with allogeneic CD8+ T effector cells. (D) Induction of suppressive activity in human Tregs by prestimulation with gp120. Tregs were stimulated with plate-bound gp120 or anti-CD3 mAbs (OKT-3, 1 μg/mL each) or left unstimulated (Ø) for 8 hours. Thereafter, cells were washed and cocultured with T-cell-depleted syngenic PBMC and allogeneic CFSE-labeled CD8+ T cells. Proliferation of alloreactive CD8+ T cells was determined on day 4. Results are representative of 3 experiments.
gp120-mediated activation of human regulatory T cells. (A) Induction of suppressive activity in human Tregs by recombinant gp120. Tregs were incubated with irradiated syngeneic, T-cell-depleted PBMC and stimulated with 1 μg/mL recombinant gp120 (strain JR-FL). After 16 hours, allogeneic CD8+ T cells were added to the cultures. Cultures without addition (Ø) or stimulated with 0.5 μg/mL anti-CD3 mAbs served as controls. Results represent the mean plus or minus SE (Treg:CD8 ratio 1:1, of 10 experiments; **P < .005). (B) Dose-dependent activation of Tregs by gp120. Experimental setup as under panel A. (C) No induction of suppressive activity in CD4+CD25− T helper cells by gp120, experimental setup as under panel A but with CD4+CD25− T helper cells instead of Tregs. One of 4 experiments (**P < .005). (A-B)  : allogeneic CD8+ T effector cells; □: Tregs, ■: coculture of Tregs and allogeneic CD8+ T effector cells. (C)
: allogeneic CD8+ T effector cells; □: Tregs, ■: coculture of Tregs and allogeneic CD8+ T effector cells. (C)  : allogeneic CD8+ T effector cells; ▤: CD4+CD25− T helper cells; ▨: coculture of CD4+CD25− T helper cells with allogeneic CD8+ T effector cells. (D) Induction of suppressive activity in human Tregs by prestimulation with gp120. Tregs were stimulated with plate-bound gp120 or anti-CD3 mAbs (OKT-3, 1 μg/mL each) or left unstimulated (Ø) for 8 hours. Thereafter, cells were washed and cocultured with T-cell-depleted syngenic PBMC and allogeneic CFSE-labeled CD8+ T cells. Proliferation of alloreactive CD8+ T cells was determined on day 4. Results are representative of 3 experiments.
: allogeneic CD8+ T effector cells; ▤: CD4+CD25− T helper cells; ▨: coculture of CD4+CD25− T helper cells with allogeneic CD8+ T effector cells. (D) Induction of suppressive activity in human Tregs by prestimulation with gp120. Tregs were stimulated with plate-bound gp120 or anti-CD3 mAbs (OKT-3, 1 μg/mL each) or left unstimulated (Ø) for 8 hours. Thereafter, cells were washed and cocultured with T-cell-depleted syngenic PBMC and allogeneic CFSE-labeled CD8+ T cells. Proliferation of alloreactive CD8+ T cells was determined on day 4. Results are representative of 3 experiments.
Because CD4 is also expressed on monocytes, the effect of gp120 on the proliferation of alloreactive CD8+ T effector cells in the presence of Tregs could also be indirectly mediated by monocytes. To identify a possible effect of gp120 on Tregs alone, we selectively stimulated Tregs with gp120 before adding them to syngenic T cell–depleted PBMC and allogeneic CD8+ T effector cells as before. As shown in Figure 1D, stimulation of Tregs with gp120 alone is sufficient to induce their suppressive activity.
gp120 binds to CD4 surface molecules on regulatory T cells
HIV-1 envelope glycoprotein gp120 binds with high affinity to CD4 and subsequently to members of the chemokine receptor family.34 To identify the binding site of gp120 essential for the observed Treg activation, we investigated gp120 binding in the presence of the anti-CD4 mAb SK3 that blocks gp120/CD4 interaction.35 Blocking gp120/CD4 interaction prevented the surface binding of gp120 to human Tregs in a dose-dependent manner (supplemental Figure 2), confirming that the CD4 molecule represents the primary binding site. Moreover, similar Treg activation was observed with recombinant gp120 from the dual-tropic (CCR5- and CXCR4-binding) HIV-1 strain MN and the CXCR4-binding HIV-1 strain LAV (supplemental Figure 2), indicating that Treg activation by gp120 is not dependent on coreceptor binding.
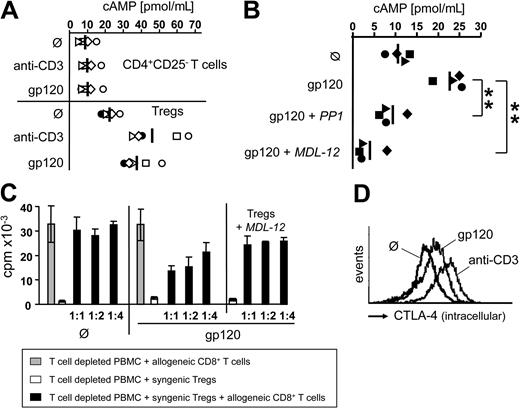
gp120-mediated activation of human regulatory T cells results in up-regulation of cAMP
We analyzed the expression of regular T-cell activation markers and Treg associated markers in Tregs upon gp120-mediated activation. However, neither activation markers such as CD69 or CD25 nor Treg-associated molecules such as GITR and Foxp3 were found to be regulated upon gp120-mediated activation (not shown). Although CTLA-4 surface expression was not altered by gp120 activation, intracellular CTLA-4 expression was increased (Figure 2D), reflecting the functional activation of human Tregs.
gp120-mediated regulatory T-cell activation depends on cAMP production and adenylate cyclase activity. (A) gp120 induces cytosolic cAMP production in human Tregs. Tregs were stimulated with gp120 or anti-CD3 mAbs for 10 hours, and cytosolic cAMP concentration was assessed by enzyme-linked immunosorbent assay (detection limit: 0.75 pmol/mL). Results of 5 individual donors are shown, represented by individual symbols. (B) Inhibition of the tyrosine kinase Lck by the inhibitor PP1 (15 μM) or inhibition of adenylate cyclase activity by the inhibitor MDL-12 (50 μM) prevent gp120-mediated cAMP production in Tregs. Each symbol represents 1 individual donor (**P < .005). (C) Blockade of adenylate cyclase activity holds off gp120-mediated Treg activation. Tregs were either preincubated with MDL-12 for 30 minutes or left untreated and subsequently washed and added to a coculture assay described in Figure 1. One representative result of 3 is shown. Ratios indicate numbers of Tregs to CD8+ T cells. (D) gp120-stimulated Tregs up-regulate intracellular CTLA-4 expression. Tregs were stimulated with gp120 or anti-CD3 mAbs for 10 hours, fixed, permealized, and stained for intracellular expression of CTLA-4.
gp120-mediated regulatory T-cell activation depends on cAMP production and adenylate cyclase activity. (A) gp120 induces cytosolic cAMP production in human Tregs. Tregs were stimulated with gp120 or anti-CD3 mAbs for 10 hours, and cytosolic cAMP concentration was assessed by enzyme-linked immunosorbent assay (detection limit: 0.75 pmol/mL). Results of 5 individual donors are shown, represented by individual symbols. (B) Inhibition of the tyrosine kinase Lck by the inhibitor PP1 (15 μM) or inhibition of adenylate cyclase activity by the inhibitor MDL-12 (50 μM) prevent gp120-mediated cAMP production in Tregs. Each symbol represents 1 individual donor (**P < .005). (C) Blockade of adenylate cyclase activity holds off gp120-mediated Treg activation. Tregs were either preincubated with MDL-12 for 30 minutes or left untreated and subsequently washed and added to a coculture assay described in Figure 1. One representative result of 3 is shown. Ratios indicate numbers of Tregs to CD8+ T cells. (D) gp120-stimulated Tregs up-regulate intracellular CTLA-4 expression. Tregs were stimulated with gp120 or anti-CD3 mAbs for 10 hours, fixed, permealized, and stained for intracellular expression of CTLA-4.
As we recently showed that activated Tregs up-regulate cAMP levels in their cytosol,25 we analyzed the influence of gp120 stimulation on the cAMP content of human Tregs. Similar to CD3-mediated activation, gp120 stimulation induced a strong up-regulation of cytosolic cAMP in human Tregs not detectable in CD4+ T helper cells (Figure 2A).
Because the intracellular part of the CD4 molecule on T cells interacts with tyrosine kinases of the src family, particularly p56lck, we asked whether Lck is critically involved in gp120-mediated Treg activation. Interestingly, inhibition of Lck by treatment with the inhibitor PP1 suppressed cAMP up-regulation in gp120-stimulated Tregs (Figure 2B), supporting the view that gp120 activates human Tregs by binding to CD4 on their surface.
To further assess the functional significance of the cAMP pathway in gp120-mediated Treg activation, we blocked cAMP production in Tregs by preincubation of the cells with a nontoxic concentration of the irreversible adenylate cyclase inhibitor MDL-12. Blocking of adenylate cyclases not only efficiently repressed cAMP up-regulation (Figure 2B) but abrogated suppressor activity in gp120-stimulated Tregs (Figure 2C), demonstrating that cAMP up-regulation is crucial for the gp120-mediated suppressive capacity of human Tregs.
Regulatory T cells control a lethal GVHD induced by human PBMC in immunodeficient NOD-scid mice
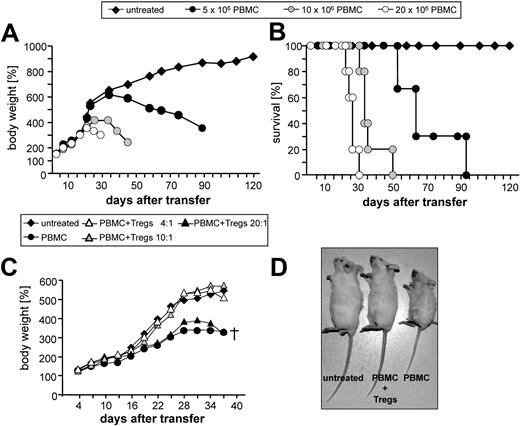
To investigate the potential Treg-modulating capacity of gp120 in vivo, we used a well-established xenogeneic GVHD model26,36 based on the transfer of human immune cells into immunodeficient mice. Intraperitoneal injection of human PBMC into newborn NOD-Scid mice resulted in development of a lethal GVHD leading to death after 30 to 90 days, depending on the number of transferred PBMCs (Figure 3A-B). GVHD was characterized by decelerated growth, reduced body weight, reduced mobility, and ruffled fur with a total mortality greater than 95% within 2 months. In this model, GVHD onset was not affected by the limited number of Tregs transferred within the PBMC; however, cotransfer of resting human Tregs in ratios between 4:1 and 10:1 (PBMC: Tregs) prevented all signs of GVHD (Figure 3C), signifying that this human/mouse chimeric animal model is in general applicable for the functional analysis of human Tregs in vivo. Comparable with published observations, Treg ratios lower than 10:1 were not effective.26
Induction of GVHD in NOD-Scid mice by human PBMC and protection from GVHD by human regulatory T cells. (A-B) Different numbers of human PBMC as indicated were injected into newborn NOD-Scid mice. Untreated mice served as controls (n = 3). (A) Cumulative mean weight data; (B) survival of individual groups. Data from 1 representative experiment of 3 is shown. (C) Protection from GVHD by human Tregs. Newborn NOD-Scid mice were transferred with 107 PBMC with or without graded numbers of Tregs. Each point represents the cumulative mean weight data of 4 mice per group. Survival of mice at day 37: untreated: 4/4; PBMC: 0/4; PBMC + Tregs 4:1: 4/4; PBMC + Tregs 10:1: 4/4; and PBMC + Tregs 20:1: 0/4. (D) Littermates 4 weeks after transfer of 107 PBMCs with or without 2.5 × 106 Tregs or untreated.
Induction of GVHD in NOD-Scid mice by human PBMC and protection from GVHD by human regulatory T cells. (A-B) Different numbers of human PBMC as indicated were injected into newborn NOD-Scid mice. Untreated mice served as controls (n = 3). (A) Cumulative mean weight data; (B) survival of individual groups. Data from 1 representative experiment of 3 is shown. (C) Protection from GVHD by human Tregs. Newborn NOD-Scid mice were transferred with 107 PBMC with or without graded numbers of Tregs. Each point represents the cumulative mean weight data of 4 mice per group. Survival of mice at day 37: untreated: 4/4; PBMC: 0/4; PBMC + Tregs 4:1: 4/4; PBMC + Tregs 10:1: 4/4; and PBMC + Tregs 20:1: 0/4. (D) Littermates 4 weeks after transfer of 107 PBMCs with or without 2.5 × 106 Tregs or untreated.
A single administration of soluble gp120 completely prevents GVHD induction
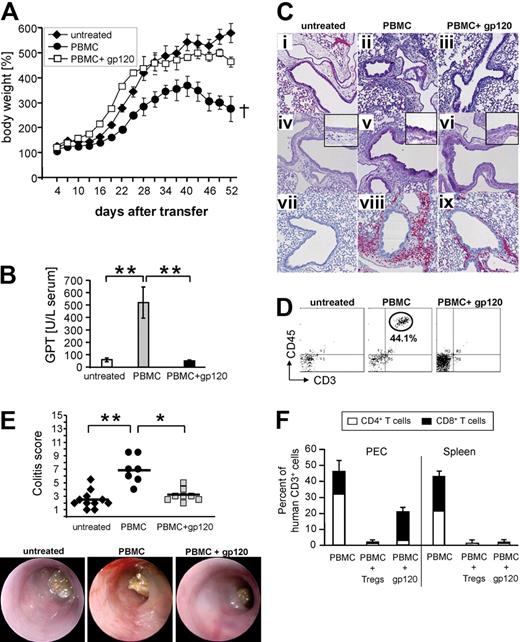
Because HIV-1 envelope glycoprotein gp120 showed potent Treg-activating capacity in vitro and the xenogeneic GVHD model proved to be useful for analyzing the suppressive function of human Tregs in vivo, we investigated the Treg-modulating activity of gp120 in this animal model. To this end, we injected 107 PBMC with or without gp120 into newborn NOD-Scid mice. Notably, a single administration of 5 μg gp120 completely prevented all phenotypic signs of GVHD without transfer of additional Tregs (Figure 4A). This tolerance-inducing potential was observed with recombinant gp120 from CXCR4-binding and CCR5-binding HIV-1 strains as well as with purified native gp120 from the CXCR4-binding HIV-1IIIB strain (not shown). To more closely examine the clinical symptoms of GVHD, we additionally analyzed the concentration of GPT as an indicator of GVHD-mediated hepatitis in the serum of mice.37 Mice engrafted with PBMC showed a significant increase in GPT production 3 weeks after onset of disease. Again, coadministration of gp120 prevented GVHD-mediated hepatitis and the increased production of GPT (Figure 4B). Similar to allogeneic GVHD, development of xenogeneic GVHD was accompanied by massive inflammatory infiltration in the lung and liver of mice engrafted with human PBMC. Histology of lungs collected on day 28 after PBMC injection showed a strong infiltration of human mononuclear cells, peribronchial and perivascular inflammation, and increased mucus production (Figure 4C). In addition, transfer of human PBMC led to significant infiltration of human T cells in the alveolar space as assessed by bronchoalveolar lavage. Treatment with gp120 significantly decreased lung inflammation as well as the number of infiltrating human T effector cells (Figure 4C-D). Colonoscopy performed with a high-resolution mouse video endoscopic system32 revealed signs of a GVHD-associated colitis as indicated by the presence of loose stool, loss of bowel wall translucency, and friable mucosa (Figure 4E). In contrast, coadministration of gp120 also suppressed development of colitis (Figure 4E), underlining the tolerizing potential of gp120 in vivo. Taken together, coadministration of a single dose of gp120 strongly reduced all signs of the severe chronic inflammation seen in mice engrafted with human PBMC.
gp120 protects from GVHD. (A) 107 PBMC were injected with or without 5 μg gp120 into newborn NOD-Scid mice. Untreated mice served as controls. Each point represents the cumulative mean weight data of one group (5 mice per group; one of 5 experiments is shown). Survival of mice at day 52: untreated: 5/5; PBMC: 0/5; and PBMC + gp120: 5/5. (B) GTP serum levels of mice belonging to different groups 3 weeks after PBMC transfer. (C) Histologic pulmonary tissue analysis 4 weeks after PBMC transfer. (D) Representative flow cytometric analysis of bronchoalveolar lavage from mice belonging to different groups 3 weeks after PBMC transfer. (E) Colitis score and endoscopic pictures of mice belonging to different groups of mice 3 weeks after PBMC transfer. (F) Regulatory T cells and gp120 inhibiting expansion of human T effector cells in lymphoid tissues. Frequencies of human CD45+ leukocytes and the CD4:CD8 T-cell ratios in the CD45+ population 28 days after PBMC transfer are shown. Columns and error bars indicate average expression plus or minus SD of 3 different mice. One representative result of 3 is shown.
gp120 protects from GVHD. (A) 107 PBMC were injected with or without 5 μg gp120 into newborn NOD-Scid mice. Untreated mice served as controls. Each point represents the cumulative mean weight data of one group (5 mice per group; one of 5 experiments is shown). Survival of mice at day 52: untreated: 5/5; PBMC: 0/5; and PBMC + gp120: 5/5. (B) GTP serum levels of mice belonging to different groups 3 weeks after PBMC transfer. (C) Histologic pulmonary tissue analysis 4 weeks after PBMC transfer. (D) Representative flow cytometric analysis of bronchoalveolar lavage from mice belonging to different groups 3 weeks after PBMC transfer. (E) Colitis score and endoscopic pictures of mice belonging to different groups of mice 3 weeks after PBMC transfer. (F) Regulatory T cells and gp120 inhibiting expansion of human T effector cells in lymphoid tissues. Frequencies of human CD45+ leukocytes and the CD4:CD8 T-cell ratios in the CD45+ population 28 days after PBMC transfer are shown. Columns and error bars indicate average expression plus or minus SD of 3 different mice. One representative result of 3 is shown.
gp120 treatment suppresses T effector cell activation comparable with increased regulatory T-cell ratios
Next we investigated the ratios of human T effector cells in the peritoneum and spleen of mice injected with 107 PBMC, 107 PBMC plus additional Tregs (4:1), or 107 PBMC with 5 μg gp120. Mice that received only PBMC developed lethal GVHD associated with high levels of human CD4+ and CD8+ T effector cells in the peritoneum and spleen (Figure 4F). Adoptive transfer of Tregs significantly inhibited this accumulation of T effector cells in both organs. This result is consistent with previous observations in allogeneic GVHD models demonstrating that increased ratios of Tregs were able to control T-cell activation against the recipient.38-40 In line with our previous finding, a single dose of gp120 also inhibited the accumulation of human T effector cells in the peritoneum and spleen. However, both higher ratios of Tregs as well as administration of gp120 completely prevented all clinical signs of GVHD associated with significantly reduced expansion of CD4+ effector cells in lymphoid tissues, confirming that gp120 is capable of activating Tregs in vivo.
Human regulatory T cells are mandatory for the suppressive function of gp120 in vivo
Because gp120 does not bind to murine CD4,41 the observed effect was exclusively dependent on interaction with human immune cells. Interestingly, the protective effect of gp120 was similar to the transfer of additional Tregs (Figure 4F), suggesting that gp120—similar to its activity in vitro—suppresses GVHD by activating the intrinsic Tregs present in PBMC. However, because the interaction of gp120 with human Tregs is not selective and does not preclude an interaction of gp120 with CD4-expressing T-helper cells and monocytes, alternatively, the observed effect might have been the result of other regulatory or blocking activities on the transferred human cells. To test these alternatives, we engrafted newborn NOD-Scid mice with Treg-depleted PBMC (supplemental Figure 3), with or without coadministration of gp120. Although mice injected with Treg-depleted PBMC did not develop significantly faster or higher-grade GVHD in absence of Tregs, GVHD could not be prevented by an additional administration of gp120 (Figure 5A-B), demonstrating that the tolerogenic effect of gp120 treatment is Treg-dependent and cannot be explained by direct inhibition of CD4+ T effector cells.
Tolerogenic function of gp120 in vivo is regulatory T-cell-dependent. (A) 107 Treg-depleted PBMC with or without 5 μg gp120 were injected into newborn NOD-Scid mice. Untreated mice served as controls. Each point represents the cumulative mean weight data of 5 mice per group (1 of 5 experiments is shown). Bars represent SEM. Survival of mice at day 43: untreated: 5/5; CD25-depleted PBMC: 0/5; and CD25-depleted PBMC + gp120: 0/5. (B) GTP serum levels of mice belonging to different groups 3 weeks after PBMC transfer. (C) Inhibition of adenylate cyclases in Tregs abrogates the tolerogenic function of gp120 in vivo. PBMCs (107) containing 3% syngenic Tregs either left untreated (Tregs) or pretreated with the adenylate cyclase inhibitor MDL-12 (50μM) for 30 minutes (Tregs*) were injected into newborn NOD-Scid mice with or without 5 μg gp120. Untreated mice served as controls. Each point represents the cumulative mean weight data of 3 mice per group (1 of 2 experiments is shown). Bars represent SEM. Survival of mice at day 52: untreated: 5/5; PBMC with untreated Tregs: 0/5; PBMC with untreated Tregs + gp120: 5/5; PBMC with MDL-12–treated Tregs: 0/5; and PBMC with MDL-12–treated Tregs + gp120: 0/5.
Tolerogenic function of gp120 in vivo is regulatory T-cell-dependent. (A) 107 Treg-depleted PBMC with or without 5 μg gp120 were injected into newborn NOD-Scid mice. Untreated mice served as controls. Each point represents the cumulative mean weight data of 5 mice per group (1 of 5 experiments is shown). Bars represent SEM. Survival of mice at day 43: untreated: 5/5; CD25-depleted PBMC: 0/5; and CD25-depleted PBMC + gp120: 0/5. (B) GTP serum levels of mice belonging to different groups 3 weeks after PBMC transfer. (C) Inhibition of adenylate cyclases in Tregs abrogates the tolerogenic function of gp120 in vivo. PBMCs (107) containing 3% syngenic Tregs either left untreated (Tregs) or pretreated with the adenylate cyclase inhibitor MDL-12 (50μM) for 30 minutes (Tregs*) were injected into newborn NOD-Scid mice with or without 5 μg gp120. Untreated mice served as controls. Each point represents the cumulative mean weight data of 3 mice per group (1 of 2 experiments is shown). Bars represent SEM. Survival of mice at day 52: untreated: 5/5; PBMC with untreated Tregs: 0/5; PBMC with untreated Tregs + gp120: 5/5; PBMC with MDL-12–treated Tregs: 0/5; and PBMC with MDL-12–treated Tregs + gp120: 0/5.
Blockade of adenylate cyclase activity in Tregs abrogates the tolerizing effect of gp120
It is recognized that in vivo and in vitro functional properties of Tregs are not necessarily identical. Because blocking of adenylate cyclases abrogated suppressor activity in gp120-stimulated Tregs in vitro (Figure 2C), we analyzed the role of adenylate cyclase activity in the regulatory function of Tregs in vivo. To this end, Tregs pretreated with the adenylate cyclase inhibitor MDL-12 or left untreated were added back to syngenic PBMC in physiologic numbers. The resulting “recomposed” PBMC were engrafted into newborn NOD-Scid mice, with or without coadministration of gp120. As shown in Figure 5C, gp120 could not prevent GVHD onset in the presence of MDL-12 treated Tregs, indicating that adenylate cyclase activity is required for the gp120-mediated suppressive activity of human Tregs in vivo.
Discussion
The data presented provide evidence that (1) HIV-1 envelope protein gp120 functionally activates human Tregs by binding to CD4 surface molecules and transmitting signals into the cell involving tyrosine kinases of the src family, (2) gp120 stimulation induces adenylate cyclase activity leading to elevation of cytosolic cAMP levels in Tregs, and (3) functional activation of human Tregs with soluble gp120 prevents the development of lethal GVHD induced by injection of human PBMC into immunodeficient NOD-Scid mice. These observations are even further corroborated by the findings that (4) the prevention of GVHD by gp120 strictly depends on the presence of Tregs and (5) the inhibition of adenylate cyclases in Tregs abrogates gp120-mediated tolerance induction in vivo.
Along with our previous observation that certain anti-CD4 mAbs have the potential to induce the suppressive function in isolated human Tregs in a T cell receptor-independent manner,20 the current results uniquely demonstrate that stimulation via the CD4 receptor represents a functional Treg-activating pathway. These findings are consistent with several studies, which assumed that gp120-CD4 interaction in HIV-infected individuals might increase the functional activity of Tregs.42,43 However, in HIV-infected patients gp120-specific effects cannot be separated from other effects of the virus on Treg function.
In contrast to our observations, at least one study suggested that the regulatory activity of human Tregs is not activated by HIV-1 envelope proteins in vitro.44 Most likely, the discrepancy between our observations and those of Hu et al might be caused by differences in the in vitro assay used. Whereas in our study Tregs were stimulated with gp120 only, Hu et al prestimulated Tregs with HIV-1 envelope proteins but subsequently stimulated the cells with anti-CD3 and IL-2 and therefore most likely outplayed CD4-mediated signals by a strong T-cell receptor signal.44
Examining the signaling events, which were affected directly by CD4 engagement on human Tregs, we demonstrate that CD4-stimulation increases cAMP production in Tregs but not in CD4+CD25− T cells. This observation is in agreement with the previous observation that the expression of the cAMP-degrading phosphodiesterase PDE3b is reduced in Tregs.45,46 It is further corroborated by a paper from Huang et al, who showed that miR-142-3p limits the level of cAMP in CD4+CD25− T cells, whereas Foxp3 down-regulates miR-142-3p and keeps the cAMP pathway in Tregs active.47 By evaluating the functional significance of the cAMP pathway, we show that adenylate cyclase activity is required for the CD4-mediated activation of human Tregs in vitro and in vivo, confirming the functional significance of the cAMP pathway in Treg activation and Treg-mediated suppression.25 Our observation that CD4-stimulated Tregs do not up-regulate activation markers on their surface but show an increased intracellular expression of CTLA-4 is in keeping with the observation reported by Vendetti et al that increased cAMP levels lead to an up-regulation of CTLA-4 expression in human CD4+ T cells in the absence of the up-regulation of CD69 and CD25 activation markers.48
Induction of xenogeneic GVHD by human PBMC in immunodeficient mice represents a robust model for studying human Treg functions in vivo.26,36 Using this experimental model, we show here that administration of gp120 is as effective in controlling GVHD as the transfer of increased Treg ratios. Presumably, the transfer of human Tregs into a xenogeneic environment only activates a limited number of these cells and therefore only strongly raised numbers of transplanted Tregs are able to control GVHD onset. On the other hand, gp120 provides a polyclonal stimulus enabling limited numbers of transplanted Tregs to suppress the activation of xenoreactive T cells.
Extensive studies have demonstrated that gp120 has diverse effects on CD4+T cells.22-24 However, these effects were mostly observed in vitro, and it is less clear how gp120 influences cellular functions in vivo. We show here that in the GVHD model the tolerizing effect of gp120 depends on the presence of human Tregs and appears to function by increasing Treg activity. Other potential effects, such as direct CD4-mediated suppression of T helper cells, cannot be excluded44 ; however, they do not seem to play an essential role as outlined by the inability of gp120 to repress GVHD induction in the absence of Tregs.
Our findings contrast with a previous study, which concluded that the depletion of CD25+ cells from infused human PBMC significantly exacerbates the symptoms and accelerates the lethality of xenogeneic GVHD.26 However, in this study, not only Tregs but also CD8+CD25+ T cells, CD25+ B cells, and CD4+ cells expressing intermediate CD25 levels were depleted from PBMC. By contrast, upon selectively removing CD4+CD25+Foxp3+ Tregs from PBMC (Figure S3), we did not observe significantly altered GVHD onset or severity (Figure 5).
One important context in which interventions to modulate Tregs may be used is allogeneic hematopoietic stem cell transplantation (HSCT). Several clinical studies suggested that after HSCT Treg activity plays an important role in controlling alloimmunity and preventing GVHD.49,50 Although a xenoreactive T-cell response is less strong than an alloreactive response, our observation that gp120-activated Tregs are able to prevent the induction of a xenogenic GVHD response suggests the use of gp120 as a tolerizing treatment in allogeneic HSCT.
Together, our findings demonstrate that stimulation via the CD4 receptor represents an alternative Treg activating pathway with potential to induce immunologic tolerance in vivo.
An Inside Blood analysis of this article appears at the front of this issue.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors are grateful to Drs S. Stoll, E. von Stebut-Borschitz, U. Kalinke, and D. Kabelitz for critical reading of the manuscript and helpful discussions. We thank L. Paragnik, S. Fondel, and P. Hoelter for their expert technical assistance.
This work was supported by the Deutsche Forschungsgemeinschaft, grants A8 SFB-548 and A2 TR52 (H.J.), A11 SFB 548 (C.T.), A1 TR52 (T.B. and E.S.), the Carl Zeiss Foundation (T.B.), and A6 SFB 548 (E.S.).
Authorship
Contribution: Christian Becker designed and performed research, analyzed data, and wrote the paper; C.T. designed and performed research and analyzed data; T.B. designed and performed research, analyzed data, and wrote the paper; Christoph Becker performed research and analyzed data; K.M. performed research; J.K. performed research; S.R. performed research; N.D. performed research; M.F.N. designed research; K.R. performed research; F.-J.S. contributed vital new reagents; E.S. designed research; and H.J. designed research and wrote the paper.
Conflict-of-interest disclosure: F.J.S., Christian Becker, E.S., T.B., and H.J. have financial interests in the therapeutic activation of Tregs consisting of a patent application. In addition, E.S. and H.J. receive research support from Boehringer Ingelheim Pharma GmbH and Co KG. F.J.S. is an employee of Boehringer Ingelheim Pharma GmbH and Co KG. The remaining authors declare no competing financial interests.
Correspondence: Dr Christian Becker, Department of Dermatology, Johannes Gutenberg-University, Langenbeckstr 1, D-55101 Mainz, Germany; e-mail: christian.becker@hautklinik.klinik.uni-mainz.de.