In this issue of Blood, Rand and colleagues have shown that in vitro hydroxychloroquine can reverse antiphospholipid antibody-mediated disruption of the annexin VA crystalline shield that protects phospholipid bilayers from taking part in coagulation reactions.1 The protective effect of hydroxychloroquine against antiphospholipid antibody-induced damage was seen on both cultured endothelial cells and a syncytialized trophoblast cell line.
Since the discovery of antiphospholipid antibodies (aPLs) and their associated thrombotic and pregnancy complications nearly 30 years ago, we have learned an enormous amount about the clinical manifestations of antiphospholipid syndrome, while animal and in vitro work has developed possible models of pathogenesis. However, there have been no major advances in treatment. We remain heavily reliant on anticoagulation in preventing both aPL-related thromboses and pregnancy morbidity. Both patients and physicians alike struggle with the stresses and strains of managing anticoagulant monitoring and the risks of major bleeding, especially with the oral vitamin K antagonists. The current hope is that the new oral fixed-dose anticoagulants will bring better efficacy, safety, and ease of use.
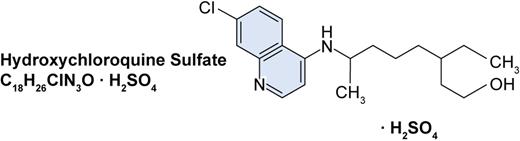
The structure of hydroxychloroquine sulphate. Professional illustration by Paulette Dennis.
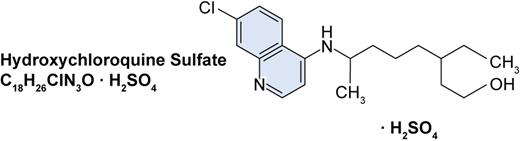
The structure of hydroxychloroquine sulphate. Professional illustration by Paulette Dennis.
Current models of how aPLs cause damage are sophisticated. But, it can be argued that up to now, no single pathogenic model can both have the potential to be applicable to all the heterogeneous types of aPL and explain the primary moments of how aPL produces changes that activate coagulation. This lack of understanding of how aPLs cause damage prevents the development of novel agents to tackle the antibody head on. Rand et al's hypothesis that the primary damaging event of aPLs is to disrupt the annexin A5 shield is a plausible mechanism to explain all the phenotypes of antiphospholipid syndrome, for the shield is present on the cell types (such as endothelium, platelet, and trophoblast) affected by aPL. If this hypothesis holds true, then hydroxychloroquine is possibly the first treatment targeted at the mechanism of action of the antibody, that is, a treatment that could “block” the primary effects of the antibody, rather than our existing crude approach of using anticoagulation to switch off the downstream effects of aPLs.
Hydroxychloroquine has been available since the 1950s. It is traditionally known as an antimalarial agent, but also is a well-established anti-inflammatory agent used as a first-line treatment for the fatigue, arthralgia, and skin rashes of systemic lupus erythematosus. It has an established safety profile including reassuring data on its use during pregnancy,2 an important consideration in view of the pregnancy morbidity associated with antiphospholipid syndrome.
Hydroxychloroquine has been known to have immunomodulatory effects for a long time. Recent work has shown this is partly or wholly mediated by its effects on inhibiting Toll-like receptors on dendritic cells.3 Interestingly, over the past 10 years, cohort studies of lupus patients have identified that those patients receiving hydroxychloroquine, whether they have antiphospholipid antibodies or not, have a significantly lower risk of thromboses.4-7 Another clue comes from a mouse model of APS in which mice receiving hydroxychloroquine had smaller and shorter-lasting thrombi after injury than those receiving placebo.8 Hydroxychloroquine has been known to mildly inhibit platelet aggregation for a long time, but the effect was not thought to explain its clinical antithrombotics efficacy. So, Rand et al's description of its direct effects against aPL is an interesting alternative.
Of course, no paper is without shortcomings and as attractive as the theory may be, further evidence is required before we can be sure that this is not a false dawn. The described studies, elegant as they are, used aPL from only 3 patients, and the work needs rep-etition with other aPL. Does current treat-ment with hydroxychloroquine attain levels similar to those used in these in vitro studies? Does hydroxychloroquine attain the same effects in patients with aPL without systemic lupus erythematosus?
Certainly, however, the combined evidence from the cohort studies of hydroxychloroquine effect in lupus patients, Rand's work, and a favorable safety profile suggest trials of hydroxychloroquine in the primary and secondary prevention of thrombosis and pregnancy morbidity of aPL are timely. The practical challenge to the community of aPL physicians is to prevent hydroxychloroquine usage slipping into routine clinical practice without first organizing good multicenter clinical trials to assess its true utility.
Conflict-of-interest disclosure: The author declares no competing financial interests. ■