Abstract
In the disorder leukocyte adhesion deficiency III (LAD-III), integrins on platelets and leukocytes are expressed but fail to function and this leads to severe bleeding and infections at an early age. Mutation in the KINDLIN3 (FERMT3) gene is the cause of LAD-III in patients from the Middle East, Malta, and Turkey. We describe 2 novel homozygous mutations in the KINDLIN3 gene of a new African-American patient that destabilize KINDLIN3 mRNA leading to loss of kindlin-3 protein. Transfection of wild-type (WT) KINDLIN3 cDNA restored integrin-related adhesion and migration in the LAD-III patient's T and B lymphocytes. We analyzed the individual mutations separately in vitro to learn more about the function of the kindlin-3 protein. The first G>A mutation gives rise to a Gly308Arg change at the end of FERM (protein 4.1, ezrin, radixin, moesin) subdomain 2, and the second mutation is a base deletion causing early termination within the pleckstrin homology (PH) domain. This second mutation prevented membrane association of kindlin-3 and did not restore either adhesion or migration, whereas the FERM subdomain 2 mutation affected only migration. Thus, these LAD-III patient mutations have highlighted functionally important regions of kindlin-3 that alter leukocyte integrin-dependent function in 2 distinct ways.
Introduction
Integrins are the major adhesion receptors of hematopoietically derived cells. The ability of leukocytes to use the integrins leukocyte function-associated antigen 1 (LFA-1) and α4β1 to leave the circulation and migrate into tissues is critical for a successful immune response.1,2 Platelets use integrins, particularly αIIbβ3, to bind fibrinogen that is essential for clotting.3 The integrins on circulating leukocytes and platelets normally bind poorly to their ligands, but become active after “inside-out” signaling through other membrane receptors.2,4,5
Important features of the signaling pathway leading to integrin activation are now understood. Diacylglycerol and Ca2+, which are the products of agonist signaling, activate protein kinase C and/or the Rap1 guanine nucleotide exchange factor, CalDAG-GEF1. These proteins promote activation of Rap1 that is brought to the membrane by the adaptor protein Rap1-guanosine triphosphate–interacting adapter molecule (RIAM).6-8 Another critical step involves the recruitment of talin to the RIAM/Rap1 complex, bringing it into position to bind to the β subunit of integrins. This binding stabilizes the conformation of integrin with highest affinity for ligand.9-11
Recently, it has been recognized that the 3 members of the kindlin family are also involved in integrin activity.12,13 Each has a distinctive tissue distribution: kindlin-1, epithelial expression; kindlin-2, muscle and more widespread expression; and kindlin-3, hematopoietic specific. Both talin and the kindlins have similar FERM (protein 4.1, ezrin, radixin, and moesin) domain structures. FERM subdomain 3 of these proteins binds the β subunit of integrins: talin at the membrane-proximal NXXY site and the kindlins at the membrane-distal NXXY site.14-16 The kindlins differ from talin in having a pleckstrin homology (PH) domain inserted into FERM subdomain 2. The standard PH domain has 7 β strands followed by 1 or 2 α helices.17,18 Many investigated PH domains bind phosphoinositides and function as membrane-anchoring structures.19,20
Kindlin-3−/− mice have bleeding and leukocyte adhesion defects, providing compelling evidence for the importance of kindlin-3 in regulating integrin activity.15,16 In terms of human disease, leukocyte adhesion deficiency-III (LAD-III) patients display disrupted platelet and leukocyte function similar to the Kindlin3−/− mice, leading to severe bleeding and infections.21 The hematopoietically derived cells of the LAD-III patients express their integrins at normal levels, but the integrins fail to function because of defective inside-out signaling.22-26 Our group and others have now demonstrated that mutation in the KINDLIN3 gene (also known as FERMT3) is responsible for the human LAD-III disorder.27-30 Five different mutations in the FERM subdomains have been reported in these patients, and all lead to lack of expression of the kindlin-3 protein (also known as FERMT3, UNC-112 related protein 2 [URP2], and mitogen-inducible gene 2B [MIG-2B]). Restoring wild-type (WT) kindlin-3 expression to LAD-III lymphocytes reverses their adhesion defects.27,29 Until now, the patients have been of Turkish, Maltese, or Middle Eastern origins. We describe here for the first time an African-American patient with 2 unique KINDLIN3 mutations that lead to loss of kindlin-3 protein. The mutations compromise kindlin-3 function in different ways when tested individually in in vitro assays, giving greater insight into the role of kindlin-3 in leukocyte adhesion and migration.
Methods
Patient
The patient is an African-American female infant, age 11 months, who displayed a bleeding tendency from birth, including gastrointestinal bleeding and multiple recurrent infections, such as Pneumocystis carinii–like pneumonia, respiratory syncytial virus–like pneumonia, Pseudomonas, and methicillin-resistant Staphylococcus aureus infections, all requiring hospitalization. The patient underwent a successful bone marrow transplantation in November 2008. More complete details of the clinical profile are published elsewhere.31 Approval for studies with the newly reported human primary cells was obtained from the Institute Review Board of Emory University School of Medicine and Children's Healthcare of Atlanta. Informed consent was obtained in accordance with the Declaration of Helsinki.
Antibodies and other reagents
Monoclonal antibodies (mAbs) 38 (αL, CD11a), TS1/18 (β2, CD18), HP2/1 (α4, CD49d), and P5D2 (β1, CD29) have been previously reported.24,32 Other antibodies were affinity-purified rabbit polyclonal serum specific for human kindlin-3 peptide (EPEEELYDLSKVVLA; amino acids 156-170)27 and anti–α-tubulin mAb (Sigma-Aldrich). Horseradish peroxidase–coupled anti–green fluorescent protein (GFP) mAb was purchased from Miltenyi Biotec. Full-length intercellular adhesion molecule-1 Fc (ICAM-1Fc) protein was prepared as previously described.24
Mutation of human KINDLIN3 cDNA
Human KINDLIN3 was obtained by polymerase chain reaction (PCR) from a full-length cDNA clone, IRAUp969A0924D (ImaGenes). A 5′ HindIII site was added using oligonucleotide (oligo) GCCAAGCTTATGGCGGGGATGAAG and a 3′ AgeI site was added using oligo TCAACCGGTCCTGCGAAGGCCTCATGGCC. The PCR product was subcloned into vector pEGFP-N1 (Clontech). The G>A and ΔT mutations were made in WT KINDLIN3-GFP using QuikChange Site-Directed Mutagenesis Kit (Stratagene). Forward and reverse primers containing the sequence CTGTCCCAGAGCAGGGAGGTGGGGG for the G>A mutation and TAGTGCCCTCCCCGAGGGCATGAGT for the ΔT mutation were used. The G>A and ΔT double-mutated construct was made by adding the G>A mutation to ΔT KINDLIN3-GFP using the same oligos and protocol as for WT KINDLIN3. All DNA constructs were verified by sequencing.
Sequencing the KINDLIN3 gene
Genomic DNA from the patient, her mother, and nonrelated controls was analyzed for base changes in all exons and intron-exon boundaries of the KINDLIN3 gene (chr11:63 730 782-63 747 930) by direct DNA sequencing in both orientations. Details are available from the authors.
Cells and cell transfections
T lymphocytes were prepared as previously described.24 Epstein-Barr virus (EBV)–transformed B-lymphoblastoid cells were derived from peripheral blood mononuclear cells of the LAD-III patient by Research Cell Services, Cancer Research UK using standard procedures. Other EBV-transformed nonrelated cell lines, BS, POS, and AY have been reported previously.24,27 All cells were maintained in RPMI-1640 with 10% fetal calf serum.
T lymphoblasts were transfected using the AMAXA Nucleofector, the T-cell kit, and program T-20 according to the manufacturer's instructions (AMAXA). EBV-transformed B cells were washed in OptiMEM+GlutaMAX (Invitrogen) and electroporation was performed using 2 × 107 cells with 10 μg per reaction of human KINDLIN3-GFP, mouse GFP-kindlin3 or pEGFP-N1 (BD Biosciences) cDNA constructs using a Gene Pulser with Capacitance Extender (Bio-Rad) set at 960 μF (microfarads) and 260 mV. Transfected cells were maintained in RPMI 1640/10% fetal calf serum for up to 24 hours. The efficiency of transfection was evaluated by flow cytometry, and the GFP-positive cells were sorted using a MoFlo Cell Sorter (Beckman Coulter). Cells expressing equivalent levels of GFP were compared in migration assays.
Flow cytometry
Leukocytes (5 × 105) were incubated on ice in 50 μL of phosphate-buffered saline/0.2% bovine serum albumin (BSA) containing primary mAb at optimal dilution as described previously.24 Bound mAb was detected with fluorescein isothiocyanate–conjugated goat anti–mouse immunoglobulin G (IgG; Sigma-Aldrich) and analyzed by FACSCalibur (BD Biosciences).
Cell attachment assays
Quantitative reverse-transcription–PCR
The human KINDLIN3 mRNA levels were quantified using TaqMan assay technology. Briefly, RNA was extracted from leukocytes using GenElute Mammalian Total RNA Miniprep Kit (Sigma-Aldrich), reverse-transcribed using the AffinityScript QPCR cDNA Synthesis Kit (Stratagene), and purified using the QIAquick PCR Purification Kit (QIAGEN Ltd). cDNA (40 ng per reaction) was amplified using TaqMan Gene Expression Assays (Applied Biosystems): for KINDLIN3, Hs00258828_m1 (exons 13-14) and Hs01075695_m1 (exons 6-7); for controls, Hs99999905_m1 (GAPDH) and Hs00202782_m1 (SF3B1).
Samples were analyzed on the ABI 7900HT Sequence Detection System instrument. Each sample was run in quadruplicate and expressed as a function of threshold cycle (Ct). The Ct values for reactions amplifying KINDLIN3 were corrected by the Ct value for 2 housekeeping genes, SF3B1 and GAPDH, to give ΔCt. The difference in ΔCt values between test and control cDNA samples allowed the relative expression of the gene to be quantified as: 2Λ[(ΔCt test − ΔCt control)] (Applied Biosystems).
Immunoblotting
Cells (5 × 107) were lysed in 0.5 mL of buffer (1% Triton X-100, 50mM tris(hydroxymethyl)aminomethane base [pH 7.5], 150mM NaCl, and complete protease inhibitor cocktail [Roche Diagnostics Ltd]). Cell lysate proteins were reduced in 2× Laemmli buffer and separated using precast 3% to 8% sodium dodecyl sulfate–polyacrylamide gel electrophoresis gels (Invitrogen), then transferred to polyvinylidene fluoride membrane (Immobilon-P; Millipore). Blots were probed with primary antibodies as specified and detected with goat anti–rabbit IgG horseradish peroxidase (Dako) or sheep anti–mouse IgG horseradish peroxidase and enhanced chemiluminescence detection reagents (GE Healthcare).
Video microscopy
μ-Slides VI (ibidi; Thistle Scientific) were coated overnight with 50 μL of 3 μg/mL ICAM-1Fc, then blocked with 2% BSA. Fluorescence-activated cell sorting (FACS)–sorted B lymphocytes (1 × 106/mL in Hanks balanced salt solution/20mM N-2-hydroxyethylpiperazine-N′-2-ethanesulfonic acid buffer) were allowed to settle for 10 minutes at 37°C. Images were taken at 15-second intervals with a Diaphot 300 microscope (Nikon Instruments Inc), using a 20× lens and AQM2001 Kinetic Acquisition Manager software (Kinetic Imaging, Andor Technology PLC). Cells were tracked using Motion Analysis software (Kinetic Imaging, Andor Technology PLC) and the data analyzed using a Mathematica notebook (Wolfram Research Inc) developed by Daniel Zicha (Cancer Research UK).
Live cell imaging of GFP-kindlin-3.
FACS-sorted B cells at 1 × 106 cells/mL were added to ICAM-1Fc–coated μ-Slides VI dishes as described above (see “Video microscopy”). Images were taken using a Axiovert 100M inverted confocal microscope (Carl Zeiss Microimaging Gmbh) with a 63× NA1.4 Plan-Apochromat oil immersion objective lens.
Interference reflection microscopy
Lymphoblasts were plated on μ-Slides VI coated with ICAM-1 (see “Video microscopy”). Images of close substrate contact of the GFP-positive migrating cells were acquired between 10 and 30 minutes of ICAM-1 attachment at 37°C in Hanks balanced salt solution/N-2-hydroxyethylpiperazine-N′-2-ethanesulfonic acid using a Zeiss Axiovert 100M inverted confocal microscope with a 63× NA1.4 Plan-Apochromat oil immersion objective lens. For evaluation of adhesion status, the area of contact was measured using MetaMorph Offline 7.1 (Molecular Devices, Dannaher Medical Technologies).
Statistical analysis
The adhesion and migration assays are presented as the mean (± SEM). The unpaired Student t test was performed on the interference reflection microscopy (IRM) data using GraphPad Prism software Version 4 for Macintosh computers. The quantitative reverse-transcription–PCR data were analyzed using the 2-way analysis of variance test, and the migration data were analyzed using a one-way analysis of variance test. The following significant differences are as indicated (*P < .05; **P < .01; and ***P < .001).
Results
Characterization of a new LAD-III patient of African-American origin
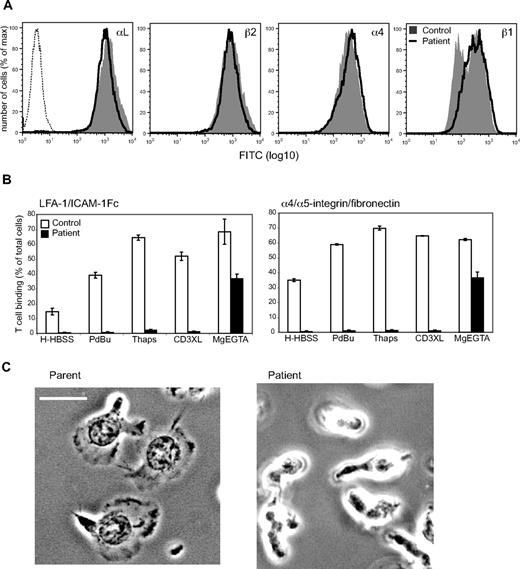
The patient is an 11-month-old African-American female with a severe bleeding tendency from birth and an elevated white blood cell count with persistent Gram-positive and -negative bacterial infections requiring hospitalization. These symptoms resembled a combination of Glanzmann thrombasthenia, in which platelets fail to aggregate because of mutations in the β3 integrin αIIbβ3, and LAD-I, in which mutation in the β2 subunit causes lack of expression of β2 integrins leading to impaired leukocyte extravasation.33 This combination of disease characteristics is typical of LAD-III. However, a key feature distinguishing LAD-III from Glanzmann thrombasthenia and LAD-I is the normal expression, but lack of function, of β1, β2, and β3 subclasses of integrins on cells of hematopoietic origin.34
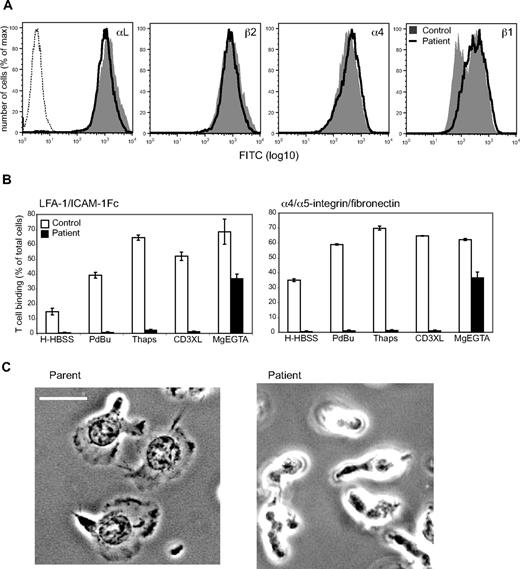
We therefore investigated LFA-1 (αL and β2 subunits) and α4β1 (α4 and β1 subunits) that are major integrins on T cells and found comparable expression between the patient, control (Figure 1A), and mother's T cells (data not shown). Analysis of integrin subclasses on the patient's neutrophils and EBV-transformed B cells also revealed normal levels of expression (data not shown). However, in contrast to control T cells, the patient's T cells failed to firmly adhere to LFA-1 ligand ICAM-1 and α4β1/α5β1 ligand fibronectin when adhesion was stimulated by inside-out signaling agonists (phorbol ester [PdBu]; Ca2+ mobilizer thapsigargin; or mAb cross-linking of the T cell receptor/CD3 complex; Figure 1B). Stimulation of adhesion with Mg2+/EGTA (ethyleneglycoltetraacetic acid), which activates integrins from “outside” the cell, showed that the integrins expressed by the patient's T cells were capable of adhesion. These findings were reinforced by the observation that the mother's T cells adhered and spread on ICAM-1 in a typical LFA-1–dependent manner, in contrast to the patient's T cells that were unable to spread (Figure 1C). Therefore the patient's T cells exhibit typical characteristics of the LAD-III disorder.
Characterization of a new LAD-III patient. (A) Expression levels of β2 integrin αLβ2 (LFA-1) and β1 integrin α4β1 are equivalent between LAD-III patient and control T lymphoblasts (control cells: gray fill; patient cells: dark line; representative mAb control: dashed line; n = 2). (B) Adhesion to LFA-1 ligand ICAM-1 and α4β1/α5β1 ligand fibronectin after inside-out signaling mediated by phorbol ester (PdBu), Ca2+ mobilizer thapsigargin (Thaps), or CD3 mAb cross-linking of the T-cell receptor/CD3 complex (CD3XL) and “outside-in” signaling via Mg2+/EGTA treatment (samples in triplicate; n = 2). (C) Attachment of T lymphoblasts to ICAM-1. The parent T cells spread as expected, whereas the patient T cells were lightly attached and failed to spread. Images are representative of 25 cells/experiment; n = 3. Scale bar represents 10 μm.
Characterization of a new LAD-III patient. (A) Expression levels of β2 integrin αLβ2 (LFA-1) and β1 integrin α4β1 are equivalent between LAD-III patient and control T lymphoblasts (control cells: gray fill; patient cells: dark line; representative mAb control: dashed line; n = 2). (B) Adhesion to LFA-1 ligand ICAM-1 and α4β1/α5β1 ligand fibronectin after inside-out signaling mediated by phorbol ester (PdBu), Ca2+ mobilizer thapsigargin (Thaps), or CD3 mAb cross-linking of the T-cell receptor/CD3 complex (CD3XL) and “outside-in” signaling via Mg2+/EGTA treatment (samples in triplicate; n = 2). (C) Attachment of T lymphoblasts to ICAM-1. The parent T cells spread as expected, whereas the patient T cells were lightly attached and failed to spread. Images are representative of 25 cells/experiment; n = 3. Scale bar represents 10 μm.
Assessment of mutations in the KINDLIN3 gene
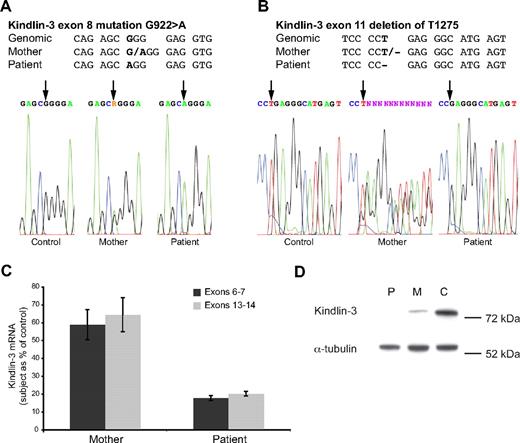
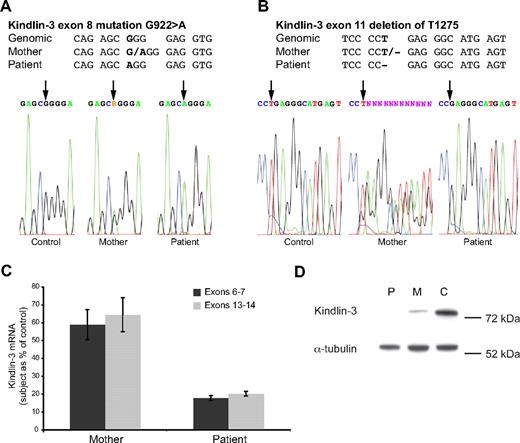
Sequencing of the KINDLIN3 genomic DNA revealed that the patient had 2 homozygous base changes at positions where the mother displayed heterozygosity, and these changes did not correspond to known polymorphisms in the KINDLIN3 gene. Furthermore, sequencing of all 15 exons and the intron/exon boundaries of the KINDLIN3 gene of the patient and her mother yielded no further unexpected mutations (data not shown but available on request).
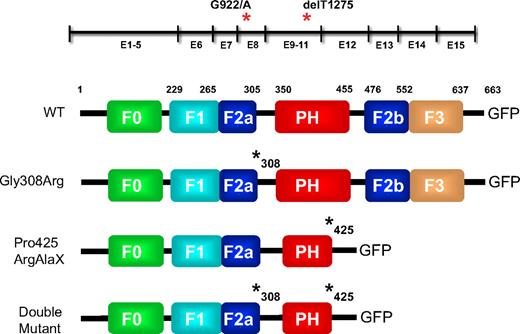
The first mutation was a G>A base substitution at position 922 in exon 8 predicted to cause an amino acid alteration of Gly308Arg (Figure 2A). The Gly308Arg change is located in the loop linking the first half of FERM subdomain 2 and the PH domain (Figure 4). The second mutation consisted of a single nucleotide deletion of 1275T (ΔT) in exon 11, causing a shift in the triplet reading frame and generating an in-frame TGA termination codon after a further 7 nucleotides (Figure 2B). Thus, premature termination will follow Pro425 after addition of 2 novel amino acids (Pro425GluGly>ProArgAlaX). This mutation is within the PH domain in the loop between the β6 and β7 strands and the first to be described in this kindlin-3 domain (supplemental Figure 1, available on the Blood Web site; see the Supplemental Materials link at the top of the online article).
Mutations in the human KINDLIN3 gene and the effect on mRNA and protein levels. (A-B) Alignment of the DNA sequence surrounding the 2 base changes (bold) in exons 8 and 11 of the KINDLIN3 gene of the LAD-III patient, her mother, and control. The original sequencing data are shown below. Reference genomic data from University of California Santa Cruz (chr11:64 250 959-64 269 504). (C) Taqman analysis of KINDLIN3 mRNA levels of mother and patient leukocytes compared with control leukocytes. Each mRNA sample was tested in quadruplicate and prepared twice or more with similar results. (D) Expression of kindlin-3 protein was absent in the patient (P), but present in mother (M) and control (C) T lymphoblasts as assessed by Western blotting (each sample tested twice; n = 2).
Mutations in the human KINDLIN3 gene and the effect on mRNA and protein levels. (A-B) Alignment of the DNA sequence surrounding the 2 base changes (bold) in exons 8 and 11 of the KINDLIN3 gene of the LAD-III patient, her mother, and control. The original sequencing data are shown below. Reference genomic data from University of California Santa Cruz (chr11:64 250 959-64 269 504). (C) Taqman analysis of KINDLIN3 mRNA levels of mother and patient leukocytes compared with control leukocytes. Each mRNA sample was tested in quadruplicate and prepared twice or more with similar results. (D) Expression of kindlin-3 protein was absent in the patient (P), but present in mother (M) and control (C) T lymphoblasts as assessed by Western blotting (each sample tested twice; n = 2).
Quantitative reverse-transcription–PCR was used to investigate the effect of these base changes on expression of patient KINDLIN3 mRNA isolated from T lymphoblasts. We used TaqMan probes specific for exons 6 to 7 that precede, and for exons 13 to 14 that follow, the mutation sites. For both sets of probes, the patient's T cells expressed a much reduced level of mRNA compared with control cells. The mother's T cells expressed approximately half the level of mRNA compared with the control cells, consistent with the lack of a functional KINDLIN3 gene on one allele (Figure 2C). The effect of the mutations was to cause unstable KINDLIN3 mRNA, leading to its destruction presumably by nonsense-mediated decay (NMD).
We then investigated the levels of T-lymphoblast kindlin-3 protein by Western blot analysis. No kindlin-3 protein was detected in the patient's T cells, whereas it was detected in the mother's T cells, but at a reduced amount compared with control T cells (Figure 2D). Therefore, as expected, the lack of KINDLIN3 mRNA meant that no kindlin-3 protein was made.
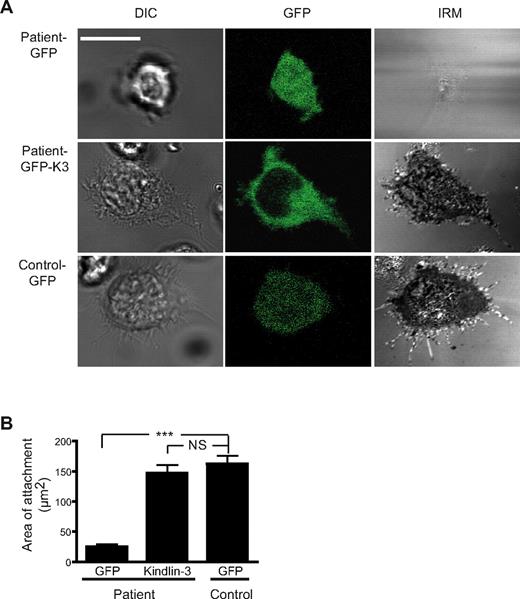
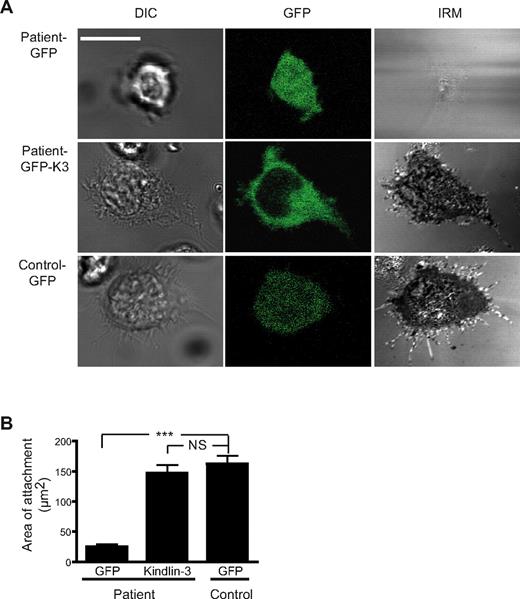
The effect of transfection of WT KINDLIN3 cDNA on LAD-III T-lymphocyte adhesion
As we were investigating a LAD-III patient from a new ethnic background, it was necessary to prove that the inability of lymphocytes to adhere was due to a faulty KINDLIN3 gene. We therefore transfected the patient's T lymphoblasts with mouse WT GFP-kindlin3 cDNA as previously described27 and used interference reflection microscopy (IRM) to assess the level of close contact of the cells with ICAM-1 as a measure of the extent of adhesion (Figure 3A). The GFP-transfected LAD-III T cells made poor contacts compared with the GFP-transfected control T cells (Figure 3A top panel versus bottom panel). However expression of WT GFP-kindlin3–cDNA in the LAD-III T cells increased contact with ICAM-1 (Figure 3A middle panel). Both individual IRM images and their quantification indicated that the GFP-kindlin3–transfected cells of the LAD-III patient made adhesions equivalent to the control T cells (Figure 3B). Therefore the failure of the patient's T cells to adhere to ICAM-1 could be restored by transfection with WT GFP-kindlin3 cDNA, proving that mutations in this protein were the cause of the LAD-III–like adhesion defects.
Adhesion characteristics of LAD-III T lymphocytes expressing WT kindlin-3. (A) Differential interference contrast (DIC), GFP, and IRM images of the patient T lymphoblasts transfected with GFP (top panel) and mouse GFP-kindlin3 cDNAs (middle panel) compared with the GFP-transfected control T lymphoblasts (bottom panel). Images are representative of 11-15 cells; n = 3. (B) Quantification of the area of close contact of the same cells; n = 11 cells per group.
Adhesion characteristics of LAD-III T lymphocytes expressing WT kindlin-3. (A) Differential interference contrast (DIC), GFP, and IRM images of the patient T lymphoblasts transfected with GFP (top panel) and mouse GFP-kindlin3 cDNAs (middle panel) compared with the GFP-transfected control T lymphoblasts (bottom panel). Images are representative of 11-15 cells; n = 3. (B) Quantification of the area of close contact of the same cells; n = 11 cells per group.
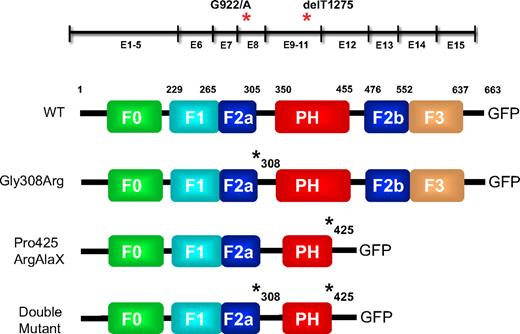
The ability of WT and mutated kindlin-3 protein to associate with membrane adhesions
As the 2 new LAD-III mutations were in domains of the kindlin-3 protein about which there is little information, it was of interest to determine whether they would affect the function of this protein in vitro. As well as human WT KINDLIN3, 3 separate mutant KINDLIN3 cDNAs were generated in a GFP vector (Figure 4). One mutant construct contained the G>A base change located at the end of the first half of FERM subdomain 2, giving rise to kindlin-3 protein expressing Gly308Arg. The second construct contained the deletion of T1275 in the PH domain and was designed to give rise to a protein truncated following Pro425ArgAlaX. The third construct incorporated both of the mutations (double mutant).
Diagrammatic representation of human KINDLIN3 gene and protein structure with the FERM subdomains (residues 1-663). The exons coding for the different subdomains are shown as well as the positions of the 2 LAD-III mutations, one in exon 8 and the other in exon 11 (illustrated with red asterisks). Details of the human kindlin-3-GFP chimeric proteins are illustrated. The WT protein contains a hypothetical F0 domain, the F1 domain, the F2 domain intersected by a PH domain, and the F3 domain that binds to the β subunit of integrin. The 3 additional schematics represent the individual kindlin-3 mutant proteins (Gly308Arg, Pro425ArgAlaX) and a protein incorporating both mutations (double mutant) resembling the patient's LAD-III protein.
Diagrammatic representation of human KINDLIN3 gene and protein structure with the FERM subdomains (residues 1-663). The exons coding for the different subdomains are shown as well as the positions of the 2 LAD-III mutations, one in exon 8 and the other in exon 11 (illustrated with red asterisks). Details of the human kindlin-3-GFP chimeric proteins are illustrated. The WT protein contains a hypothetical F0 domain, the F1 domain, the F2 domain intersected by a PH domain, and the F3 domain that binds to the β subunit of integrin. The 3 additional schematics represent the individual kindlin-3 mutant proteins (Gly308Arg, Pro425ArgAlaX) and a protein incorporating both mutations (double mutant) resembling the patient's LAD-III protein.
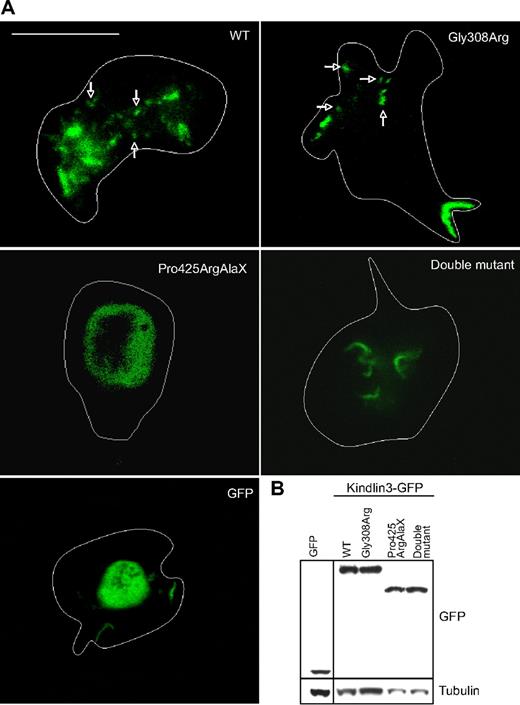
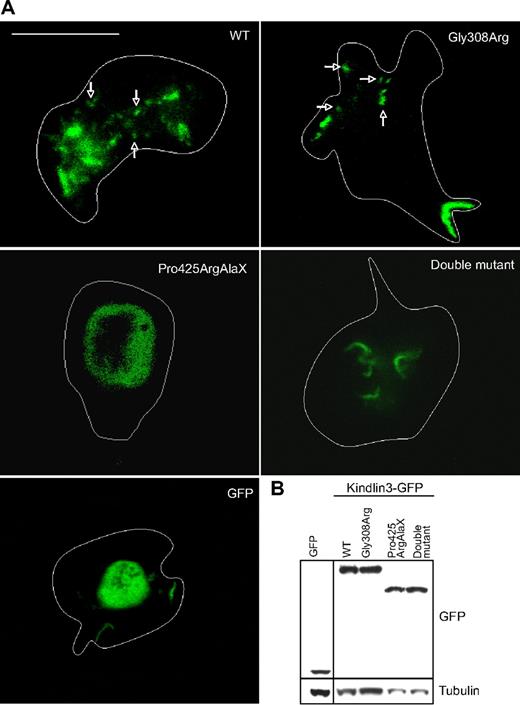
To gain some insight into whether kindlin-3 had a role at the level of the lymphocyte membrane, we transfected patient EBV-transformed B cells with WT KINDLIN3-GFP cDNA, the 3 mutant KINDLIN3-GFP cDNAs, and GFP cDNA as a control (Figure 5). The cells were FACS-sorted using GFP to be certain that similar levels of kindlin-3-GFP protein were expressed in each transfectant (data not shown). Western blotting confirmed the expression of GFP, kindlin-3-GFP WT, and mutant proteins and that the proteins were of expected molecular size (Figure 5B).
Confocal microscopy of LAD-III B cells transfected with human KINDLIN3-GFP cDNA constructs. (A) FACS-sorted LAD-III B cells transfected with GFP cDNA were compared with cells transfected with WT KINDLIN3, Gly308Arg, Pro425ArgAlaX, and double mutant KINDLIN3-GFP cDNAs. Fluorescent images of live B cells taken at the interface with ICAM-1 show punctate membrane localization (arrows) of WT and Gly308Arg Kindlin-3-GFP protein compared with other transfectants showing a diffuse distribution of fluorescence in the cell body and extensions. The boundaries of the cells are highlighted with a white line. Only the WT and Gly308Arg KINDLIN3-GFP cDNA–transfected cells adhered well. The cells are typical examples from 1 experiment of n = 4. Scale bar represents 10 μm. (B) Western blot of GFP, WT kindlin-3-GFP, full-length Gly308Arg, and truncated Pro425ArgAlaX and double mutant kindlin-3-GFP proteins expressed in EBV-transformed B cells and showing the expected molecular size. Loading control is α-tubulin.
Confocal microscopy of LAD-III B cells transfected with human KINDLIN3-GFP cDNA constructs. (A) FACS-sorted LAD-III B cells transfected with GFP cDNA were compared with cells transfected with WT KINDLIN3, Gly308Arg, Pro425ArgAlaX, and double mutant KINDLIN3-GFP cDNAs. Fluorescent images of live B cells taken at the interface with ICAM-1 show punctate membrane localization (arrows) of WT and Gly308Arg Kindlin-3-GFP protein compared with other transfectants showing a diffuse distribution of fluorescence in the cell body and extensions. The boundaries of the cells are highlighted with a white line. Only the WT and Gly308Arg KINDLIN3-GFP cDNA–transfected cells adhered well. The cells are typical examples from 1 experiment of n = 4. Scale bar represents 10 μm. (B) Western blot of GFP, WT kindlin-3-GFP, full-length Gly308Arg, and truncated Pro425ArgAlaX and double mutant kindlin-3-GFP proteins expressed in EBV-transformed B cells and showing the expected molecular size. Loading control is α-tubulin.
We then viewed the cells by confocal microscopy after 20-minute migration on immobilized ICAM-1. Punctate staining was visible at the interface with ICAM-1 for B cells expressing WT and Gly308Arg mutant kindlin-3, but not for the cells expressing either Pro425ArgAlaX, the double mutant, or GFP proteins (Figure 5A). Therefore, WT kindlin-3-GFP was expressed at membrane level and this localization was not affected by the Gly308Arg mutation, but was prevented by the Pro425ArgAlaX mutant that was truncated in the PH domain.
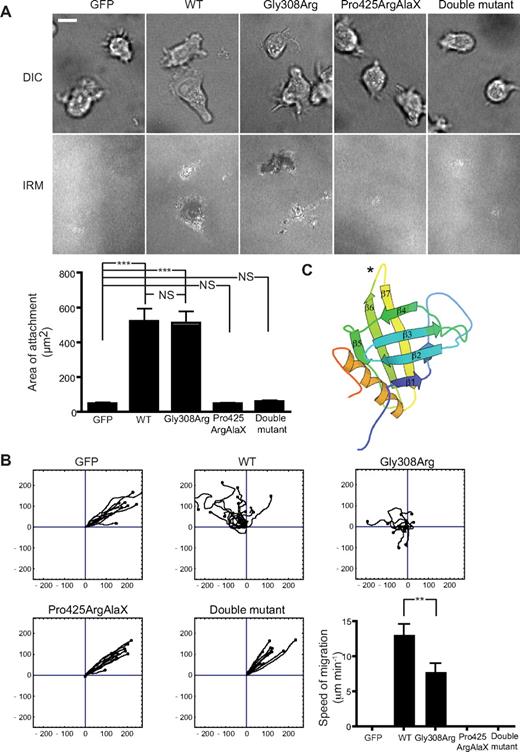
Adhesion and migration of LAD-III B lymphocytes after transfection of WT and mutated KINDLIN3 cDNA
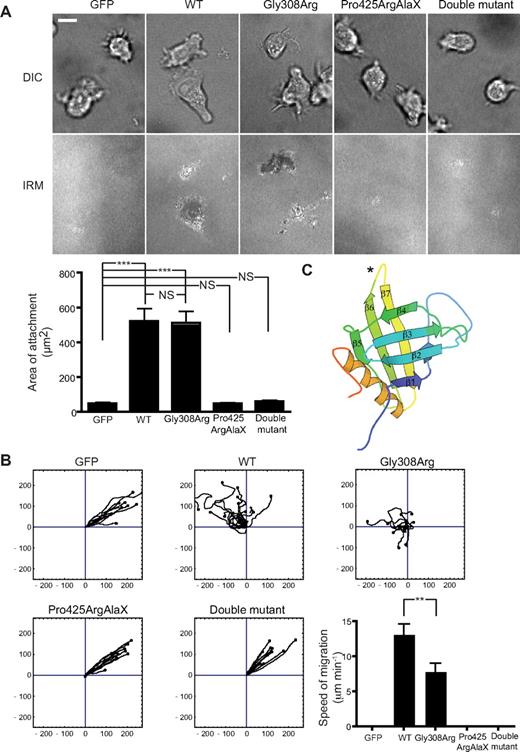
We next wanted to test whether the presence of membrane-localized kindlin-3 correlated with the ability of B cells to adhere and migrate. We have shown previously that normal B cells, but not LAD-III B cells, could undergo LFA-1–mediated adhesion and migration on ICAM-1.27 The patient B cells transfected with GFP failed to adhere as measured by IRM (Figure 6A). This was also reflected in their inability to migrate, resulting in a floating cell phenotype (Figure 6B; supplemental Video 1). Transfection of LAD-III B cells with WT KINDLIN3 cDNA restored the ability to adhere both at a single-cell level and when the area of attachment was quantified (Figure 6A). Random migration on ICAM-1 could also be restored by transfection of the cells with WT KINDLIN3 cDNA (Figure 6B; supplemental Video 2).
Adhesion and migration characteristics of LAD-III B cells expressing human WT and mutant kindlin-3-GFP. (A) DIC and IRM images of the LAD-III patient's EBV-transformed B cells transfected with GFP cDNA were compared with cells transfected with WT KINDLIN3, Gly308Arg, Pro425ArgAlaX, and double mutant KINDLIN3 cDNAs. Images are representative of 20 fields per sample; n = 3. Quantification of the area of close contact from one typical experiment; n = 30 cells/group. Data are shown as mean ± SEM; ***P < .001; NS indicates not significant. Scale bar represents 10 μm. (B) Migration characteristics of LAD-III B cells transfected with GFP cDNA were compared with cells transfected with WT KINDLIN3-GFP, Gly308Arg, Pro425ArgAlaX, and double mutant KINDLIN3-GFP cDNAs. n = 3 for each cDNA construct. Single-cell tracking images are accompanied by quantification of average speed of migration for n = 15 cells/group from a representative experiment. Data are shown as mean ± SEM; **P < .01. (C) Model of the kindlin-3 PH domain showing location of the Pro425AlaArgX truncation mutation (*) in the loop between the β6 and β7 strands.
Adhesion and migration characteristics of LAD-III B cells expressing human WT and mutant kindlin-3-GFP. (A) DIC and IRM images of the LAD-III patient's EBV-transformed B cells transfected with GFP cDNA were compared with cells transfected with WT KINDLIN3, Gly308Arg, Pro425ArgAlaX, and double mutant KINDLIN3 cDNAs. Images are representative of 20 fields per sample; n = 3. Quantification of the area of close contact from one typical experiment; n = 30 cells/group. Data are shown as mean ± SEM; ***P < .001; NS indicates not significant. Scale bar represents 10 μm. (B) Migration characteristics of LAD-III B cells transfected with GFP cDNA were compared with cells transfected with WT KINDLIN3-GFP, Gly308Arg, Pro425ArgAlaX, and double mutant KINDLIN3-GFP cDNAs. n = 3 for each cDNA construct. Single-cell tracking images are accompanied by quantification of average speed of migration for n = 15 cells/group from a representative experiment. Data are shown as mean ± SEM; **P < .01. (C) Model of the kindlin-3 PH domain showing location of the Pro425AlaArgX truncation mutation (*) in the loop between the β6 and β7 strands.
In terms of the LAD-III B cells transfected with the mutated constructs, Gly308Arg KINDLIN3 restored cell adhesion comparably with WT KINDLIN3 (Figure 6A). However, this same transfectant had significantly reduced levels of migration compared with WT KINDLIN3-transfected LAD-III B cells (Figure 6B; supplemental Video 3). This mutant also had the effect of interfering with migration when transfected into normal EBV-transformed B cells (data not shown). Therefore, although not affecting the ability of kindlin-3–expressing cells to adhere, the presence of the Gly308Arg change in FERM subdomain 2 affects another kindlin-3 function upon which migration is dependent.
Finally, transfection with the truncated Pro425ArgAlaX KINDLIN3 cDNA that terminates within the PH domain and KINDLIN3 containing both mutations (double mutant) failed to restore either adhesion (Figure 6A) or migration (Figure 6B; supplemental Videos 4-5) of LAD-III B cells. A model of the kindlin-3 PH domain is shown with the location of Pro425ArgAlaX in the β6 to β7 loop indicated (Figure 6C). We compared the FERMT3/kindlin-3 PH domain with PH domains expressing both canonical and noncanonical phosphatidylinositol (PI)–binding sites (supplemental Figure 1).19,20 The kindlin-3 PH domain displays all the key conserved residues of the canonical binding site, indicating that it will bind phosphoinositides. A dendrogram of relatedness to other canonical PH domain–containing proteins shows it to most closely resemble Bruton tyrosine kinase, phosphoinositide-dependent protein kinase 1, and phospholipase Cδ1, key immune cell mediators (supplemental Figure 2). Thus, an explanation for the lack of association of Pro425ArgAlaX kindlin-3 with the membrane is that the truncated PH domain is no longer capable of membrane anchoring.
Discussion
We describe here a new LAD-III patient of African-American origin who, unlike previously described LAD-III patients, expresses 2 homozygous mutations in the KINDLIN3 gene. The mutated KINDLIN3 DNA in the patient's primary leukocytes results in destabilized mRNA, so that no kindlin-3 protein is detectable and this causes the LAD-III phenotype.
An issue of interest is the inheritance of the 2 homozygous KINDLIN3 mutations. One option is that they have coevolved and a second is that they have arisen separately and become linked in the African-American population, to which our patient and her heterozygous mother belong. Population screening would be required to investigate the frequency of the 2 KINDLIN3 mutations within this group. The LAD-III disease characteristics of the patient are particularly severe.31 For example, the patient displayed extensive osteopetrosis that has also been a feature of the Kindlin3−/− mice.15 This has so far been detailed for one other LAD-III patient with a mutation in the kindlin-3 F0 subdomain.29 Differences in disease severity between LAD-III patients may depend on their genetic backgrounds. However, it is also possible that the nature of the KINDLIN3 mutation may play a role, potentially giving rise to small amounts of mutated protein in vivo that are difficult to detect in vitro. As the 2 mutations of the African-American patient affect both adhesion-dependent as well as adhesion-independent functions in in vitro assays, they might be particularly debilitating in terms of disease. Therefore, there may be heterogeneity in the LAD-III disorder that is dependent on the location of the KINDLIN3 mutations.
The lack of patient KINDLIN3 mRNA indicates that the mutations caused instability and subsequent loss through NMD. However we reasoned that KINDLIN3 cDNA constructs containing the individual mutations would be resistant to NMD because of their lack of introns35,36 and give rise to KINDLIN3 mRNA and protein. Therefore to further examine the properties of this protein in vitro, we made WT KINDLIN3-GFP and the 2 mutant cDNAs separately. As expected, all constructs gave rise to protein when transfected into lymphocytes. It is well-established that FERM subdomain 3 of the kindlins binds to the integrin β subunit and that this binding enables the talin FERM domain to function as an integrin activator.14-16 B cells expressing WT kindlin-3-GFP displayed punctate kindlin-3 localization at the interface of the cell membrane with LFA-1 ligand ICAM-1. This is in keeping with the ability of kindlin-3 to bind to the β2 subunit of integrins.16 Both kindlin-1 and kindlin-2 colocalize with focal adhesions in nonhematopoietic cells,12,37 suggesting a conservation in function between all 3 members of the kindlin family in this regard.
However, little is known of other kindlin-3 activities, so it was of interest to investigate the 2 LAD-III patient mutations separately, in circumstances where they would be expressed, to discover whether their effects on function were similar or distinctive. A function of PH domains is to act as a membrane anchor via recognition of PI-binding sites.17,18 The canonical PI recognition site is composed of the loop between β1 and β2 strands of the fold with secondary involvement of β3-β4 and β5-β6 loops.20 A second noncanonical PI binding site is located on the opposing side of the β1/β2 strands, with additional input from the β5-β6 loop.19 Bioinformatics analysis shows that the kindlin-3 PH domain expresses a canonical PI-binding motif, suggesting a role for the kindlin-3 PH domain in membrane anchoring. Of interest is the relatedness of the kindlin-3 PH domain to the PH domains of other immune mediators Bruton tyrosine kinase, 3′-phosphoinositide–dependent kinase, and phospholipase Cδ1 that serve as membrane-anchoring domains for these proteins.
The kindlin-3 proteins expressing the PH domain with the Pro425ArgAlaX mutation are truncated following the β6 strand. The deleted sequence includes the β7 strand that is a major support of 1 β sheet of the fold. Its absence is predicted to destroy the overall topology of the entire 7-stranded β sheet fold, thereby inactivating PH domain function. The instability of this truncated PH domain offers an explanation as to why the Pro425ArgAlaX and double mutant kindlin-3–expressing cells are unable to make membrane attachments. The lack of an intact PH domain would also contribute to the inability of the 2 kindlin-3 proteins with mutant PH domains to restore either adhesion or migration of the LAD-III B cells.
It seemed possible that the Gly308Arg point mutation was a population-associated polymorphism, coinherited with the debilitating Pro425ArgAlaX mutation. Consistent with this idea, Gly308Arg kindlin-3–expressing LAD-III B cells made punctate attachments similar to WT kindlin-3–expressing B cells and restored the ability of the cells to adhere to ICAM-1 comparably with WT kindlin-3. It was therefore unexpected to find that expression of this mutant kindlin-3 did not fully restore migration of LAD-III cells and, secondly, that it interfered with migration of normal B cells. This suggested that integrin-mediated adhesion is not the only function that kindlin-3 participates in and that the Gly308Arg base change affected, not adhesion, but another activity of kindlin-3 essential for migration. Support for a second category of kindlin-3 function involving migration comes from studies using mouse Kindlin3−/− platelets. In response to Mn2+ that induces the αIIbβ3 integrin to bind ligand, platelets are able to attach, but are unable to spread like Kindlin3−/− platelets.15
Other than integrin binding, the contributions that the individual kindlin FERM subdomains might make to adhesion or migration have not been clearly defined. The kindlins are regarded essentially as scaffold proteins lacking domains with intrinsic activity. To date, integrin-linked kinase has been identified as a binding partner of UNC112, the kindlin homologue in Caenorhabditis elegans38 and kindlin-2 in fibroblasts.39 The filamin-binding protein, migfilin, also binds to kindlin-2.40 Both could potentially provide a link to the actin cytoskeleton, but so far there is no information as to how these proteins interact with the kindlin structure.13,41 Kindlin-1 lacking the FERM F0 domain has decreased ability to activate integrin in CHO cells, showing the importance of other regions in terms of function.42 Further explanation awaits detailed structural studies on the kindlins and more information about their binding partners, especially in leukocytes.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
We thank Dr Ian Tomlinson (Wellcome Trust Center for Human Genetics), Dr Saverio Brogna, University of Birmingham, and Dr Paul Bates (Cancer Research UK London Research Institute [CR- UK LRI]) for their most helpful advice on genetics, NMD, and protein structure, respectively; Drs Markus Moser, Siegfried Ussar, and Reinhard Faessler (Max Planck Institute of Biochemistry) for the anti–human kindlin-3 antibody and mouse GFP-Kindlin3 construct; and Darren Harvey (CR-UK LRI) for generation of the LAD-III EBV-transformed cell lines. We are most grateful to Mike Fried (University of California, San Francisco) and Erik Sahai (CR-UK LRI) for careful reading of this paper.
L.S. was supported by a Marie Curie individual fellowship.
Authorship
Contribution: A.M. and L.S. performed experiments, interpreted results, and assisted with writing the paper; P.S., I.P., and K.H. performed experiments and commented on the paper; P.C. contributed the bioinformatics information; H.S. and M.B. supplied patient material; and N.H. directed the project and wrote the paper.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: N. Hogg, Leukocyte Adhesion Laboratory, Cancer Research UK London Research Institute, 44 Lincoln's Inn Fields, London WC2A 3PX, United Kingdom; e-mail: nancy.hogg@cancer.org.uk.
References
Author notes
A.M. and L.S. contributed equally to this work.