Abstract
Sickle cell disease is characterized by painful vaso-occlusive crises during which abnormal interactions between erythroid adhesion molecules and vessel-wall proteins are thought to play a critical role. Hydroxyurea, the only drug with proven benefit in sickle cell disease, diminishes these interactions, but its mechanism of action is not fully understood. We report that, under hydroxyurea, expression of the unique erythroid laminin receptor Lu/BCAM was increased, but red blood cell adhesion to laminin decreased. Because Lu/BCAM phosphorylation is known to activate cell adhesion to laminin, it was evaluated and found to be dramatically lower in hydroxyurea-treated patients. Analysis of the protein kinase A pathway showed decreased intracellular levels of the upstream effector cyclic adenosine monophosphate during hydroxyurea treatment. Using a cellular model expressing recombinant Lu/BCAM, we showed that hydroxyurea led to decreased intracellular cyclic adenosine monophosphate levels and diminished Lu/BCAM phosphorylation and cell adhesion. We provide evidence that hydroxyurea could reduce abnormal sickle red blood cell adhesion to the vascular wall by regulating the activation state of adhesion molecules independently of their expression level.
Introduction
Sickle cell disease (SCD) is characterized by painful episodic vaso-occlusive crises (VOCs), acute chest syndrome, and a chronic inflammatory state. Hydroxyurea (HU), also called hydroxycarbamide, is the only drug now available having demonstrated benefit for SCD patients, with fewer VOCs and acute chest syndromes and lower mortality and morbidity.1-4 It was commonly thought that HU acted as an antisickling agent by increasing fetal hemoglobin (HbF) levels, leading to significantly less hemoglobin S polymerization. However, HU was often associated with clinical improvement before HbF rose significantly, suggesting that it could also act through other mechanisms.2
Growing evidence supports the hypothesis that, in SCD patients, transit of red blood cells (RBCs) into small vessels could be slowed by their abnormal adhesion to the vascular wall through interactions between erythroid adhesion molecules and proteins on the surface of endothelial cells or extracellular matrix (ECM) components.5-7 Such interactions could play a critical role in HbS polymerization and VOC development by prolonging RBC transit time in capillaries.
Several interactions have been described between SS RBCs and the endothelial vascular wall. Integrin α4β1, expressed on young circulating reticulocytes, is one of the major factors in these interactions through its binding to vascular cell adhesion molecule-1, fibronectin, thrombospondin (TSP), and endothelial Lu/BCAM (Lutheran/basal cell-adhesion molecule).8-13 TSP mediates adhesion of SS reticulocytes to endothelial cells by bridging CD36 molecules expressed on both cell types.14 However, the clinical severity of SCD in CD36-deficient patients is not diminished.15 Landsteiner-Wiener/intercellular adhesion molecule-4 (LW/ICAM-4) and Lu/BCAM are members of the immunoglobulin superfamily, expressed on young and mature RBCs; they are also involved in the abnormal adhesion of SS RBCs through interactions with endothelial integrin αVβ3 and ECM laminin 511/521, respectively.16-21 In vivo, HU decreases the percentage of circulating CD36- and α4β1-expressing reticulocytes22 and CD36 and α4β1 expression levels at the mRNA and protein levels23 ; it also reduces phosphatidylserine expression on the surfaces of erythrocytes and platelets,24 and plasma levels of soluble vascular cell adhesion molecule-1 and endothelin-1.25,26 HU diminishes SS RBC adhesion to endothelial cells and the ECM proteins, fibronectin, TSP, and laminin.23,27,28 These decreases are consistent with less CD36, α4β1, and LW/ICAM-4 expression on the surfaces of SS reticulocytes and erythrocytes.29
Surprisingly, Odièvre et al showed that RBC expression of Lu/BCAM, the unique erythroid receptor for laminin,19,21 was significantly elevated in HU-treated children.29 Consequently, SS RBC adhesion to laminin could not be directly linked to the cell-surface Lu/BCAM expression level. Lu/BCAM is responsible for abnormal SS RBC adhesion to laminin in a protein kinase A (PKA)- and/or Rap1-dependent manner.30,31 Although Lu/BCAM is expressed on normal (AA) and SS RBCs, only SS RBCs adhere to laminin and resist high shear-stress forces.19,21,32 This adhesion is activated by the phosphorylation of serine 621 in the Lu/BCAM cytoplasmic domain on PKA-pathway activation.33 Lu/BCAM is not phosphorylated in AA RBCs.33
For this study, we hypothesized that HU could interfere with SS RBC adhesion to laminin by modulating Lu/BCAM phosphorylation. Adhesion to laminin of RBCs from adult SCD patients, HU-treated or not, was investigated during a quiescent phase of the disease (steady state). HU increased Lu/BCAM erythroid expression but decreased RBC adhesion to laminin; that diminished adhesion was correlated with less Lu/BCAM phosphorylation. Analysis of the signaling pathways involved in Lu/BCAM phosphorylation showed decreased intracellular levels of cyclic adenosine monophosphate (cAMP), the upstream effector of both PKA and Epac/Rap1 pathways, during HU treatment. These observations were then confirmed in a cellular model expressing recombinant Lu/BCAM long isoform Lu. Our results provide the first evidence that HU could reduce abnormal RBC adhesion to the vascular wall by acting on the activation state of adhesion molecules (eg, Lu/BCAM), independently of their expression level.
Methods
Patients and blood samples
Homozygous SCD patients (SS) at least 18 years old, able to give their informed consent and consulting at our Adult Sickle Cell Referral Center, were eligible for inclusion in this study, which was approved by the local ethics committee (Comité de Protection des Personnes) and was conducted in accordance with the provisions of the Declaration of Helsinki and local laws and regulations. Experiments were performed with freshly drawn ethylenediaminetetraacetic acid–anticoagulated venous blood from healthy adult donors or HU-treated or untreated adult SS patients. SCD steady state was defined as a visit at least more than or equal to 1 month after an acute clinical event and more than or equal to 3 months after blood transfusion. None of the included patients had an acute SCD-related event during the 2 weeks after sampling at steady state.
Cell lines and antibodies
Human erythroleukemic K562 cells expressing the long human Lu/BCAM isoform (Lu-gp), K562-Lu, were obtained and grown, in the absence or presence of 250μM HU (Sigma-Aldrich) for 24 and 48 hours,27 as described.19 Mouse antihuman Lu/BCAM monoclonal antibody (mAb), clone F241, was produced in our institute.33 Biotinylated goat polyclonal anti-Lu/BCAM antibody was from R&D Systems.
Flow cytometry
Percentages of reticulocytes in whole or fractionated blood samples were determined using thiazole orange dye (Retic-Count, BD Biosciences) and a BD FACScanto II flow cytometer (BD Biosciences) with FACSDiva software (Version 6.1.2) for acquisition and analysis. The percentage was determined by gating the red cell population based on size (forward scatter) and granularity (side scatter). Expression of cell-surface Lu/BCAM on RBCs and transfected K562-Lu cells was evaluated with anti-Lu/BCAM F241 mAb. Mean fluorescence intensity (MFI) was determined under the same conditions for all samples. Lu/BCAM antigen strength varies widely among persons and exhibits heterogeneity between individual RBCs within a given person. This variability accounts for the mixed field-agglutination patterns showing clumps of agglutinated cells in the presence of many free cells, usually seen with Lutheran antisera, especially anti-Lua, and the wide range of survival times of Lu(b+) cells introduced into a Lu(a+b−) person with anti-Lub.34 Therefore, Lu/BCAM-positive RBCs were gated, and Lu/BCAM MFI was calculated only for this population.
Percoll double-density separation
All collected blood samples designated for this fractionation were kept at 4°C overnight, then subjected to density separation at room temperature as described.35 Percoll (Sigma-Aldrich) was diluted in 125mM NaCl, 4.5mM KCl, 3% bovine serum albumin (BSA) to obtain densities of 1.076 and 1.085; 3 mL of the latter density was placed in an empty 15-mL polypropylene tube followed by 3 mL of the former, and then 3 mL of whole blood was carefully loaded onto the surface. After centrifugation (30 minutes, 1000g), blood fractions were collected and washed 3 times with Hanks buffer (Sigma-Aldrich). An aliquot was saved to count reticulocytes by flow cytometry, and the rest was used in adhesion and phosphorylation assays.
Adhesion assays
RBC and K562-Lu-cell adhesions to laminin were measured under physiologic flow conditions using a plate flow chamber, by a person blinded to the patient's status, as described.33 Laminin 511/521 (10 μg, Sigma-Aldrich) from human placenta was immobilized in uncoated μI microslides (ibidi; internal channel dimensions: length 50 mm, width 5 mm, height 0.4 mm) at 4°C overnight. RBCs and K562-Lu cells were washed and suspended, respectively, in Hanks buffer supplemented with 0.2% BSA at hematocrit 0.5% and 107 cells/mL. Cells were perfused through the microslide at a shear stress of 0.4 dyn/cm2 for 5 minutes at 37°C and washouts used Hanks buffer at 0.4 and 2 dyn/cm2 for 5 minutes each. After each wash, adherent cells were counted in 5 representative areas along the centerline of the microslide by microscopy using Optimas 6.1 image analysis system (Media Cybernetics).
Phosphorylation assays
RBCs and K562-Lu cells were phospholabeled as described.33 Briefly, RBCs (200 μL) were incubated in 1.8 mL of buffer A (150mM NaCl; 20mM Tris-HCl, pH 7.5; 10mM KCl; 1mM MgCl2) for 4 hours at 35°C, centrifuged at 750g for 3 minutes, and suspended in 1.8 mL of buffer A containing 32P (300 μCi) for 14 hours at 35°C. RBCs were washed twice with cold PBS and lysed with buffer A containing 1% Triton X-100, 0.2% BSA, phosphatase (Sigma-Aldrich), and protease inhibitor cocktails (Roche Diagnostics). Lu/BCAM was immunoprecipitated with F241 mAb and protein A-Sepharose CL4B beads (Roche Diagnostics) overnight at 4°C. After sodium dodecyl sulfate–polyacrylamide gel electrophoresis and protein transfer, phosphorylated proteins were detected and quantified (P) with a FujiFilm BAS-1800 II PhosphorImager, using Image Reader BAS-1800 II Version 1.8 and Multi Gauge, Version 3.0 software, respectively (Fuji). Total Lu/BCAM was then revealed on the same membrane by Western blotting (WB) using biotinylated anti-Lu/BCAM antibody (R&D Systems) and the Molecular Imager Gel Doc XR System (Bio-Rad). Proteins were quantified by WB using Quantity One software (Bio-Rad). The P/WB ratio was calculated to determine the proportion of phosphorylated Lu/BCAM among total immunoprecipitated Lu/BCAM proteins.
cAMP quantification
Total cAMP was measured in RBCs and K562-Lu cells as described in the Cayman Chemical cAMP enzyme immunoassay kit. Briefly, 70 μL of RBCs or 5 × 106 K562-Lu cells was lysed in 430 μL or 200 μL of 0.1M HCl, respectively. After centrifugation, supernatants were acetylated, and 50 μL of each was added per well in a 96-well ELISA plate provided in the kit. After an 18-hour incubation at 4°C, wells were washed and 200 μL of revelation buffer was added to each well. After 2 hours of incubation at room temperature, total cAMP levels were measured according to the manufacturer's instructions.
Statistical analyses
Results are expressed as medians (interquartile range), mean plus or minus SD, mean plus or minus SEM, numbers, or percentages, as appropriate. Nonparametric tests were used because normal distribution could not be assumed because of the small samples (< 30), and those data had skewed distributions. Thus, quantitative parameters were compared between groups using a Mann-Whitney test, Kruskal-Wallis test for more than 2 groups, Wilcoxon signed-rank test for paired observations, or Friedman test for repeated measures. Fisher exact test was used for variance comparisons. Correlations were sought with simple linear regression and Pearson correlation. A P value less than or equal to .05 was considered significant.
Results
Patients
The 49 homozygous SCD patients enrolled in this study formed 3 groups: 13 patients followed prospectively before and after starting HU (20 mg/kg per day) with 6 months of follow-up (pre-post group), 15 untreated patients (UT group), and 21 HU-treated patients (HU group). Results obtained with blood samples from the pre-post group before and more than 6 months after starting HU were also included in the UT and HU groups, thereby raising the respective numbers of blood samples to 28 and 34. The mean plus or minus SD age and the male/female ratio were 36 plus or minus 8.34 years and 0.75 for the UT group and 32 plus or minus 8.64 years and 0.41 for the HU group. RBCs from 7 healthy donors were also analyzed.
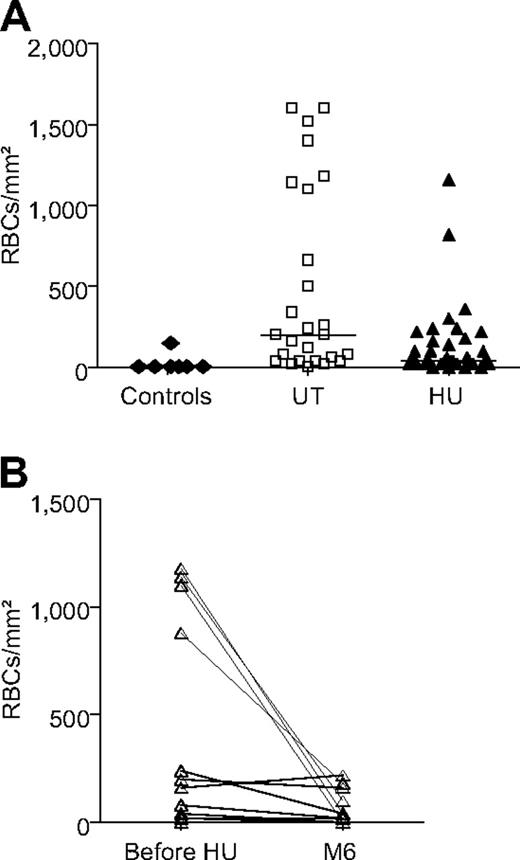
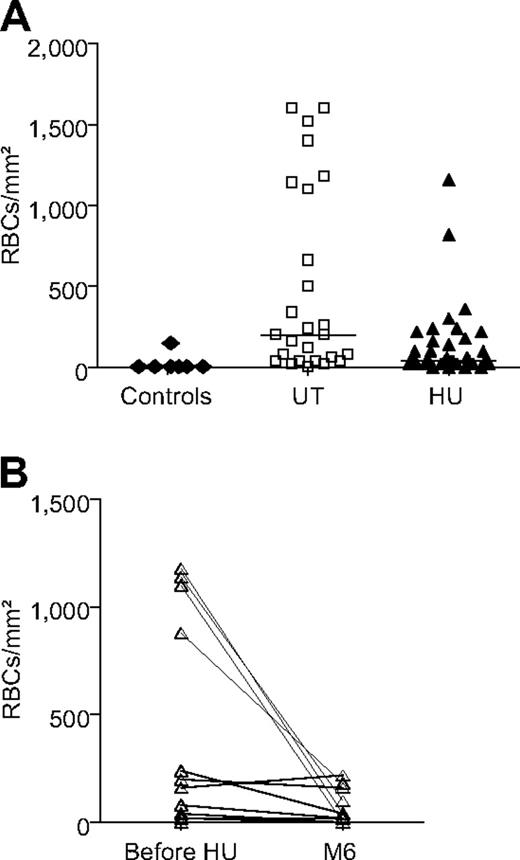
Less adhesion to laminin by SS RBCs from HU-treated patients
The effect of HU treatment on SS RBC adhesion to laminin was investigated with adhesion assays under flow conditions with 34 blood samples from HU-treated patients and 28 from UT patients. HU-exposed SS RBCs adhered less than UT SS RBCs with respective medians of 40 versus 200 RBCs/mm2 at 2 dyn/cm2 (P = .007; Figure 1A) and 160 versus 550 RBCs/mm2 at 0.4 dyn/cm2 (P = .008; data not shown). The impact of HU on cell adhesion was also analyzed by comparing the UT and HU groups in terms of RBC adhesion value distributions. We found that the dispersion of values was much wider for the UT group than the HU group, with significantly different between group variance values (Fisher exact test, P < .001). Adhesion of RBCs from 7 control donors was close to null and significantly lower than for the UT and HU groups (P < .01).
Fewer SS RBCs adhered to laminin during HU treatment. (A) Blood samples from 7 healthy controls, 28 untreated (UT), and 34 HU-treated patients (HU). Horizontal lines represent medians. UT RBCs were more adherent than HU RBCs (2 dyn/cm2, P = .007; Mann-Whitney test). Exposure to HU led to less dispersion of HU group values compared with the UT group (P < .001; Fisher exact test). (B) For the pre-post group, RBC adhesion was significantly lower after 6 months of HU (M6) than before (2 dyn/cm2, n = 13; P = .013; Wilcoxon signed-rank test).
Fewer SS RBCs adhered to laminin during HU treatment. (A) Blood samples from 7 healthy controls, 28 untreated (UT), and 34 HU-treated patients (HU). Horizontal lines represent medians. UT RBCs were more adherent than HU RBCs (2 dyn/cm2, P = .007; Mann-Whitney test). Exposure to HU led to less dispersion of HU group values compared with the UT group (P < .001; Fisher exact test). (B) For the pre-post group, RBC adhesion was significantly lower after 6 months of HU (M6) than before (2 dyn/cm2, n = 13; P = .013; Wilcoxon signed-rank test).
Because of wide interindividual variability in SCD, the same assays were run using blood samples from 13 pre-post group patients, which showed that adhesion was significantly lower after 6 months of HU (P = .013) and dramatically diminished for the 5 patients with the highest adhesion levels before starting HU (Figure 1B).
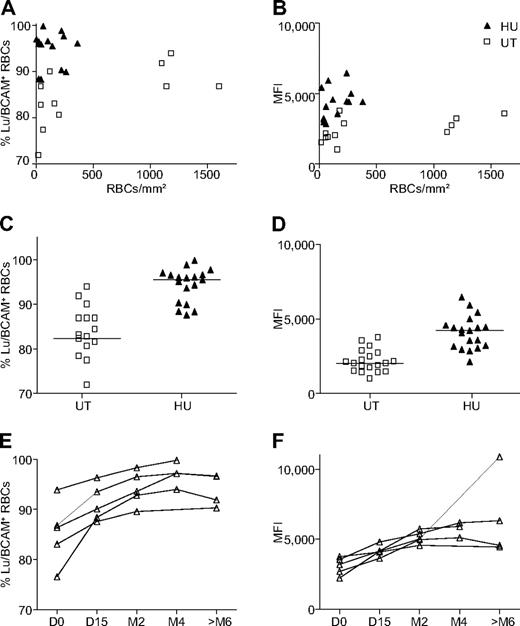
SS RBC adhesion to laminin is not correlated with the Lu/BCAM expression level
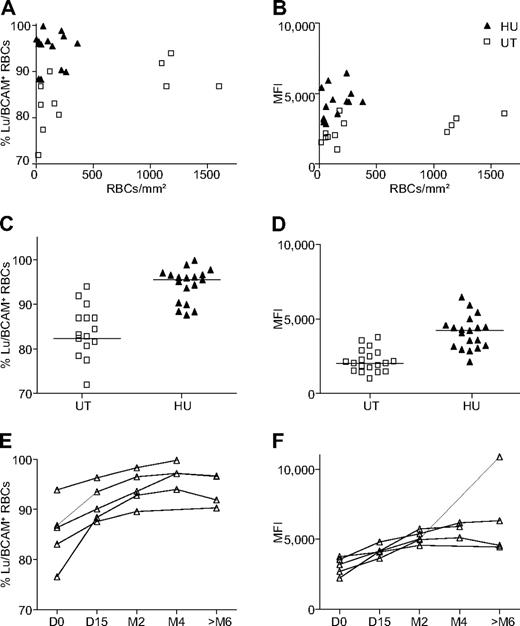
To determine whether SS RBC adhesion to laminin was conditioned by the Lu/BCAM expression level, flow cytometry and cell-adhesion assays were conducted with 14 and 12 HU- and UT group blood samples, respectively. When all patients were taken into account, no correlation was found between the adhesion level and Lu/BCAM expression, as determined by the percentage of RBCs expressing Lu/BCAM or the number of Lu/BCAM molecules/RBC, estimated by Lu/BCAM-positive RBC MFI (Figure 2A-B). When UT- and HU-treated patients were considered separately, no correlation was found between adhesion level and Lu/BCAM expression, although a trend emerged for the UT group associating the adhesion level and MFI of Lu/BCAM-positive RBCs (P = .06, r2 = 0.3, n = 12).
HU-exposed SS RBC adhesion to laminin decreased, whereas Lu/BCAM erythroid expression increased. Lu/BCAM expression was measured by flow cytometry using anti-Lu monoclonal antibody F241. (A-B) SS RBC adhesion as a function of the percentage of RBCs from 12 untreated (UT) and 14 HU-treated patients expressing Lu/BCAM (Lu/BCAM+; A) or of Lu/BCAM MFI (B). (C-D) Lu/BCAM expression level on the surface of RBCs from 19 UT and 19 HU-treated patients represented as the percentage of circulating RBCs expressing Lu/BCAM (C) and the latter's MFI (D). HU increased the percentage of Lu/BCAM-positive RBCs (P < .001) and Lu/BCAM MFI (P < .001; Mann-Whitney test). Horizontal lines represent medians. (E-F) Same as panels C and D for the 5 pre-post group patients before (D0) and during HU treatment (D15, M2, M4, and > M6).
HU-exposed SS RBC adhesion to laminin decreased, whereas Lu/BCAM erythroid expression increased. Lu/BCAM expression was measured by flow cytometry using anti-Lu monoclonal antibody F241. (A-B) SS RBC adhesion as a function of the percentage of RBCs from 12 untreated (UT) and 14 HU-treated patients expressing Lu/BCAM (Lu/BCAM+; A) or of Lu/BCAM MFI (B). (C-D) Lu/BCAM expression level on the surface of RBCs from 19 UT and 19 HU-treated patients represented as the percentage of circulating RBCs expressing Lu/BCAM (C) and the latter's MFI (D). HU increased the percentage of Lu/BCAM-positive RBCs (P < .001) and Lu/BCAM MFI (P < .001; Mann-Whitney test). Horizontal lines represent medians. (E-F) Same as panels C and D for the 5 pre-post group patients before (D0) and during HU treatment (D15, M2, M4, and > M6).
Paradoxically, and as previously reported by Odièvre et al,29 flow cytometry analysis of blood samples from 19 HU group and 19 UT group patients showed that the percentage of Lu/BCAM-expressing cells and the number of Lu/BCAM molecules/RBC were significantly higher for the HU group than the UT group (P < .001; Figure 2C-D); this result was also confirmed for 5 other pre-post group patients who had significantly increased Lu/BCAM expression under HU (Figure 2E-F).
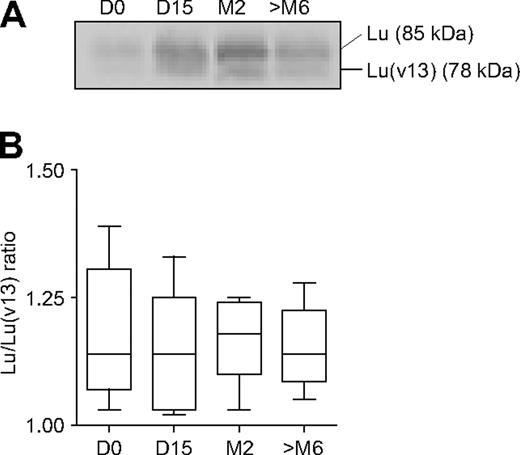
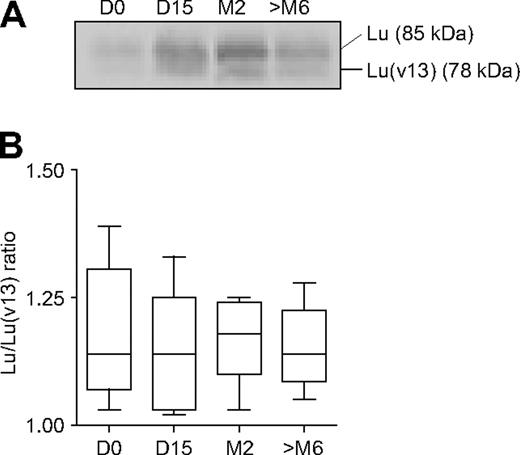
Two Lu/BCAM glycoprotein (gp) isoforms are present on human RBCs, Lu (85 kDa) and Lu(v13) (78 kDa); they result from the alternative splicing of intron 13 and differ by the lengths of their cytoplasmic domains.36,37 Because Lu/BCAM antigens reside on both isoforms, flow cytometry analysis could not show whether one or both of Lu/BCAM isoforms were overexpressed under HU. Therefore, Lu/BCAM gp were immunoprecipitated from SS RBCs of 5 pre-post group patients and revealed by WB (Figure 3A, typical result). After protein quantification, the Lu/Lu(v13) ratio was determined for the 5 patients at all treatment stages (Figure 3B). It showed that Lu was predominantly expressed and that HU did not alter the Lu/Lu(v13) ratio. This finding indicated that Lu/BCAM overexpression under HU was due to an overexpression of both isoforms, suggesting that HU could up-regulate LU gene expression in erythroid cells. In addition, it showed that HU does not modulate the alternative splicing generating Lu and Lu(v13).
Erythroid expression of Lu and Lu(v13) during HU treatment. Lu and Lu(v13) were immunoprecipitated and revealed by WB. (A) Typical result showing the presence of Lu (85 kDa) and Lu(v13) (78 kDa) before and during HU treatment. (B) Box and whiskers represent the Lu/Lu(v13) ratio of 5 pre-post group patients during HU treatment; internal horizontal line, median; lower and upper box limits, 25th and 75th percentiles; and T-bars, range.
Erythroid expression of Lu and Lu(v13) during HU treatment. Lu and Lu(v13) were immunoprecipitated and revealed by WB. (A) Typical result showing the presence of Lu (85 kDa) and Lu(v13) (78 kDa) before and during HU treatment. (B) Box and whiskers represent the Lu/Lu(v13) ratio of 5 pre-post group patients during HU treatment; internal horizontal line, median; lower and upper box limits, 25th and 75th percentiles; and T-bars, range.
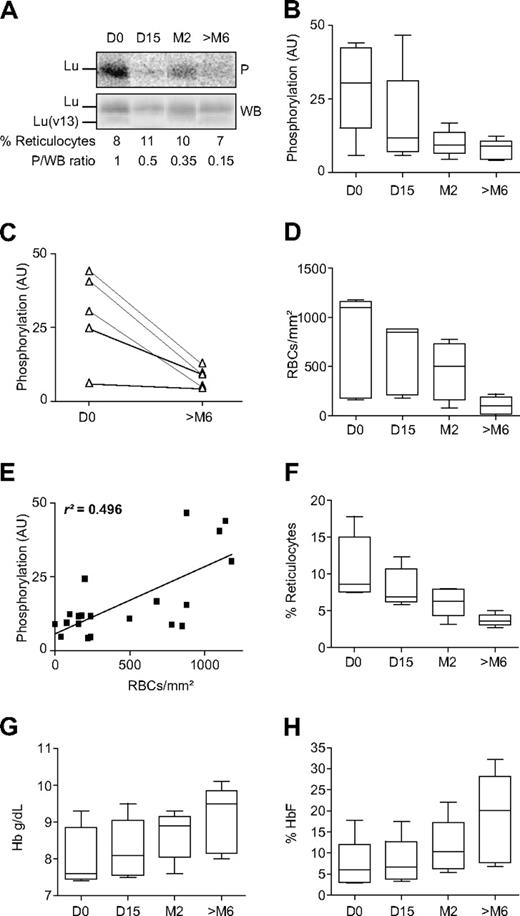
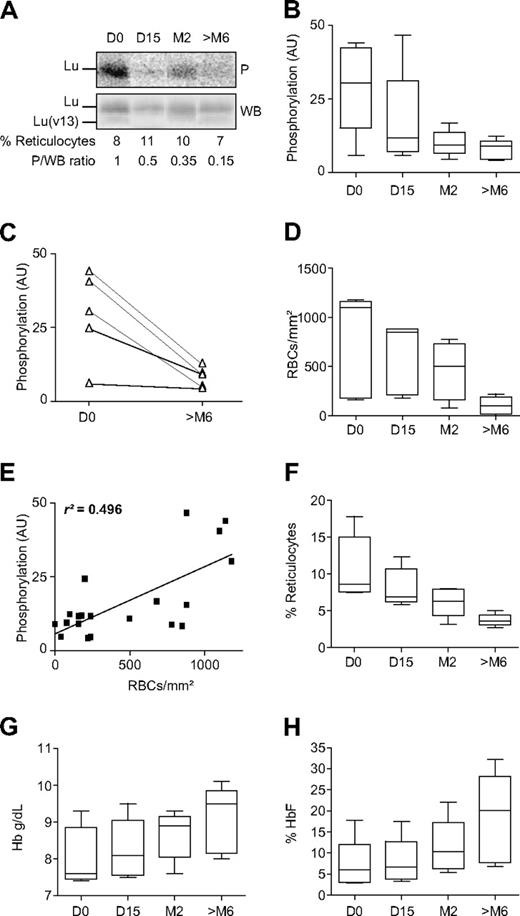
Decreased Lu/BCAM phosphorylation on RBCs under HU
We postulated that HU might reduce SS RBC adhesion by inhibiting Lu/BCAM activation. Lu, but not Lu(v13), is phosphorylated on SS RBCs in a PKA-dependent manner.33 To determine whether HU could modulate phosphorylation of the Lu isoform, radiophospholabeling experiments were performed with RBCs from the pre-post group to assess Lu phosphorylation status in the same person before and during HU treatment. SS RBC samples were obtained from 5 patients before starting HU and at regular intervals during treatment: 15 days, 2, 4, and more than 6 months after starting HU. After RBC radiophospholabeling, Lu/BCAM was immunoprecipitated with F241 mAb, which recognizes the extracellular domain of both isoforms. Phosphorylated (P) Lu-gp was quantified by phosphorImager after sodium dodecyl sulfate-polyacrylamide gel electrophoresis and protein transfer to a nitrocellulose membrane. Total amounts of immunoprecipitated Lu-gp were then quantified on the same membrane by WB. The Lu-gp phosphorylated fraction was estimated by calculating the P/WB ratio of those determinations (Figure 4A, typical result). As expected, both isoforms were expressed on RBCs, but only Lu-gp was phosphorylated (Figure 4A). It is noteworthy that Lu phosphorylation decreased during HU treatment in this patient, although no significant drop was observed for his percentage of circulating reticulocytes (Figure 4A). Decreased Lu-gp phosphorylation was observed after 15 days of HU for 3 patients and within 2 months for the 2 others. This reduction persisted throughout the 6 months of follow-up and was highly significant after 6 months of treatment (P = .005, n = 5 patients; Figure 4B-C). Less phosphorylation was associated with reduced RBC adhesion to laminin (Figure 4D). A linear regression analysis showed a partial correlation between RBC adhesion and Lu/BCAM phosphorylation (Figure 4E, P < .001, r2 = 0.496). Three other parameters known to be modulated by HU were measured. As expected, the percentage of reticulocytes decreased during HU treatment (Figure 4F), whereas the Hb concentration and the percentage of HbF increased (Figure 4G-H).
Lu/BCAM phosphorylation (P), RBC adhesion, and evolution of 3 blood parameters during HU treatment. (A) Typical results (1 of 5 experiments) obtained with pre-post group patient's SS RBCs showing the phosphorylation of the Lu-gp long isoform after RBC radiophospholabeling and immunoprecipitation of Lu/BCAM. The percentage of reticulocytes was determined by flow cytometry of each sample. Total immunoprecipitated Lu/BCAM proteins were quantified by WB. The P/WB ratio estimates the proportion of phosphorylated proteins. (B) Box and whiskers represent Lu/BCAM phosphorylation in 5 patients before (D0) and during HU treatment (D15, M2, and > M6); internal horizontal line, median; lower and upper box limits, 25th and 75th percentiles; and T-bars, range. HU significantly decreased Lu/BCAM phosphorylation (P = .005; Friedman test, AU indicates arbitrary units). (C) Lu/BCAM-phosphorylation change after 6 months of HU treatment for each of the 5 patients. (D) Evolution of RBC adhesion under treatment for the 5 HU-treated patients. (E) A linear-regression analysis between RBC adhesion and Lu/BCAM phosphorylation (P < .001, r2 = 0.496). (F-H) Box and whiskers represent the evolution of reticulocyte percentages, Hb concentrations and HbF percentages, respectively.
Lu/BCAM phosphorylation (P), RBC adhesion, and evolution of 3 blood parameters during HU treatment. (A) Typical results (1 of 5 experiments) obtained with pre-post group patient's SS RBCs showing the phosphorylation of the Lu-gp long isoform after RBC radiophospholabeling and immunoprecipitation of Lu/BCAM. The percentage of reticulocytes was determined by flow cytometry of each sample. Total immunoprecipitated Lu/BCAM proteins were quantified by WB. The P/WB ratio estimates the proportion of phosphorylated proteins. (B) Box and whiskers represent Lu/BCAM phosphorylation in 5 patients before (D0) and during HU treatment (D15, M2, and > M6); internal horizontal line, median; lower and upper box limits, 25th and 75th percentiles; and T-bars, range. HU significantly decreased Lu/BCAM phosphorylation (P = .005; Friedman test, AU indicates arbitrary units). (C) Lu/BCAM-phosphorylation change after 6 months of HU treatment for each of the 5 patients. (D) Evolution of RBC adhesion under treatment for the 5 HU-treated patients. (E) A linear-regression analysis between RBC adhesion and Lu/BCAM phosphorylation (P < .001, r2 = 0.496). (F-H) Box and whiskers represent the evolution of reticulocyte percentages, Hb concentrations and HbF percentages, respectively.
More adhesion to laminin of reticulocytes where Lu/BCAM phosphorylation mainly occurs
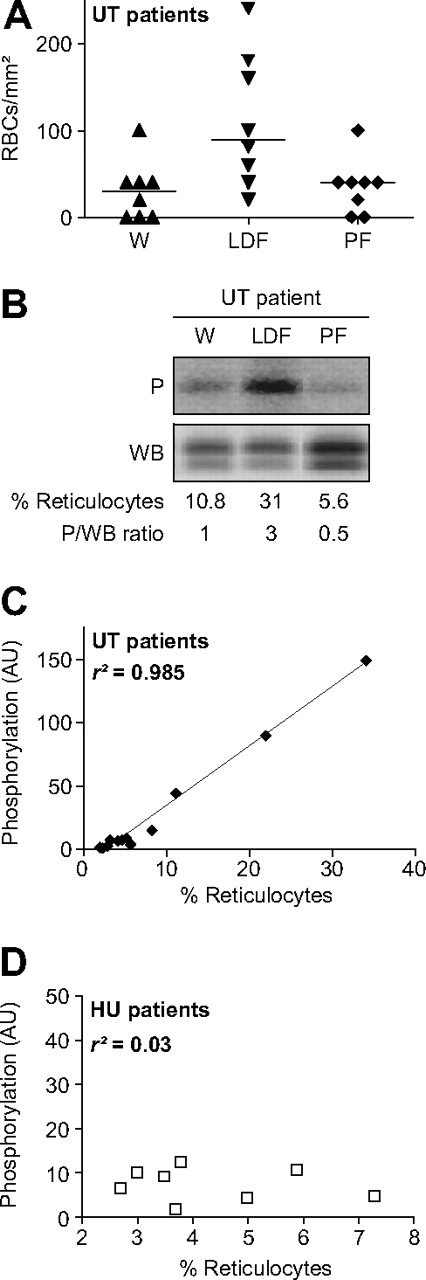
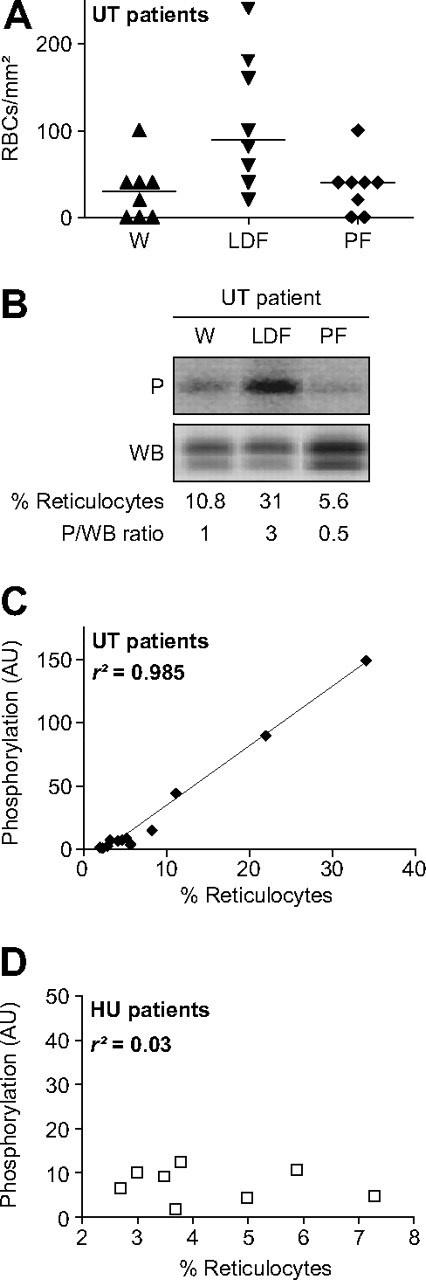
The SCD RBC lifespan is dramatically shortened, and the corresponding reticulocyte count is much higher than in healthy controls. To determine whether the SS reticulocyte percentage could influence RBC adhesion to laminin, flow-adhesion assays were performed with reticulocyte-enriched UT RBCs obtained after whole blood fractionation by Percoll double-density gradient centrifugation. The median percentage of reticulocytes in whole blood (W), the low-density reticulocyte-rich fraction (LDF), and the pellet (reticulocyte-poor fraction, PF) were 8.2, 53, and 4.8, respectively. The LDF exhibited the highest cell-adhesion level, adhering more than cells from whole blood (P < .01) and the pellet (P < .05; Figure 5A). Because Lu/BCAM-mediated cell adhesion to laminin is modulated by phosphorylation, we analyzed Lu-isoform phosphorylation in both fractions and whole blood (Figure 5B). The phosphorylation level (P/WB ratio) was directly correlated to the percentage of reticulocytes (Figure 5C, P < .001, r2 = 0.985, n = 5 patients), indicating that Lu-gp was phosphorylated mainly in young immature RBCs of UT patients.
RBC adhesion to laminin at 0.4 dyne/cm2 and Lu/BCAM phosphorylation (P) after blood fractionation. (A) Adhesion of UT RBCs from whole blood (W), the reticulocyte-rich low-density fraction (LDF), and the pellet containing the mature RBC-rich fraction (PF). Horizontal lines are medians. More LDF cells adhered than those from W (P < .01) or the PF (P < .05; Friedman test). (B) Typical results (1 of 5 experiments) showing the phosphorylation of the Lu-gp long isoform in W, LDF, and PF of an UT patient. The percentage of reticulocytes was determined by flow cytometry for each sample. Total immunoprecipitated Lu/BCAM proteins were quantified by WB. P/WB ratio estimates the proportion of phosphorylated proteins. (C) Linear regression between phosphorylation and reticulocyte percentage in UT patients (r2 = 0.985, P < .001, n = 5 patients, 3 samples for each patient: W, LDF, and PF). (D) Lu/BCAM phosphorylation as a function of the reticulocyte percentage in 8 HU-treated patients (r2 = 0.03, P = .66, n = 8).
RBC adhesion to laminin at 0.4 dyne/cm2 and Lu/BCAM phosphorylation (P) after blood fractionation. (A) Adhesion of UT RBCs from whole blood (W), the reticulocyte-rich low-density fraction (LDF), and the pellet containing the mature RBC-rich fraction (PF). Horizontal lines are medians. More LDF cells adhered than those from W (P < .01) or the PF (P < .05; Friedman test). (B) Typical results (1 of 5 experiments) showing the phosphorylation of the Lu-gp long isoform in W, LDF, and PF of an UT patient. The percentage of reticulocytes was determined by flow cytometry for each sample. Total immunoprecipitated Lu/BCAM proteins were quantified by WB. P/WB ratio estimates the proportion of phosphorylated proteins. (C) Linear regression between phosphorylation and reticulocyte percentage in UT patients (r2 = 0.985, P < .001, n = 5 patients, 3 samples for each patient: W, LDF, and PF). (D) Lu/BCAM phosphorylation as a function of the reticulocyte percentage in 8 HU-treated patients (r2 = 0.03, P = .66, n = 8).
Considering these results, we asked the question whether the decreased Lu/BCAM phosphorylation in HU-treated patients could be a consequence of the HU-driven decrease of circulating reticulocytes. To answer this question, Lu/BCAM phosphorylation levels were determined in RBCs from 8 HU-treated patients and plotted against their percentage of reticulocytes (Figure 5D). As expected, low levels of Lu/BCAM phosphorylation were obtained for all patients. Interestingly, higher reticulocyte count was not associated with higher Lu/BCAM phosphorylation. Figure 5D shows that Lu/BCAM phosphorylation was independent of the reticulocyte percentage of HU-treated patients, indicating that the decrease of Lu/BCAM phosphorylation in HU-treated patients was not a consequence of their decreased reticulocyte count.
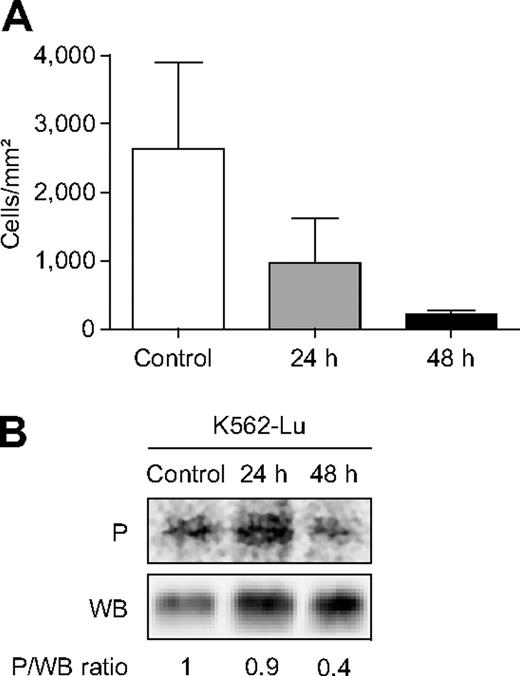
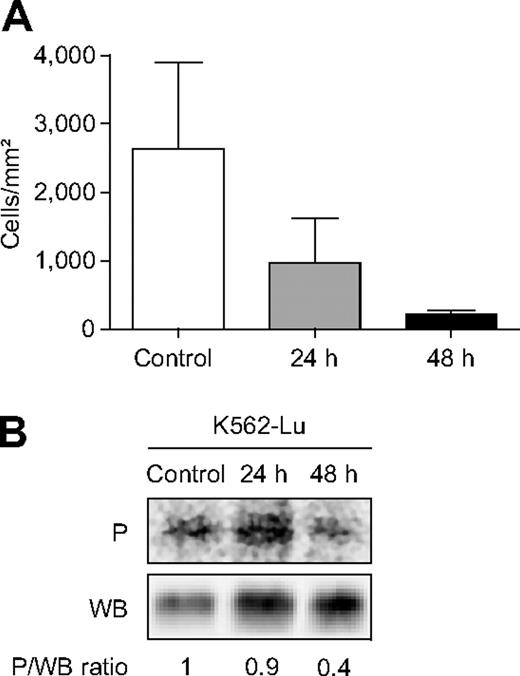
HU exposure leads to less K562-Lu cell adhesion to laminin and less Lu-gp phosphorylation
In an attempt to test the effect of HU on SS RBCs in vitro, RBCs were incubated with or without HU for 24 and 48 hours at 37°C but, unfortunately, severe hemolysis ensued, even in the absence of HU. Therefore, SS RBCs were replaced by a transfected erythroleukemic cell line expressing recombinant Lu-gp, K562-Lu cells. Adhesion and phospholabeling assays were run before and after incubating these cells with HU for 24 and 48 hours. Because HU is cytotoxic, cell viability was monitored by the cell growth curve and flow cytometry using TO-PRO3 iodide. Cell proliferation was slowed down by HU, and cell death was mildly but not sharply induced, as only 2.4% and 4.7% dead cells were detected at 24 and 48 hours, respectively (n = 3). Adhesion at 24 hours was comparable with untreated cells. K562-Lu cell adhesion to laminin was 12-fold lower at 48 hours than untreated control cells (Figure 6A). This difference was not the result of inhibition of Lu-gp expression, as determined by flow cytometry (data not shown). The lower cell adhesion was associated with markedly less Lu-gp phosphorylation of HU-treated cells at 48 hours (Figure 6B), confirming the relationship between the Lu-gp phosphorylation level and cell adhesion and showing that HU could diminish cell adhesion to laminin by modulating Lu-gp phosphorylation.
Adhesion of K562-Lu cells to laminin and Lu-gp phosphorylation (P) during exposure to HU. (A) Data are mean ± SEM values of K562-Lu cells adhering to laminin at 2 dyn/cm2 before (Control) and after 24 and 48 hours of exposure to 250μM HU (n = 3). (B) Lu-gp phosphorylation of HU-treated K562-Lu cells (typical result); data (mean ± SEM) at 24 and 48 hours were 0.75 ± 0.27 and 0.27 ± 0.1, respectively (n = 3). HU exposure reduced K562-Lu adhesion to laminin and Lu-gp phosphorylation.
Adhesion of K562-Lu cells to laminin and Lu-gp phosphorylation (P) during exposure to HU. (A) Data are mean ± SEM values of K562-Lu cells adhering to laminin at 2 dyn/cm2 before (Control) and after 24 and 48 hours of exposure to 250μM HU (n = 3). (B) Lu-gp phosphorylation of HU-treated K562-Lu cells (typical result); data (mean ± SEM) at 24 and 48 hours were 0.75 ± 0.27 and 0.27 ± 0.1, respectively (n = 3). HU exposure reduced K562-Lu adhesion to laminin and Lu-gp phosphorylation.
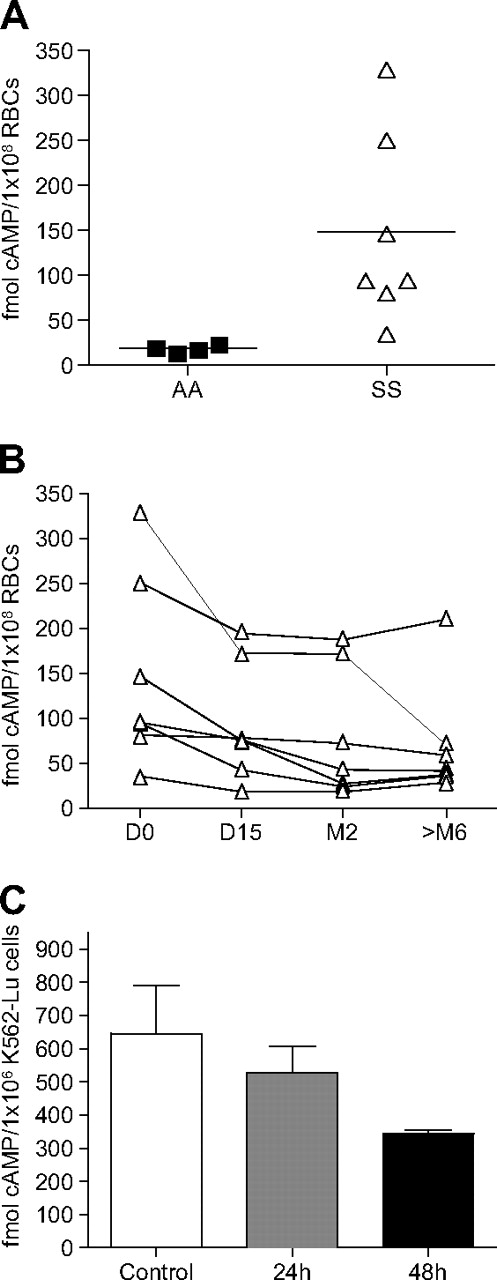
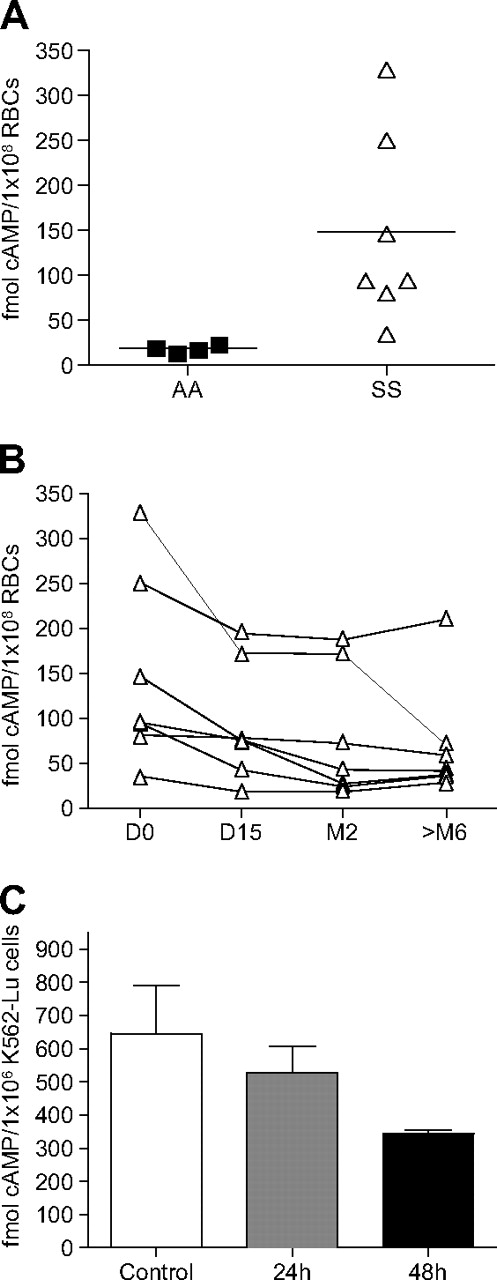
Intracellular levels of cAMP are decreased under HU treatment
Two signaling pathways involved in enhanced Lu/BCAM-mediated SS RBC adhesion to laminin have been described: the PKA30,33 and the Epac/Rap131 pathways. Because cAMP is a common upstream effector of both pathways, its intracellular levels were measured in SS RBCs. We first compared the basal levels of cAMP in SS versus AA RBCs and found higher levels in the former, as previously reported30 (Figure 7A). We then wondered whether cAMP production could be modulated under HU treatment. Intracellular levels of cAMP were determined in RBC samples of 7 pre-post group patients and showed a steady and significant decrease over time (Figure 7B, P = .002). The effect of HU on intracellular cAMP levels was also measured using K562-Lu cells treated for 24 and 48 hours and yielded similar results (Figure 7C). These findings indicated that the lower Lu/BCAM phosphorylation under HU could be a direct consequence of a diminished stimulation of PKA and/or Epac/Rap1 pathways.
Quantification of intracellular cAMP in RBCs and K562-Lu cells. cAMP levels were measured using an enzyme immunoassay. (A) cAMP levels in 4 AA and 7 SS RBC samples. Each dot represents the measured cAMP value in 108 RBCs from one patient. The horizontal lines are medians. (B) cAMP values measured in 7 patients during HU treatment at D0, D15, M2, and more than M6. The decrease in cAMP levels was significant (P = .002; Friedman test). (C) Decreased cAMP values measured in K562-Lu cells incubated with HU for 24 and 48 hours.
Quantification of intracellular cAMP in RBCs and K562-Lu cells. cAMP levels were measured using an enzyme immunoassay. (A) cAMP levels in 4 AA and 7 SS RBC samples. Each dot represents the measured cAMP value in 108 RBCs from one patient. The horizontal lines are medians. (B) cAMP values measured in 7 patients during HU treatment at D0, D15, M2, and more than M6. The decrease in cAMP levels was significant (P = .002; Friedman test). (C) Decreased cAMP values measured in K562-Lu cells incubated with HU for 24 and 48 hours.
Discussion
The pathophysiology of SCD is complex and not fully understood. The first step in the sickling process is HbS polymerization; hence, factors delaying reoxygenation of the HbS deoxygenated form or increasing the intracellular HbS concentration are thought to play major roles in initiating and accelerating the sickling process, consequently promoting the blockade of the microcirculation.38 RBC adhesion to the vascular wall probably favors the formation of HbS polymers by slowing the flow of cells circulating through capillaries, thereby leading to the next step, which is vaso-occlusion. Many observations support an important role of abnormal cell adhesion in the obstruction of microvessels or in facilitating the trapping of sickle cells in postcapillary venules.5-7 We focused our study on Lu/BCAM, as they are the unique erythroid receptors of laminin, a major ECM protein, and are expressed in young and mature RBCs, unlike CD36 and integrin α4β1, which are restricted to reticulocytes. Considering the important interindividual heterogeneity in SCD and the variability of RBC characteristics during VOC,39 we applied strict patient inclusion criteria to minimize potential biases (“Patients and blood samples”).
Hillery et al provided the first evidence that HU decreased SS RBC adhesion to TSP and laminin, but too few patients were studied to draw conclusions regarding potential correlations between RBC adhesion and the clinical response.28 Because HU modulates the expression of several genes, up-regulating HbF and down-regulating adhesion molecules CD36 and α4β1,22,23,29 it could be expected that less adhesion to laminin resulted from less Lu/BCAM. Paradoxically, the findings of Odièvre et al did not support that hypothesis, as they showed that HU enhanced erythroid Lu/BCAM expression in children.29 Thus, SS RBC adhesion to laminin does not reflect the Lu/BCAM-expression level on the cell surface.
Herein, we confirmed that HU significantly increased erythroid Lu/BCAM expression by enhancing both the percentage of Lu/BCAM-positive RBCs and the numbers of Lu/BCAM copies/RBC. We showed that HU did not modulate the alternative splicing generating Lu and Lu(v13) isoforms but rather up-regulated erythroid expression of the LU gene. As expected, HU increased the Hb concentration and HbF percentage. Pertinently, the lower cell adhesion and Lu/BCAM phosphorylation preceded the HbF rise. Moreover, we showed that the reduced RBC adhesion to laminin under HU was associated with dramatically decreased Lu/BCAM long-isoform phosphorylation, despite its enhanced expression, clearly demonstrated for the pre-post group patients. This decreased phosphorylation was most probably a direct consequence of the diminished intracellular cAMP levels measured in these patients during HU treatment. Thus, HU could modulate PKA and/or Epac/Rap1 pathways, downstream of cAMP, and inhibit Lu/BCAM phosphorylation. As intracellular cAMP levels are controlled by several effectors, including adenylyl cyclase and phosphodiesterases, further studies are needed to fully characterize the HU mechanism of action in SCD. Our finding agrees with the results of other studies describing the role of HU in regulating cellular functions via signaling pathways. Some observations suggested that HU might raise nitric oxide levels by stimulating vascular endothelial cell production of it via the eNOS-cGMP pathway.40-43 HU could also prevent neutrophil activation and adhesion to fibronectin in a cAMP-PKA–dependent manner.44,45 The in vivo effect of HU on Lu/BCAM long-isoform phosphorylation and cAMP decrease could not be tested ex vivo using SS RBCs because of hemolysis. Nevertheless, using human erythroleukemic K562-Lu cells expressing recombinant Lu-gp, we showed that the ex vivo effects of HU were similar to those observed for SS RBCs from HU-treated SCD patients. Although the K562 cell line derives from an erythroid lineage, it could not be compared with RBCs. Nevertheless, these experiments revealed that HU could negatively impact cAMP levels, Lu/BCAM phosphorylation, and cell adhesion to laminin in this cell line, suggesting that it could help deciphering the HU mechanism of action.
Another new finding was the correlation between Lu-gp phosphorylation and the percentage of reticulocytes in UT patients, which could explain why their reticulocyte-enriched fractions adhered more to laminin than mature RBCs. Two studies investigated SS RBC adhesion to laminin according to their density and reported that cells from the dense fraction were the most adherent.46,47 Our results were obtained using a different experimental approach to have reticulocyte-enriched fractions. The 5% to 10% of very dense and irreversibly sickled cells, reported to be the most adherent,46,47 were diluted in our pellet fraction with cells of intermediate density known to be much less adherent. We chose to focus on reticulocytes because no Lu/BCAM phosphorylation was detected in mature dense RBCs, and our objective was to determine the effect of HU on Lu/BCAM activation through the phosphorylation of the long Lu isoform. Our results showed that, contrary to what was observed for UT patients, the Lu/BCAM phosphorylation level was independent of the reticulocyte count in HU-treated patients, as patients with less than 3% and more than 7% of reticulocytes showed similar phosphorylation levels (Figure 5D). We showed that the HU effect on RBC adhesion preceded the reticulocyte count decline. Pre-post group RBC adhesion to laminin was often diminished before the reticulocyte count changed significantly, revealing a qualitative modification of the adhesive properties of circulating reticulocytes. This was clearly demonstrated for the patient in Figure 4A who showed a dramatic decrease of Lu/BCAM phosphorylation after more than 6 months of HU therapy, although no significant change was observed for his percentage of circulating reticulocytes. In addition, the reticulocyte count diminution under HU in the 5 pre-post group patients was not statistically significant (P = .26). Nevertheless, because the phosphorylation level results from the balance between kinase and phosphatase activities, and the RBC stock of kinases declines with age, it cannot be excluded that the prolongation of RBC survival under HU could partially contribute to the reduced Lu/BCAM phosphorylation.
In addition to phosphorylation, Lu/BCAM-mediated cell adhesion to laminin is regulated by the interaction of the Lu/BCAM cytoplasmic domain with the spectrin-based skeleton.48-50 Loss of interaction with spectrin increases Lu/BCAM-mediated cell adhesion to laminin.48,49 Because HbS polymerization during sickling generates skeleton disorganization, it could negatively affect the Lu/BCAM-spectrin interaction, of both Lu and Lu(v13) isoforms, and lead to enhanced adhesion of sickled RBCs, independently of phosphorylation events. This scenario could account for the partial correlation between phosphorylation and adhesion in our experiments (r2 = 0.496) and for the previously reported high adhesion of very dense, irreversibly sickled cells.46,47 Several RBC skeletal proteins undergo phosphorylation, which regulates their interactions with other cytoplasmic proteins. Our results showed an HU impact on phosphorylation events in RBCs; thus, it could modulate protein-protein interactions. Further studies are needed to investigate the role of the Lu/BCAM-spectrin interaction in SS RBC adhesion to laminin and the effect of HU on it.
Altogether, our results strongly suggest a critical role for HU in inhibiting Lu-gp phosphorylation, which was associated with significantly less SS RBC adhesion to laminin. It is widely accepted that HU reduces SS RBC adhesion by down-regulating the reticulocyte count and the expression levels of adhesion molecules. Our findings show, for the first time, that HU could also play a role in reducing receptor-ligand interactions, most probably by modulating their affinity, which could explain the very short duration of HU pharmacologic activity, independent of its reconditioned RBC renewal wave.
In conclusion, the results of our study reveal a new HU mechanism of action in regulating SS RBC adhesion by modulating the phosphorylation state of an adhesion molecule independently of its expression level. Future investigations should help characterize the pathway leading to this HU-induced modulation, which could give rise to new therapeutic perspectives.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank Centre National de Référence sur les Groupes Sanguins for the storage and management of blood samples.
This work was supported by Institut National de la Transfusion Sanguine, Inserm, Agence Nationale de la Recherche (SCADHESION 2007), Région Île-de-France (SESAME 2007 no. F-08-1104/R), and Société Française de Médecine Interne and Actélion (fellowship “maladies rares”).
Authorship
Contribution: P.B. designed and performed research, analyzed data, and wrote the paper; V.C. designed and ran experiments and commented on the manuscript; J.P. designed and performed cytometry experiments and commented on the manuscript; D.B., A.H., C.F., and F.G. collected blood samples and provided patients' clinical data; Y.C. and C.L.V.K. discussed the results, gave advice, and commented on the manuscript at all stages; and W.E.N. supervised the project, designed and performed research, and wrote the paper.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Wassim El Nemer, Inserm, UMRS 665, Institut National de la Transfusion Sanguine, 6, rue Alexandre Cabanel, 75015 Paris, France; e-mail: wassim.el-nemer@inserm.fr.