Abstract
Abstract 1077
Studies focused on elderly APL are limited. The European APL study group reported in their APL 93 trial that lower survival rate in elderly APL was mainly due to an increase of early deaths and toxicity of chemotherapy (Ades et al, 2005). On the other hand, PETHEMA group reported in their LPA96 and 99 studies that ATRA combined with anthracycline monochemotherapy resulted in low toxicity and high compliance, and that survival rate is similar to younger patients (Miguel A et al, 2004). We analyzed clinical features and outcomes of elderly APL patients with APL who were treated with ATRA and intensive chemotherapy and compared with those of younger patients in long term follow-up of the JALSG-APL97 Study.
Patients with newly diagnosed APL were continuously registered from May 1997 to June 2002, and induction therapy was composed of ATRA and chemotherapy including idarubicin and cytarabine. The dose and duration of chemotherapy were based on initial leukocyte count. After completion of 3 courses of consolidation chemotherapy, patients negative for the PML-RARA transcript were randomly allocated either to receive 6 courses of intensified maintenance chemotherapy or to observation. Elderly patients were treated with the same schedule to younger patients (Asou et al, 2007). Clinical features as well as relapse rate (RR), overall survival (OS) and disease-free survival (DFS) were assessed in elderly group with aged 60 or more in comparison with younger group. Clinical outcomes were updated on January, 2009 and the median follow up period is 7.3 years.
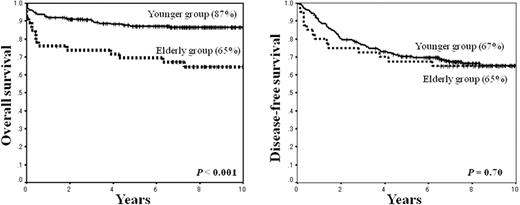
Of 302 patients registered in this study, 283 patients were assessable. The median age was 48 years (range, 15–70 years), with 237 patients in younger group (median age, 44 years) and 46 patients in elder group (median age, 63 years). Significantly lower platelet count (less than 10 × 109/L), higher incidence of ECOG performance status 3 to 4, lower albumin level (< 3.5g/dl) were observed in elderly group compared to younger group (P = 0.04, P = 0.02 and P < 0.001, respectively), while clinical characteristics including gender, initial leukocyte count, APL cells in peripheral blood, DIC score, frequency of variant type (M3v), expression of CD-phenotype, past history of chemotherapy and/or radiotherapy and number of infectious complications at diagnosis, did not differ between two groups. The CR rates and early mortality during induction therapy including to hemorrhagic complications were similar between two groups (89% vs. 96%, P = 0.06; 11% vs. 4%, P = 0.08), whereas induction death due to differentiation syndrome in elderly group is higher compared with younger group (4% vs. 0%, P = 0.03). The cumulative incidence of non relapse mortality (NRM) during the third consolidation chemotherapy was significantly higher in elderly group (9% vs. 1%., P = 0.04). All of the mortality occurred during consolidation therapy was associated with infection. Although OS was lower in elderly groups at 10 year compared with younger group (65% vs. 87%, P < 0.001), DFS and RR were similar between two groups (65% vs. 67%, P = 0.70; 13% vs. 26%, P = 0.15, respectively).
The present study demonstrated that efficacy of ATRA combined with chemotherapy in elderly APL was similar to younger APL. Nevertheless, lower OS at 10 year in elderly APL was observed in this study. One of the reasons was an increase of NRM, especially induction death due to differentiation syndrome and infection death during consolidation chemotherapy. Thus, reduction of intensity of post remission chemotherapy should be considered in elderly patients. Non-myelosuppressive agents such as arsenic trioxide and/or tamibarotene should be incorporated into the post remission therapy for elderly patients with APL.
No relevant conflicts of interest to declare.

This icon denotes an abstract that is clinically relevant.
Author notes
Asterisk with author names denotes non-ASH members.