Abstract
Abstract 1281
Cytomegalovirus (CMV) end-organ disease is a serious complication after allogeneic stem cell transplantation (Allo-SCT). The quality of the post-transplant immune reconstitution plays a crucial role in the development of both, post-transplant infections and relapse of the underlying disease, two of the main factors conditioning post-transplant mortality and hence final survival. The relationship between viral replication and CMV specific immune reconstitution has not been completely unveiled. This knowledge would allow identifying patients at risk for developing CMV disease and eventually improving their clinical management.
to analyze the relationship between CMV replication and specific CMV immune reconstitution and the potential influence of this relationship in main clinical outcomes.
A prospective study of consecutive recipients of Allo-SCT was performed from June 2008 through December 2009 at a single institution. Blood samples were collected from one week before transplant, weekly during the first three months after transplant, every other week from month three to six and monthly from month seven to complete one year of follow up. CMV viral load was determined by real time PCR and CMV-specific T cell response was determined by flow cytometry with surface markers and intracellular cytokine staining. The percentage of activated CD4+, CD8+ and CD3+ T cells expressing CD69 were considered positive when IFN-’Y cytokine secretion was over 0.25%. Chimerism of the isolated CD8+ T cell subpopulation was determined by PCR. CD69 expression and cytokine secretion were compared in both CD4+ and CD8+ T cells between the different time points and both subsets of patients by the Wilcoxon test. CMV viral load reduction without treatment administration was compared by Wilcoxon test. Differences were considered statistically significant for p-values < 0.05. All statistical analyses were performed using SPSS 16.0 software (Chicago, IL).
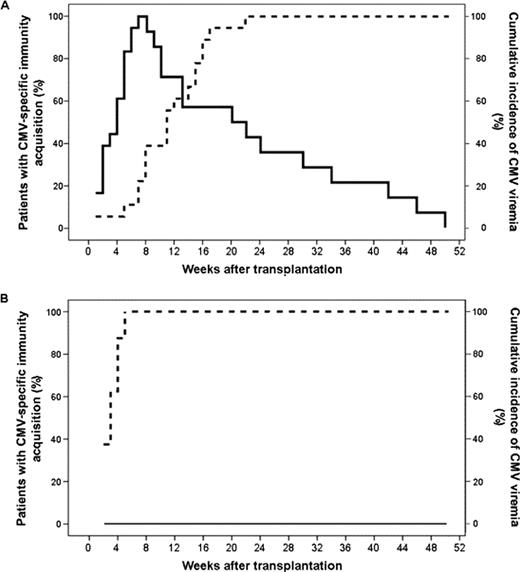
Twenty-six patients were enrolled in the study with a median age of 33 years (range:15-61). We identified two groups of patients. A first group of 18 (69.2%) patients developed CMV infection and acquired CMV-specific T cell response by median week 8 (range:1-22; Figure 1A). The decline in the incidence of CMV replication episodes correlated with the acquisition of CMV-specific T cell response (Linear regresion r2=0.781, Pearson correlation p=0.01). A second group of 8 patients (30.8%) never developed CMV infection after the transplant, with a median value of 2 weeks (range:1-7; Figure 1B). The time of the acquisition of CMV-specific T cell response for the group with viremia and for the non-viremic group (week 2 vs. week 8) was statistically different (p= 0.01). Fifteen per cent of the patients (n=4) developed end-organ disease. Three out of five patients with end-organ disease developed replication CMV episodes over 10,000 copies/ml, while only 1 out of 13 patients with no end-organ disease developed viral loads under 10,000 copies/ml (p=0.04). The percentage of positive CD8+ T cells expressing IFN-γ in the patients that developed disease tended to be lower than in the patients that did not develop disease (median percentage of IFN-g positive CD8 T cells 0.3 vs. 0.5, respectively). The chimerism of the CD8+ T cells subpopulation after acquiring the specific immune response was of complete donor origin for all the patients.
Developing donor-derived T-cell mediated CMV-specific immune response within the following two weeks after the transplant is inversely associated with the development CMV infection. The level of CMV viral load may predict end-organ disease. The use of a tool to determine T-cell mediated CMV-specific immune response in the clinical practice may help to improve the management of these patients, avoiding unnecessary treatments, and predicting clinical outcomes.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.